Syphilis: if you don’t look for it, you’ll miss it
Syphilis notification rates are rising in Australia, particularly in women of reproductive age. Congenital syphilis has significant morbidity and mortality, which can be easily prevented through antenatal screening, identifying ongoing risks for syphilis at subsequent encounters and early treatment during pregnancy. Asymptomatic presentations are not uncommon, and syphilis can also mimic other conditions. First-line treatment is benzathine benzylpenicillin, and there is emerging evidence for doxycycline for syphilis prevention. Contact tracing remains an important part of management to reduce transmission and the risk of reinfection.
Syphilis is caused by a spirochaete bacterium that is a subspecies of Treponema pallidum and is the only subspecies that is transmitted through sexual contact (vaginal, anal or oral sex). Transmission occurs following direct contact with an infectious lesion (chancre) in or on the penis, vagina, anus, rectum, lips or mouth. Transmission can also occur vertically across the placenta and with the use of injectable drugs.
Syphilis notification rates continue to rise with worrying trends among women of reproductive age. This is a significant concern because of the associated risk of congenital syphilis. This article provides an update on syphilis management with a focus on antenatal, maternal and infant care, as well as syphilis prevention.
Epidemiology and outbreak control
In 2020, an estimated 7.1 million adults had new-onset syphilis globally.1 In 2016, an estimated 661,000 infants were born with congenital syphilis, which is the second leading cause of preventable stillbirth.1 The most recent surveillance report from the Kirby Institute showed increasing notification rates of infectious syphilis (primary, secondary and early latent syphilis) in Australia, with a threefold increase (6.7 to 23.9 per 100,000) between 2012 and 2019.2 In 2021, there were a total of 5570 infectious syphilis notifications, primarily in men, people aged 25 to 39 years and those residing in major cities.2 In 2021, the incidence of infectious syphilis among HIV-positive homosexual and bisexual men attending sexual health clinics was 8.1 new infections per 100 person-years, compared with 5.5 new infections per 100 person-years in HIV-negative homosexual and bisexual men.2 An ongoing trend of concern is the increase in notification rates in women by sixfold from 1.4 to 8.5 per 100,000 between 2012 and 2021, with the highest rates in women aged between 15 and 29 years.2
In response to the increasing rates of syphilis in Australia, the National Syphilis Strategic Surveillance and Monitoring Plan was implemented in 2021.3 The key priorities of this plan include reducing the incidence of syphilis (particularly in women of reproductive age), eliminating congenital syphilis and controlling outbreaks in Aboriginal and Torres Strait Islander communities.
An infectious syphilis outbreak in regional and remote Aboriginal and Torres Strait Islander communities was first reported in northwest Queensland in January 2011, which spread to the Northern Territory, Western Australia and South Australia. There was a fourfold increase in infectious syphilis notifications among Aboriginal and Torres Strait Islander peoples between 2012 and 2019 (29 to 122.6 per 100,000), with more infections reported in young, heterosexual people.2 Between 2012 and 2021, 54% (37 of 68 cases) of congenital syphilis notifications were in Aboriginal and Torres Strait Island people, with the rate in 2021 almost 27 times higher than that in non-Aboriginal people.2
A national plan was developed in 2017 to manage these areas of outbreak.4 The key strategies of this plan include improving testing and treatment, surveillance and reporting, education and awareness, and antenatal care. Different jurisdictions have implemented various responsive measures, including initiatives such as offering additional universal syphilis testing during pregnancy; introducing point-of-care testing to reduce the time between testing and treatment; and launching campaigns to increase disease awareness, such as the Young Deadly Free campaign (https://youngdeadlyfree.org.au/young-deadly-syphilis-free/).
Antenatal screening
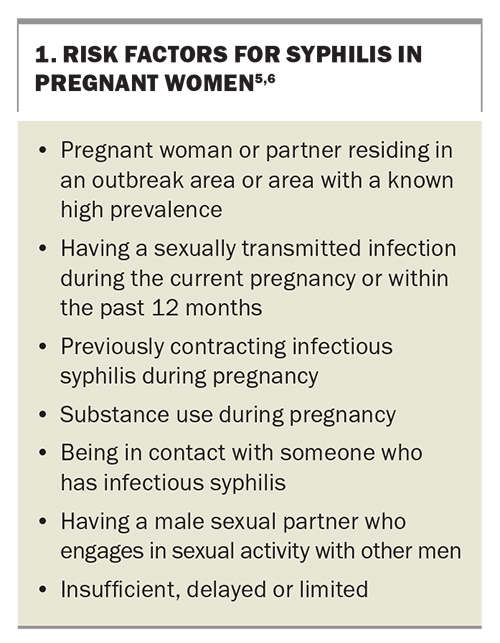
Considering the high burden of morbidity and mortality associated with congenital syphilis, one of the WHO goals is to work towards eliminating mother-to-child transmission of syphilis. Universal screening for syphilis is recommended at the first antenatal visit. The minimum time points for repeat testing for women with a high risk of infection or reinfection are in the third trimester (28 to 32 weeks of gestation) and at the time of birth.5 States with syphilis outbreaks have adapted this recommendation to suit their local needs with additional universal antenatal screening. Pregnant women who receive insufficient or limited antenatal care represent missed opportunities for testing and early treatment; therefore, a focus on how to address this gap in care can improve maternal and infant health outcomes. Factors that increase the risk of syphilis in a pregnant woman should be considered at each encounter (Box 1).5,6 Refer to your local state guidelines for up-to-date recommendations related to antenatal testing for syphilis.
Syphilis testing
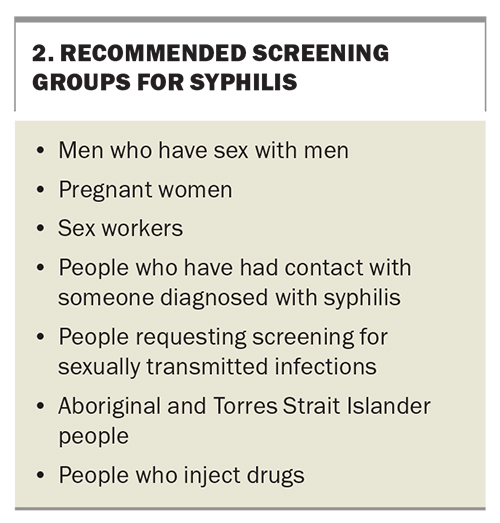
Syphilis testing should be offered as part of routine sexual health screening. There are also recommendations for specific populations that should be screened (Box 2). The interpretation of syphilis serology requires the assessment of two types of serological tests: treponemal-specific tests and nontreponemal tests.
Treponemal-specific tests detect antibodies to T. pallidum antigens, the results of which remain positive for life even after treatment; however, these tests do not indicate disease activity and should be interpreted in conjunction with nontreponemal tests. Enzyme immunoassay tests can be automated and are frequently used for screening. Their sensitivity and specificity vary depending on the stage of infection. Confirmatory treponemal-specific tests include the T. pallidum particle agglutination assay, T. pallidum haemagglutination test and fluorescent treponemal antibody absorption test.
Nontreponemal tests indirectly detect T. pallidum by detecting antibodies to reagin (cardiolipin), which is a byproduct of spirochaetes-induced cell wall damage. Nontreponemal tests include the rapid plasma reagin (RPR) and Venereal Diseases Research Laboratory (VDRL) tests, the results of which are reported as a titre (1:8, 1:16, 1:32, etc.). Changes in this titre indicate disease activity. A fourfold reduction in titre indicates an adequate response to treatment, whereas a fourfold increase in titre indicates reinfection.7
PCR testing can be useful for diagnosing early-stage infection, and the results can be positive before there is a serological response. A viral transport medium swab is taken from a syphilitic lesion and is the most useful for establishing a diagnosis of primary syphilis.
Clinical manifestations
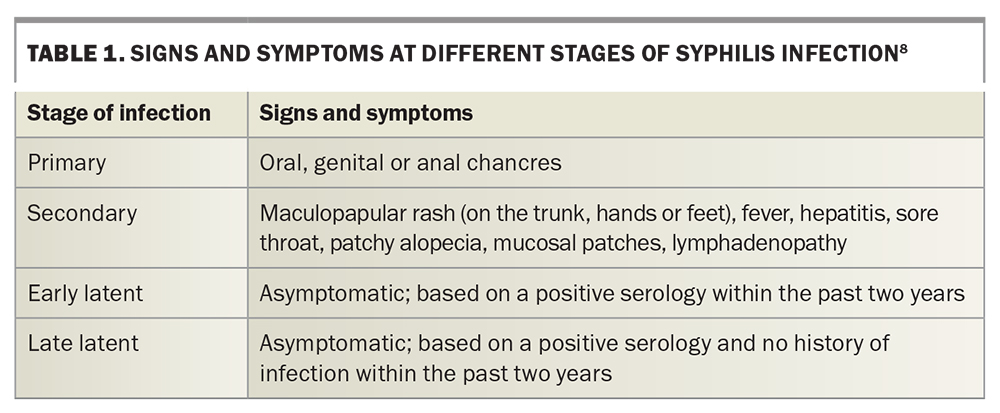
Syphilis can present as a myriad of signs and symptoms that mimic other illnesses; therefore, GPs should have a high index of suspicion. Around 50% of people will be asymptomatic, hence why asymptomatic screening is recommended.8 The course of infection progresses through several clinical stages (Table 1).8
Primary syphilis
The incubation period for primary syphilis is between nine and 90 days (average of three weeks).9 During this period, patients present with an ulcer (chancre) at the site of inoculation, depending on the type of sexual exposure, which is associated with nontender local lymphadenopathy. A typical chancre is solitary, painless and indurated (firm) with a clean base and can present on the vulva, cervix, penis, anus, or oral mucosa. However, GPs should be aware of atypical presentations of chancres that are multiple, painful and purulent. Without treatment, chancres will spontaneously heal within a few weeks.9
Secondary syphilis
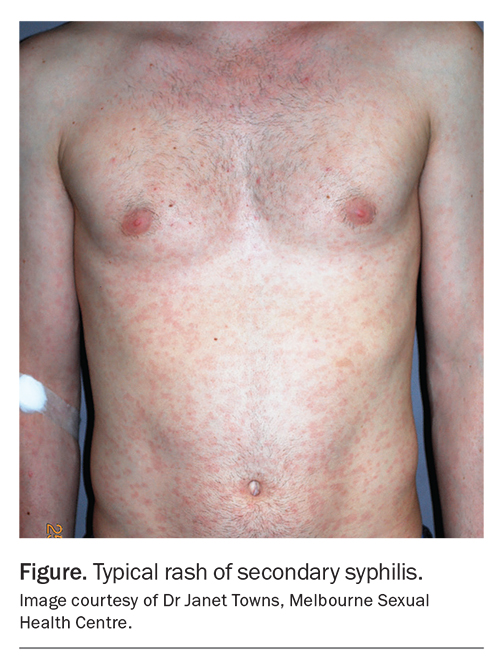
The incubation period for secondary syphilis is two to 24 weeks (average of six weeks).9 Haematogenous and lymphatic dissemination causes the infection to affect multiple organ systems and cause signs and symptoms that mimic other conditions. Most patients will present with a maculopapular rash on the trunk (Figure), sometimes involving the palms and soles, as well as systemic symptoms of fever, malaise, headache, sore throat and lymphadenopathy. The systemic symptoms and rash can be mistaken for other causes, such as glandular fever or drug eruption; therefore, it is important to consider syphilis among the differential diagnoses. Other symptoms can include oral or genital mucosal patches, condylomata lata (soft, wartlike growths in moist areas), patchy alopecia, hepatitis and glomerulonephritis. If left untreated, the symptoms of secondary syphilis will resolve but can reoccur up to two years after infection.9
Neurosyphilis, ocular syphilis and otosyphilis
Neurosyphilis, ocular syphilis and otosyphilis can occur during secondary syphilis. It is important to assess patients for symptoms, conduct a thorough examination and urgently refer to specialist services for management and treatment to avoid permanent deficits.
Ocular syphilis and otosyphilis can occur in isolation or with other manifestations of neurosyphilis. Ocular syphilis affects various structures in the eye, most commonly causing uveitis but also interstitial keratitis, conjunctivitis, optic neuropathy and retinal vasculitis.10 Reported symptoms include blurry vision, the presence of ‘floaters’, eye pain, eye redness and decreased vision.11 Urgent review by an ophthalmologist is recommended to commence appropriate treatment and prevent permanent vision loss. Otosyphilis affects the eighth cranial nerve, causing vestibulocochlear symptoms, such as vertigo, tinnitus and sensorineural hearing loss.12 Unilateral or bilateral hearing loss can occur acutely and progress quickly with permanent deficits.
Early neurosyphilis occurs in the first few months or years of untreated infection, and the presentations may include headaches, dizziness, altered mental state, meningitis and stroke.12 Late neurosyphilis or tertiary syphilis occurs several years after untreated infection with presentations that include progressive cognitive decline, gait disturbance, motor and sensory loss and severe radicular pain.12
Confirming a diagnosis of neurosyphilis can be challenging, as there is no consensus on definitive diagnostic criteria. A cerebrospinal fluid (CSF) examination should be considered if there is clinical evidence of neurosyphilis or if there are abnormal examination findings suggestive of ocular syphilis or otosyphilis; however, a negative CSF result does not exclude a diagnosis of neurosyphilis and should be interpreted in the context of clinical signs and reactive syphilis serology.
Latent syphilis
Latent syphilis is divided into early and late latent infection. The differentiation is important when it comes to treatment. Early latent syphilis is diagnosed based on a positive serology, an absence of symptoms and evidence of having been infected in the last two years.13 It is useful to gather information about previous negative serology and any preceding history of symptoms that suggest primary or secondary syphilis. Of note, symptoms of secondary syphilis can also recur during this early latent stage. The diagnosis of late latent syphilis is based on similar features, but infection may have occurred more than two years prior.13
Tertiary syphilis
Tertiary (late) syphilis is less commonly seen in the current antibiotic era and develops after months or years if left untreated in about one-third of cases. Symptomatic late disease includes cardiovascular, late neurological and gummatous effects.13
Congenital syphilis
Untreated syphilis during pregnancy can cause devastating outcomes, such as preterm birth, stillbirth, low birth weight, neonatal death and congenital syphilis.5 Congenital syphilis occurs through vertical transmission at any stage of the pregnancy; therefore, early detection and treatment are essential to prevention.
Infants can be asymptomatic at birth and develop clinical features over time. Clinical manifestations of congenital syphilis are multisystemic and can be subtle and variable. Most infants exhibit signs and symptoms by 3 months of age. In the first two years, these can include maculopapular or bullous rash, haemorrhagic rhinitis or ‘snuffles’, generalised lymphadenopathy, hepatosplenomegaly and inflammation of the bones.14 Other signs include a low birth weight and failure to thrive, as well as haematological, ophthalmic and neurological abnormalities. After two years, late clinical findings include facial and bone abnormalities, tooth damage, interstitial keratitis, seizure disorders and intellectual disability.14
Management and follow up of the neonate are vital if congenital syphilis is a possibility. The Australian Society for Infectious Diseases have updated the guidelines for the management of perinatal infections.6 The recommendations include performing an infant serology, full clinical examination, placental histopathology and, if available, placental PCR. If findings are abnormal, further investigations to confirm a diagnosis of congenital syphilis or neurosyphilis include a full blood count, liver function testing, urea electrolytes and creatinine measurement, long bone and chest x-ray, and lumbar puncture. An infant with congenital syphilis or a high risk of congenital syphilis should be given benzylpenicillin intravenously as treatment and requires regular follow-up serology to ensure that the treatment is adequate. An infant with normal investigation results still requires follow-up serology at 3 and 6 months of age. If the serology remains negative, no further follow up is required.
A multidisciplinary approach may be required to engage the mother for both maternal and infant monitoring and contact tracing. If available, refer to the local or state protocol for the management of syphilis in pregnancy and congenital syphilis, or speak to a specialist service.
HIV and syphilis coinfection
HIV testing should be conducted in patients who have tested positive for syphilis. The diagnosis, treatment and follow up of syphilis infection in patients who test positive for HIV are managed the same as in patients who test negative for HIV. There are some considerations in patients with syphilis who test positive for HIV; these are uncommon but include an increased risk of neurological complications in early-stage infection, unusual serological responses (false-negative results and delayed seroconversion) and treatment failure.15 It is important to be aware that CSF abnormalities of a raised leucocyte count and protein levels are common in patients without syphilis who test positive for HIV; therefore, this needs to be considered when interpreting CSF results in the context of possible neurosyphilis.14
Treatment
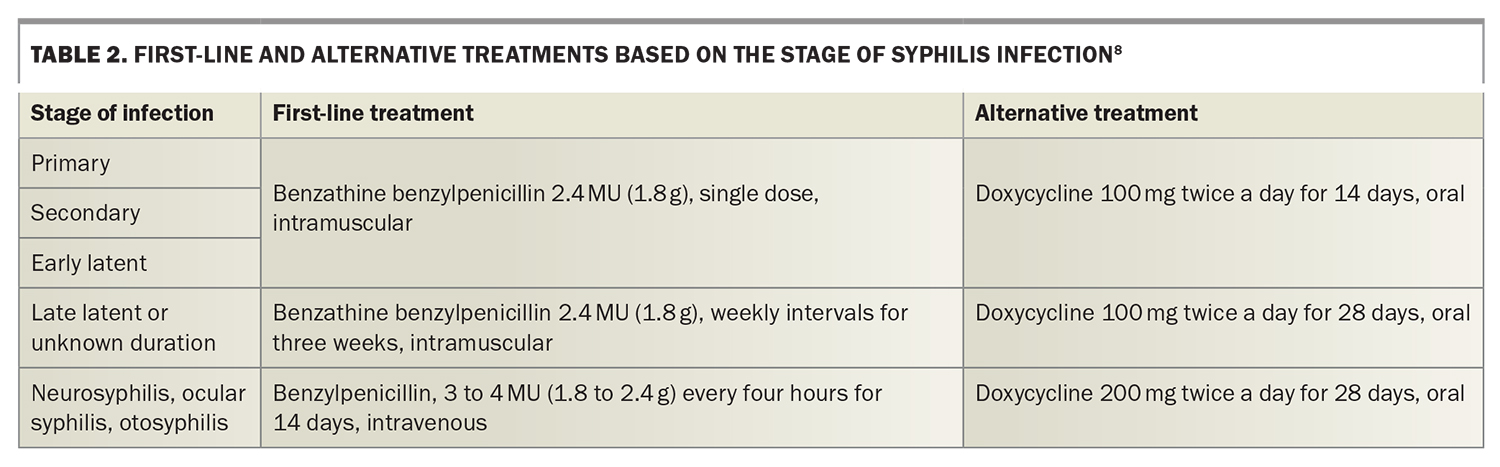
Treatment for infectious syphilis (primary, secondary or early latent) involves a single intramuscular dose of benzathine benzylpenicillin 2.4 MU (1.8 g). This is the first-line treatment and, fortunately, penicillin resistance is not an issue. Late latent syphilis requires extra doses of benzathine benzylpenicillin 2.4 MU (1.8 g) administered at weekly intervals for a total for three doses. If one dose is delayed by more than seven days (i.e. the interval is more than 14 days), the three-dose course of treatment should be restarted. If the duration of infection is unknown, treatment should be given as that for late latent syphilis. Benzathine benzylpenicillin is available for order in the ‘doctor’s bag’. The first-line and alternative treatments at different stages of infection are presented in Table 2.8
Patients may experience a Jarisch–Herxheimer reaction six to 12 hours after treatment and should be informed of the risk of this prior to administration. The symptoms can include fever, headache, myalgia and rigors, which improve within 24 hours.
Alternative treatment with doxycycline is only recommended if the patient’s allergy history is well documented or if the patient is intolerant to injections. In these cases, it is important to address adherence and to ensure close follow up to ensure that the treatment response is adequate.
Referral to a specialist service is recommended if there is evidence of neurosyphilis, ocular syphilis, otosyphilis or tertiary syphilis, as the treatment requires intravenous administration of antibiotics.
Treatment during pregnancy and maternal management
Patients with syphilis who are pregnant should also be referred to a specialist service to ensure adequate treatment, monitoring, follow up and contact tracing of both the pregnant woman and infant. Doxycycline use during pregnancy is contraindicated; therefore, benzathine benzylpenicillin is the best option using the same dose administered as that for a nonpregnant woman. Desensitisation is often required if the woman is allergic to penicillin. Jarisch–Herxheimer reactions can also occur in pregnant women, and it is important to advise them to seek medical attention if they develop uterine contractions, loss of foetal movement or fever.6 Treatment is not required if biological test results are false positive or if there is a clear history of adequate syphilis treatment prior to pregnancy and no risk for reinfection. If treatment is given early during pregnancy, repeat serology is recommended at 26 to 28 weeks and at 34 to 36 weeks of gestation, as well as postpartum.6 It is likely that a fourfold reduction in the RPR or VDRL titre may not occur prior to delivery to help confirm an adequate response to treatment.
Response to treatment and follow up
To monitor the response to treatment, repeat RPR or VDRL testing should be conducted every three months.16 It is ideal to conduct this testing at the same laboratory and to use the same nontreponemal test for comparison (e.g. RPR to RPR, not RPR to VDRL). Adequate treatment is indicated by a fourfold reduction in the RPR or VDRL titre over a 12-month period. If there is a fourfold increase, this is most likely due to reinfection and the patient will need retreatment. If the interpretation is unclear, refer to a specialist service for further advice.
Contact tracing
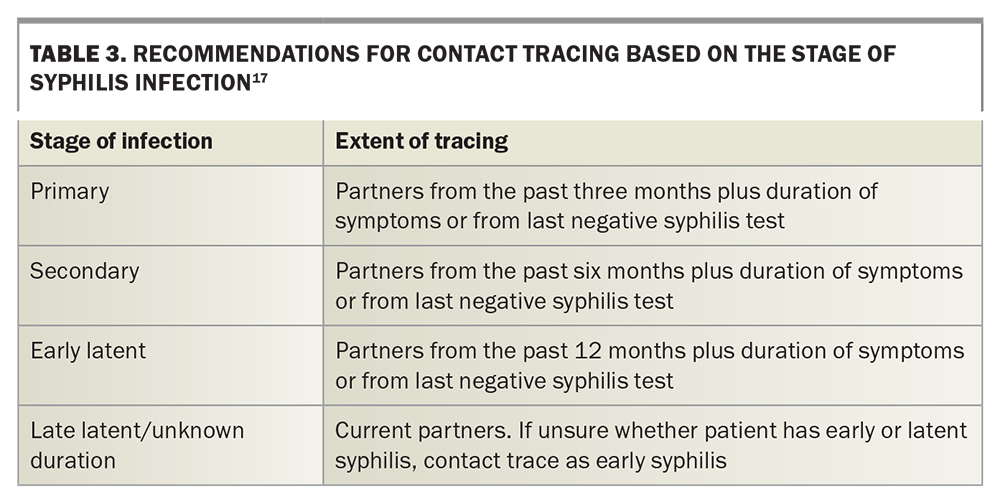
Contact tracing or partner notification is a crucial component of management to prevent ongoing transmission and reinfection. The extent of the tracing required depends on the clinical stage of the infection (Table 3).17 Late latent and tertiary syphilis are less likely to be infectious; however, it is not unreasonable to test current partners and children. Contact tracing can be performed by the patient themselves, or with the aid of healthcare professionals or online contact tracing services while maintaining anonymity. Additional contact tracing support should be extended to pregnant women, mothers and infants born with congenital syphilis.
Those who have had contact with patients with infectious syphilis in the past three months should be offered presumptive treatment with benzathine benzylpenicillin 2.4 MU (1.8 g), as the syphilis serology may still be negative in the early stages of infection. If the contact had occurred beyond three months prior, syphilis testing can be performed to determine if treatment is necessary.
Syphilis prevention
In addition to continuing work in the areas of health promotion, health education, awareness of condom use and peer outreach, research on vaccinations and biomedical prevention has been undertaken to reduce the rates of sexually transmitted infections.
Current studies are investigating the use of doxycycline as postexposure prophylaxis (PEP) with the regimen of taking doxycycline 200 mg within 24 to 72 hours after condomless sex. This has been shown to be effective in reducing syphilis infections in men who have sex with men and transgender women; however, it has not yet been shown to be effective in cisgender women.18 Different studies in France, the USA and Canada have shown consistent findings of the regimen in reducing syphilis infections. In the DOXYVAC trial in France, the incidence of an initial episode of syphilis was 5.6 per 100 person-years in the group taking doxycycline as PEP, compared with 35.4 per 100 person-years in the non-PEP group.19 However, there are still unknown outcomes related to antimicrobial resistance in the context of sexually transmitted infections and other pathogenic organisms.
Using doxycycline as PEP is not currently endorsed by professional bodies in Australia; however, a survey conducted in Melbourne suggests that some individuals are already using doxycycline as PEP.19 The Australasian Society for HIV Medicine published an interim position statement, summarising the evidence for the risks and benefits of using doxycycline as PEP with the aim of assisting clinician–patient discussions.19
Conclusion
The fundamentals of the diagnosis and management of syphilis remain largely unchanged; however, there have been shifts in its epidemiology in Australia, mainly reflected in increasing rates in women of reproductive age and increasing rates of congenital syphilis. Early identification, treatment and prevention strategies can reduce the risk of health sequalae related to syphilis, including syphilis during pregnancy and congenital syphilis. Many syphilis diagnoses are made in general practice, where it can be managed by consulting national and state guidelines and with assistance from local sexual health services. As more information becomes available about the risks, benefits and unknown factors associated with the use of doxycycline as syphilis prophylaxis, there may be increased patient and clinician interest in this prevention method. MT
COMPETING INTERESTS: None.
References
1. Global progress report on HIV, viral hepatitis and sexually transmitted infections, 2021. Accountability for the global health sector strategies 2016–2021: actions for impact. Geneva: World Health Organisation; 2021. Available online at: https://www.who.int/publications/i/item/9789240027077 (accessed May 2023).
2. King J, McManus H, Kwon A, Gray R, McGregor S. HIV, viral hepatitis and sexually transmissible infections in Australia: annual surveillance report 2022. Sydney: The Kirby Institute, UNSW Sydney; 2022. Available online at: https://kirby.unsw.edu.au/report/asr2022 (accessed May 2023).
3. National syphilis surveillance and monitoring plan 2021. Canberra: Australian Government Department of Health; 2021. Available online at: https://www.health.gov.au/resources/publications/national-syphilis-surveillance-and-monitoring-plan-2021?language=en (accessed May 2023).
4. National strategic approach for an enhanced response to the disproportionately high rates of STI and BBV in Aboriginal and Torres Strait Islander people. Canberra: Department of Health and Aged Care; 2018. Available online at: https://www.health.gov.au/resources/publications/national-strategic-approach-for-an-enhanced-response-to-the-disproportionately-high-rates-of-sti-and-bbv-in-aboriginal-and-torres-strait-islander-people (accessed May 2023).
5. Clinical Practice Guidelines: Pregnancy Care, 2020 Edition. Canberra: Australian Government Department of Health; 2020. Available online at: https://www.health.gov.au/resources/pregnancy-care-guidelines (accessed May 2023).
6. Australasian Society for Infectious Diseases (ASID). Management of perinatal infections. 3rd ed. Palasanthiran P, Starr M, Jones C, Giles M, eds. Sydney: ASID; 2022. Available online at: https://asid.net.au/publications (accessed May 2023).
7. Oxford Textbook of Medicine. 6th ed. Firth J, Conlon C, Cox T, eds. Oxford: Oxford University Press; 2020.
8. Ong JJ, Bourne C, Dean JA, et al. Australian sexually transmitted infection (STI) management guidelines for use in primary care 2022 update. Sex Health 2023; 20: 1-8.
9. Mindel A, Tovey S, Timmins D, Williams P. Primary and secondary syphilis, 20 years’ experience. Genitourinary Med 1989; 65: 1-3.
10. Northey LC, Skalicky SE, Gurbaxani A, McCluskey PJ. Syphilitic uveitis and optic neuritis in Sydney, Australia. Br J Ophthalmol 2015; 99: 1215-1219.
11. Ong D, Bhardwaj G, Ong JJ, Chen MY, Lim LL. Keeping an eye on syphilis. Aust J Gen Pract 2017; 46: 401-404.
12. Jones-Vanderleest JG. Neurosyphilis, ocular syphilis, and otosyphilis: detection and treatment. Am Fam Physician 2022; 106: 122-123.
13. Clark EG, Danbolt N. The Oslo study of the natural history of untreated syphilis; an epidemiologic investigation based on a restudy of the Boeck-Bruusgaard material; a review and appraisal. J Chronic Dis 1955; 2: 311-344.
14. Kingston M, French P, Higgins S, et al. UK national guidelines on the management of syphilis 2015. Int J STD AIDS 2015; 27: 421-446.
15. Workowski K, Bachmann L, Chan P, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep 2021; 70: 1-187.
16. Syphilis. Sydney: Australian STI Management Guidelines for Use in Primary Care; 2021. Available online at: https://sti.guidelines.org.au/sexually-transmissible-infections/syphilis/ (accessed May 2023).
17. Syphilis. Sydney: Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine; 2022. Available online at: https://contacttracing.ashm.org.au/syphilis/ (accessed May 2023).
18. Doxycycline does not prevent STIs among cisgender women. Proceedings of the Conference on Retroviruses and Opportunistic Infections; 2023 Feb 19-23; Seattle, Washington. New York: National AIDS Treatment Advocacy Project; 2023. Available online at: https://www.natap.org/2023/CROI/croi_10.htm (accessed May 2023).
19. Cornelisse VJ, Ong JJ, Ryder N, et al. Interim position statement on doxycycline post-exposure prophylaxis (Doxy-PEP) for the prevention of bacterial sexually transmissible infections in Australia and Aotearoa New Zealand - the Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine (ASHM). Sex Health 2023; 20: 99-104.