Chronic venous insufficiency: the role of venous obstruction and treatment options
Abnormal venous reflux caused by venous incompetence has been the dominant concept in chronic venous insufficiency; however, the pivotal role of iliac venous obstructive lesions is now well recognised. Greater consideration should be given to investigating obstructive lesions when treating patients with venous ulcers, recurrent venous thrombosis and unresolved venous disease such as pelvic congestion syndrome.
- Venous disease contributes considerably to the burden of disease for patients and healthcare services but is under-researched and undertreated.
- Venous obstruction has been a largely neglected cause of chronic venous disease and remains underdiagnosed.
- Patients presenting with severe symptoms of chronic venous insufficiency or a history of thrombosis should be evaluated with a thorough history, physical examination and detailed lower-extremity venous duplex scans, and referred to a vascular specialist to rule out iliac venous obstructive lesions.
- Percutaneous balloon angioplasty and stenting appear to be a safe and effective treatment for venous obstruction, with significant clinical resolution of symptoms, prevention of recurrence of thrombosis and ulceration and acceptable long-term patency.
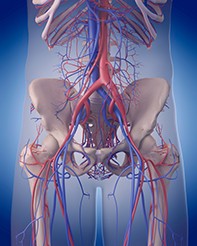
Picture credit: © Sebastian Kaulitzki/Shutterstock
Chronic venous insufficiency (CVI) is a condition affecting the lower limbs that is characterised by persistent ambulatory venous hypertension causing problems such as pain, oedema, skin changes and ulceration. Although the term CVI is often used to imply the more advanced manifestations of chronic venous disease, it is considered by vascular surgeons to include the full spectrum of this disease.1 This ranges from varicose veins, which involve incompetent valves and increased venous pressure, to hyperpigmentation, venous eczema, lipodermatosclerosis, atrophie blanche and healed or active ulcers.
CVI has a high prevalence and considerable socioeconomic impact, so an understanding of its clinical manifestations, diagnostic modalities and new therapeutic options is warranted. This article reviews clinical aspects of CVI, focusing on the diagnostic and therapeutic options for venous obstruction, as most of the available literature focuses on venous incompetence.
Relevance
CVI is important because of the number of people affected and the socioeconomic impact of its more severe manifestations. It is a common problem that affects people psychologically, as patients with CVI often develop depression and anxiety, as well as clinically.2
Although there are no data on the prevalence of CVI in the Australian population, the prevalence of varicose veins in countries with a similar ethnic composition ranges from 6.8 to 39.7% in men and 24.6 to 39.0% in women.3 Data from Medicare Australia suggest that the largest group of patients requiring treatment for varicose veins is women between the ages of 35 and 64 years.3
Because of the dynamic and recurrent nature of venous disease, most vein conditions are long term and often require multiple treatments. A study evaluating more than 91,000 patients in various geographic regions found that clinically significant chronic venous disease was present in about 60% of the population worldwide.4 Approximately 20% of all patients with CVI will develop venous ulcers, and active or healed ulcers are present in about 1% of the adult population.5-9
Delayed healing and a high rate of recurrent ulceration mean that the overall prognosis of venous ulcers is poor. Recurrence rates have been shown to be 50 to 76%, and an Australian study showed the point prevalence of leg ulcers to be 0.1%.1,5,10
The socioeconomic impact of venous ulceration is multifactorial. Disability related to venous ulcers leads to the loss of productive work hours, with an estimated two million workdays lost per year in the USA.1 It can also lead to early retirement, which has been found to occur in more than 12% of workers with venous ulcers.1,6
On top of this, the financial burden of venous ulcer disease on the healthcare system is estimated to be 1 to 2% of the total healthcare budget. This means that the annual cost of venous ulcer care in Australia is about A$3 billion.5,8 In Australia, the care of patients with venous ulcers has now partly shifted from the acute care sector into the community, where wound care services and products are not fully subsidised by the government. A pilot study in 2010 indicated that the average expenses incurred by people with CVI in the process of managing their venous leg ulcers was A$114 per month. This result was concerning, considering the average weekly income from the aged pension was A$206, indicating that about 13% of total weekly income was being spent on treatment and management of leg ulcers.11
Pathophysiology
The proper functioning of the venous system depends on patency of the vessels, one-way valves and muscle pumps. In the erect position, blood that enters the lower-extremity venous system must travel against gravity to return to the central circulation. Contraction of the muscle pumps, primarily in the calf, forces blood up the deep venous system. The valves prevent blood from being forced more distally within the deep venous system or through perforator veins into the superficial system.
Immediately after ambulation, the pressure within the veins of the lower extremities is normally low because the venous system has been emptied by the muscle pump action. With prolonged standing, the veins become distended as they fill via antegrade flow, allowing the valves to open and pressure to increase.
Venous disease develops when venous pressure is increased and the return of blood is impaired.12 This may result from valvular incompetence, venous obstruction or a combination of these mechanisms.
Lower-limb venous pressure changes depend on ambulation, rest and standing position. In a person with normal venous function, the resting standing venous pressure is about 80 to 90 mmHg. The pressure decreases by more than 50% with calf exercise, dropping to 20 to 30 mmHg, and the return to resting pressure is gradual, with refill taking more than 20 seconds. If abnormal venous reflux is present (in patients with valve incompetence) then the resting standing pressure is usually higher than normal and the decrease in pressure with calf exercise is blunted (less than 50% decrease). There is also a faster return in venous pressure to the resting level because of the short refill time (less than 20 seconds). In patients with venous obstruction, the resting standing venous pressure is again higher than normal, but there is minimal to no drop in pressure with calf exercise (Figure 1).1 This means that patients with venous obstruction do not benefit from exercise as patients with venous reflux do.
Venous obstruction and pelvic vein insufficiency
Venous outflow obstruction has been largely neglected as a cause of chronic venous disease, partly because valve incompetence and venous reflux were the focus of attention and partly because treatment options were limited to invasive surgical techniques, such as bypass grafting, with limited patency rates. Over the past two decades, however, minimally invasive treatment options have gained popularity, mainly through improvements in endovascular technology.
Venous obstruction may result from an intrinsic venous process, such as chronic deep vein thrombosis, or from extrinsic compression. May–Thurner syndrome, also known as Cockett’s syndrome or iliac vein compression syndrome, is most often described as compression of the left common iliac vein between the right common iliac artery and the lumbar vertebrae, which causes the development of fibrosis (much like scar tissue) inside the vein.13 This leads to progressive stenosis and the development of venous disease symptoms. The pelvic veins can also be compressed at other points by other segments of artery or by overlying structures such as an enlarged uterus or a tumour.
Venous outflow obstruction plays a significant role in the pathogenesis of CVI.14 Venous obstruction, as well as deep vein valve dysfunction, is associated with a high rate of venous ulceration (Figures 2a and b) and more rapid progression of disease than in superficial venous valve incompetence. A study of intravascular ultrasound examinations found that iliac vein obstructive lesions were present in 938 limbs of 879 patients with severe symptoms of CVI; 53% of the limbs had nonthrombotic iliac vein lesions, 40% were post-thrombotic and 7% were a combination.15
Despite a high incidence in the general population, venous obstruction is often asymptomatic and remains underdiagnosed. It has been suggested that iliac vein lesions act as permissive lesions, and it is the addition of factors such as trauma, cellulitis, distal thrombosis, lymphatic exhaustion or reflux that renders the extremity symptomatic.15 In the elderly, atherosclerosis of the overlying artery, venosclerosis, decreasing mobility and leg dependency or other comorbid conditions predisposing to pedal oedema may be contributory factors in symptom expression. In some cases, no secondary aggravating factors are apparent, and symptom expression may simply be related to further progression of the stenotic lesion.16
Clinical manifestations
CVI represents a spectrum of conditions ranging from simple telangiectasia or reticular veins to more advanced stages, such as skin fibrosis and venous ulceration. The same clinical manifestations may result from different pathogenic mechanisms, including incompetent valves, venous obstruction, muscle pump dysfunction or a combination of these. Some patients whose iliac veins are narrowed by 50% or more will develop one or more symptoms. The symptoms are caused by high pressure in the veins resulting from the obstruction and the enlargement of other veins to carry blood flow around the obstruction and back to the heart.
Iliac vein thrombosis secondary to an obstructive lesion is well recognised and thought to occur in 18 to 69% of patients with lower-extremity deep vein thrombosis.17 Patients who have compression or stenosis of an iliac vein may be more prone to developing thrombosis if they also have other risk factors for clotting, such as use of oral contraceptives or oestrogen therapy, pregnancy, extended sedentary periods or inherited disorders that increase the risk of abnormal clotting (e.g. factor V Leiden mutation, factor II prothrombin mutation, protein S or protein C deficiency or antithrombin III deficiency).
Varicose veins in the abdomen or groin that appear distended even in the supine position or that are present in nonsaphenous territories are highly indicative of a pelvic source (Figure 3). Orthostatic limb pain or pain after exercise (claudication type pain) in the younger population (aged under 30 years) should raise suspicion of pelvic vein obstruction.18 Exercise-induced pain usually occurs in the thigh and occasionally the calf muscles. Such venous claudication, described by patients as a bursting sensation or throbbing/pressure type of pain, is relieved by rest and elevation of the legs. A syndrome of spinal claudication caused by spinal compression by venous collaterals has also been described.19
Severe leg swelling, particularly when affecting the thigh, should also suggest a pelvic source. Pelvic pain, lower back pain or urinary bladder discomfort are common findings in patients with iliac vein obstructive lesions and pelvic vein insufficiency. Patients often present with unilateral or bilateral lower abdominal or pelvic pain, which is generally chronic and dull, although acute and severe pain may occur. The pain, described as heaviness and fullness in the lower pelvis, thighs and vulvar region or scrotum, is exacerbated in women during menses and may be associated with postcoital ache, dyspareunia, perineal pain, urinary urgency and atypical varicosities, such as pudendal, vulvar and perilabial veins and varicoceles.20 Incompetent veins can also collateralise along the posterolateral thigh and gluteal regions.21
Patients with venous obstruction can experience bleeding from high-pressure varicosities, and the venous congestion occasionally results in hyperhidrosis and significant fluid loss through the skin. Skin changes can include pigmentation caused by haemosiderin deposition and eczematous dermatitis.16 Lipodermatosclerosis is a fibrotic process that may occur in the dermis and subcutaneous fat. There is an increased risk of cellulitis, leg ulceration and delayed wound healing in patients with venous obstruction. In addition, protracted CVI may contribute to the development of lymphoedema, representing a combined process.
Depression and anxiety are common comorbidities in patients with venous obstruction, often owing to a prolonged time to diagnosis, and these comorbidities may also have a physiological cause. In response to the shearing and stretching of the congested pelvic veins, endothelial and smooth-muscle cells release vasodilator substances, which play a key role in regulating emotions and stress.22
As the symptoms of venous obstruction progress slowly over many years, patients often adapt their lifestyles accordingly and do not seek medical attention until symptoms become severe. Many patients have reported unknowingly decreasing their level of physical activity as the symptoms worsened, attributing them to being part of the normal ageing process.
Diagnosis of venous obstruction
Investigation of patients with suspected venous insufficiency begins with a thorough history and physical examination, followed by a detailed lower-extremity venous duplex scan to evaluate obstruction and valvular incompetence of both deep and superficial venous systems.
The appropriate diagnosis of venous obstruction requires a high degree of suspicion and a low threshold for extending investigations beyond duplex ultrasound evaluation of the lower extremity. Pelvic imaging (transabdominal duplex, computed tomography or magnetic resonance imaging) should be obtained to exclude malignancy, benign tumours, retroperitoneal fibrosis and other aetiologies.
The diagnosis of venous outflow obstruction largely depends on anatomical rather than haemodynamic criteria. Transfemoral venography is the standard method of imaging the venous outflow tract and may disclose the site of obstruction (Figure 4). However, intravascular ultrasound is superior to venography in estimating the morphological degree and extent of iliac vein stenosis and visualising details of intraluminal lesions.23
Patients should be referred to a vascular specialist for further investigation if they:
- have a previous history of deep or superficial vein thrombosis (especially if it is recurrent or unprovoked)
- have venous ulceration
- have a lower-limb venous duplex scan that has indicated a pelvic source for their varicosities
- are young and complaining of leg claudication
- have severe oedema (especially if affecting the thigh)
- have pelvic congestion symptoms
- have vulvar varicosities or varicoceles.
It is important to note that patients may present with one or a combination of these symptoms.
Treatment of venous obstruction
Conservative management methods traditionally used for CVI, such as gradual compression stockings and exercise, are usually not beneficial in treating venous obstruction and often cause the patient increased discomfort and pain. Percutaneous venous balloon angioplasty and stenting is emerging as a safe and effective alternative to traditional open surgery (Figures 5a to c).
The mortality rate after endovenous stenting is nil and the morbidity rate is less than 1%.24 In a review of multiple reports involving about 1500 patients, patency was found to be 90 to 100% for nonthrombotic disease and 74 to 89% for post-thrombotic disease at three to five years.25 The clinical efficacy of iliofemoral venous stenting is supported by reports of significant relief of pain and swelling and high rates of ulcer healing. Objectively documented swelling is completely relieved in about a third of limbs and significantly reduced in others, and about half of patients have complete relief of pain after stenting.24 Despite the presence of untreated reflux in many limbs, about half of ulcerated legs will heal, and remain healed for up to two years, after iliac vein stent placement.17,24,25
A recent study of 220 women treated for pelvic congestion syndrome found that 82% of those with pelvic venous reflux had an iliac vein obstruction. The authors concluded that in patients with iliac vein obstructive lesions and ovarian incompetence, the iliac vein lesion should be treated first, and ovarian reflux should only be treated if symptoms persist.26
Conclusion
The pivotal role of iliac venous obstructive lesions in the development of CVI and thrombosis is now well recognised. Patients presenting with severe symptoms of CVI or a history of thrombosis should be thoroughly evaluated. Percutaneous balloon angioplasty and stenting appear to be a safe and effective treatment for venous obstruction, with significant clinical resolution of symptoms, prevention of recurrence of thrombosis and ulceration and acceptable long-term patency. MT
Acknowledgement
The author wishes to thank Ms Kate Dwight, Vascular Care Centre, Wollongong, NSW, for her contribution to this article.