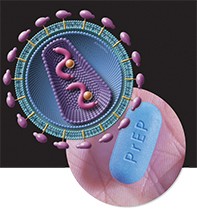
Are you PrEPared for the end of HIV in Australia?
Pre-exposure prophylaxis (PrEP) for HIV has good efficacy data and strong global support for implementation and national support from sexual health physicians and LGBTIQ advocacy groups.
The HIV epidemic currently affects 36.1 million people worldwide.1 There are 21,000 people who live with HIV infection in Australia with annual new infection rates of 1200 per year, most of whom are men who have sex with men (MSM).1 People living with HIV infection have a greatly improved life expectancy, nearing that of the general population, but those infected with HIV still continue to require lifelong medication and management.
In the past few years, randomised clinical trials have focused on a strategy where individuals who are not infected with HIV, but are at high risk of exposure, take antiretroviral medications to prevent themselves from acquiring the infection.2-7 Results of these trials have been impressive and this strategy is called pre-exposure prophylaxis (PrEP). PrEP is a new HIV prevention tool and it is important to be aware of this option when advising MSM or other population groups attending for sexual health checks who are at risk for HIV infection.
What is PrEP?
PrEP is licensed for use in Australia by HIV-negative adults who are at high risk of HIV acquisition. Oral antiviral medication, namely coformulated tenofovir disoproxil fumarate and emtricitabine, is used for PrEP and is marketed as Truvada; however, it is not available on the PBS for PrEP. (It is PBS listed for use in HIV- and hepatitis B-infected patients.) Many patients within Australia and globally access generic versions of the drug through online pharmacies after consultation with a prescriber. PrEP is recommended for daily use during periods where the patient is at risk of acquiring HIV infection, such as when having regular, condomless anal sex with partners of unknown HIV status.
I am confused: is this not PEP?
Post-exposure prophylaxis (PEP) is another intervention to prevent HIV infection. An individual takes a four-week oral course of HIV antiretroviral medication within 72 hours of a high-risk exposure with someone of unknown HIV status from a high-risk group.8 This regimen can be used to prevent HIV infection after occupational needlestick injuries or sexual exposure risk. PEP has been available in Australia since the late 1990s from S100 prescribers, hospitals and emergency departments.
Who is at high risk for HIV infection in Australia?
Australia has a concentrated HIV infection epidemic; MSM are the population group most affected by HIV, with about two-thirds of new infections occurring in this group.9 Heterosexual people who acquire HIV infection often originate from countries with a high prevalence of HIV.10
Despite high coverage of HIV testing among MSM and early prescribing of antiretroviral therapy, there has been growing concern about the failure of rates of new HIV notifications to decline. Risk factors for HIV infection acquisition within Australia among MSM, based on longitudinal cohort follow up of MSM, are:
- condomless anal intercourse
- injection of drugs
- methamphetamine use
- recently acquired infectious syphilis
- recent anal infections with either chlamydia or gonorrhoea
- having sexual partners who are HIV positive and not taking HIV antiretroviral therapy.11
It is generally not recommended that heterosexuals have PrEP unless they have a sexual partner who is HIV positive and not on treatment and they are having sex without using a condom. The Box provides guidance on eligibility for PrEP.12
What is the evidence for PrEP?
The effectiveness of oral PrEP containing tenofovir disoproxil fumarate has been demonstrated in 11 clinical trials among different populations including MSM, injecting drug users and heterosexuals at risk for HIV acquisition. It has been shown that oral PrEP provides high levels of protection against HIV infection – provided that adherence is high – and that there are limited short-term significant toxicities apart from small decreases of renal function and transient declines in bone mineral density (BMD).13
Two recent randomised trials using coformulated tenofovir disoproxil fumarate and emtricitabine in populations of European MSM have been reported.4,14 The reductions in HIV acquisition in both trials were 86% , which is the highest efficacy observed in PrEP trials to date and comparable with the efficacy of condoms at preventing HIV transmission.15 The real-world effect of PrEP in combination with repeated testing of high-risk populations and rapid initiation of HIV treatment in recently diagnosed individuals has led to a dramatic reduction in HIV notifications in central London.16 From October 2015 to September 2016, HIV diagnoses fell by 32% compared with October 2014 to September 2015.
How should I prescribe PrEP?
There are now state- and territory-based and national PrEP guidelines that provide recommendations on eligibility criteria and prescribing. PrEP is not currently available on the PBS, so patients can access coformulated tenofovir disoproxil fumarate and emtricitabine either through a private prescription for oral daily Truvada (although the cost is generally prohibitive at about $800 per month) or importation of generic versions from overseas using well-established online pharmacies ($50 to $100 per month). Patients can also be referred to state- and territory-based PrEP implementation programs such as:
- EPIC-NSW (https://endinghiv.org.au/nsw/stay-safe/epic/)
- QPrEP in QLD (http://www.comeprepd.info/qprepd-project/)
- PrEPX in Victoria (https://www.alfredhealth.org.au/research/research-areas/infectious-diseases-research/prepx-study)
- PrEPX-SA (https://www.alfredhealth.org.au/research/research-areas/infectious-diseases-research/prepx-south-australia).
What requires monitoring?
At the time of commencing PrEP, the patient should have HIV-negative status (i.e. a negative HIV test within seven days or as close as practically possible), hepatitis B and C infection should have been excluded, renal function established with an estimated glomerular filtration rate of more than 60 mL/min/1.73 m2. A repeat HIV test is generally recommended at four weeks and/or initiation of PrEP and subsequent three-monthly HIV and sexually-transmitted infection (STI) testing after this, which includes serology for syphilis (and HIV), chlamydia and gonorrhoea.
On each occasion, adherence to the daily dosing schedule, side effects, renal function monitoring and any symptoms suggestive of HIV seroconversion should be checked. Current recommendations in Australia are for daily dosing of PrEP and efficacy data suggest that taking at least four doses in seven days is required. The safety profile of daily coformulated tenofovir disoproxil fumarate and emtricitabine has been established from clinical trials with follow up of participants up to four years. Adverse reactions – including headache, abdominal pain and weight loss – are generally minor and self-limiting.
What are the controversies?
There have been concerns that PrEP availability results in increased rates of condomless sex and risk behaviours. Indeed, rates of STIs among high-risk MSM accessing PrEP programs appears to be much higher than the general MSM population; however, rates of STIs and condomless anal sex were increasing before PrEP became available.17 These issues have been carefully evaluated in PrEP implementation programs and to date there is conflicting evidence that PrEP actually results in increased risk behaviours such as condomless sex.
PrEP is not without potential toxicities with reduction in BMD and renal function observed, albeit in low numbers. Data regarding BMD to date found a 1% decline in BMD, but no increase in fragility fractures over the one to two years of observation compared with placebo, although the studies were too small and too short to detect any impact of PrEP on fracture incidence.18 In these studies, the decline in BMD was observed during the first few months on PrEP, and it either stabilised or returned to normal thereafter.
Other benefits of discussing PrEP with your patients
PrEP delivery programs emphasise that this is an opportunity to engage high-risk populations with clinical care and not just prescribing medication to prevent HIV acquisition. It is important to assess sexual health (and dysfunction), mental health, alcohol and other drug issues. HIV risk behaviour profiles of MSM accessing PrEP are not constant, with variations in risk, such as travelling, breaks in partnerships, associated alcohol consumption and other drug use. PrEP should not be viewed as an alternative to condoms but rather a complementary prevention method for high-risk populations who cannot use condoms all the time or risk exposures during these periods of their lifetime.
Conclusion
PrEP is an important new HIV prevention tool that can effectively reduce the acquisition of HIV infection by high-risk individuals. Recognising these high-risk patients and subsequently discussing PrEP with them can lead to important engagement with clinical services and regular comprehensive STI screening. PrEP should work alongside existing strategies to decrease the risk of HIV infection such as condom use and regular STI testing. MT
Further reading
This article is for general information purposes only, and the full product information should be consulted before prescribing any of the mentioned medications.