Chronic rhinosinusitis: alleviating symptoms and improving quality of life
Sinus complaints are common and can be attributed to a variety of rhinological and nonrhinological disorders. Chronic rhinosinusitis is a disease of persistent sinonasal inflammation for which corticosteroid therapy provides patients with symptomatic relief and an improved quality of life. Functional endoscopic sinus surgery provides a means for long-term management with use of topical therapies alone.
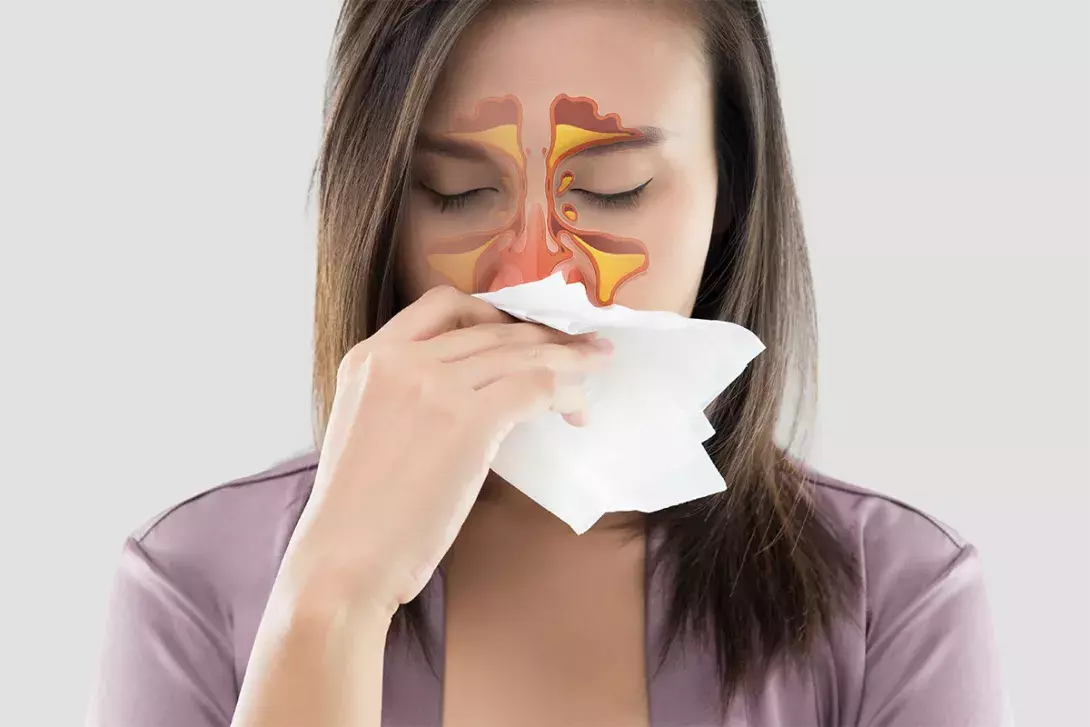
- Chronic rhinosinusitis is a heterogeneous condition of sinonasal inflammation, manifesting with symptoms of nasal obstruction/congestion, nasal discharge, reduction in smell and facial pain/pressure. Endoscopic and radiological assessment shows mucosal oedema with or without nasal polyps.
- Despite overlapping symptomatology, history, examination and imaging can differentiate chronic rhinosinusitis from rhinitis, sinonasal neoplasms and nonsinogenic pathology, such as headache or migraine disorders.
- Management with topical and systemic corticosteroids and nasal saline irrigation is complemented by functional endoscopic sinus surgery to facilitate improved delivery of topical therapy. Doxycycline and macrolide antibiotics can be used for their anti-inflammatory and immunomodulatory effects, however, prolonged courses are required.
- Functional endoscopic sinus surgery entails removal of bony sinonasal partitions to reduce the surface area of the inflammatory burden, and maximise access for nasal sprays and irrigation into the sinuses.
- Biological therapy is available for refractory disease.
- First-line management that can be initiated by GPs includes intranasal corticosteroid sprays and saline nasal irrigations. Noncontrast CT of the paranasal sinuses is the imaging modality of choice and should be performed in patients who have persistent symptoms and before specialist referral.
- Long-term supplementary care by the treating specialists and GP is required to ensure patient compliance with maintenance therapy and management of disease exacerbations or recurrence.
Chronic rhinosinusitis (CRS) is defined by symptomatology in conjunction with endoscopic and/or radiological findings (Box 1). However, in general practice and in epidemiological studies, the definition is often based on symptomatology alone, which may overestimate the prevalence due to overlap with rhinitis conditions.1
Epidemiology
The true prevalence of CRS is estimated to be less than 5% when using guideline-based diagnostic criteria.2 It is more commonly diagnosed in middle-aged and older patients, women, current and former cigarette smokers and individuals who consume alcohol on a regular basis.3
CRS imposes a greater impact on social functioning than angina or chronic heart failure.4 Total direct costs of CRS with nasal polyps in a Dutch cohort of patients was €1500 per patient per year, primarily due to outpatient department visits and hospitalisation.5 The indirect costs are amplified as the disease process predominantly affects people of working age resulting in missed work and study and reduced productivity.
Classification
CRS is heterogeneous and multifactorial in aetiology, but the common outcome is chronic sinonasal inflammation. Previous disease distinctions based on the presence or absence of nasal polyps have been replaced by nuanced systems incorporating disease distribution, underlying immune dysfunction and aetiology. The current classification of CRS is divided into primary and secondary disease and further categorised based on distribution and endotype (Figure 1 and Figure 2).1 This enables stratification of patients into clinically relevant phenotypes that guide management (Box 2).6-9
Definitive endotype diagnosis is based on histopathological analysis of sinonasal tissue and mucous; examination of cell type (eosinophils, neutrophils, lymphocytes) and quantity (number per high powered field); epithelial, subepithelial and basement membrane alterations; and the presence of fungal elements and cell breakdown products. Standardised reporting has been developed to assist pathologists and clinicians.
Pathophysiology
CRS is due to a complex dysfunctional interaction between environmental factors and the host immune system. Interactions and influences of environmental stimuli vary between individuals, giving rise to differing endotypes and phenotypes of disease. There is mounting evidence for an underlying genetic basis with polymorphisms in the major histocompatibility complex (MHC) genes involved in antigen-specific adaptive immune responses, innate immunity and specific inflammatory pathways and mediators.10 Additional areas of active research include the role of allergy, staphylococcal superantigen, bacterial biofilm, fungal colonisation and abnormalities of the eicosanoid pathway. Nevertheless, the final common pathway is a loss of immune tolerance at the mucosal level and beyond, with subsequent chronic inflammation, tissue remodelling and symptom development.
This inflammatory response can propagate from the confines of the sinonasal cavity to affect the lower airway, and vice versa – the united airway disease hypothesis.11 The purported mechanism is that localised airway inflammation leads to a systemic response, with bone marrow involvement, resulting in the release of progenitor cells that are then recruited to distant tissue sites.12 It has been shown that allergen exposure in one part of the airway (upper or lower) can elicit an inflammatory response in both areas within 24 to 48 hours of the challenge.13,14 A neurogenic nasobronchial reflex has also been described.15 The united airways hypothesis exists for atopic and nonatopic individuals as seen in patients with NSAID-exacerbated respiratory disease (NERD), characterised by the Samter’s triad of aspirin sensitivity, nasal polyposis and asthma.
Aetiology
The aetiology of primary CRS is multifactorial, with involvement of environmental, host immune behaviour, allergy, infective and genetic elements. CRS can also be secondary to a wide array of local and systemic disease processes. Common causes of localised disease include dental infection (odontogenic sinusitis), inhaled noninvasive fungal accumulation (mycetoma), neoplasia and anatomic alterations (e.g. uncinate process lateralisation and silent sinus syndrome). Systemic considerations include autoimmune and vasculitic processes (granulomatosis with polyangiitis, Churg-Strauss syndrome), cystic fibrosis (CF) and primary ciliary dyskinesia (PCD; especially in children with CRS) and immune deficiency. In these circumstances, investigation and management of the underlying aetiology is pivotal to addressing the CRS.
Associations
About 25% of patients with CRS have asthma (compared with 5% in the general population).1 Onset of asthma may precede or follow the onset of CRS and the type of asthma can mirror the CRS endotype – childhood allergic asthma in central compartment atopic disease (CCAD) and adult-onset eosinophilic asthma in type 2 eosinophilic CRS. Allergic rhinitis has significant symptom overlap with CRS. The prevalence of allergy in CRS varies with phenotype, with stronger associations in CCAD and allergic fungal rhinosinusitis (AFRS). Other relevant CRS associations include gastro-oesophageal reflux disease (GORD), NERD, immunodeficiency, smoking, alcohol consumption and exposure to air pollution.
Clinical features
The cardinal symptoms of CRS are nasal blockage, obstruction or congestion; anterior or posterior nasal discharge; facial pain or pressure; and hyposmia or anosmia. Hyposmia is more common in patients with the type 2 endotype of CRS and is believed to be caused by both mechanical obstruction of the olfactory cleft from mucous and polyps, as well as the effect of inflammatory changes on olfactory neuron function. These patients often respond favourably to courses of systemic corticosteroids and report a return of their smell while on the medication. Facial pain is a common presenting symptom and often suspected to be ‘sinus’ in origin but, in isolation, is rarely due to CRS.16
In all patients with a sinonasal presentation, red flag symptoms and signs that may indicate a disease complication or an alternative diagnosis (e.g. sinonasal malignancy) must be elicited (Box 3). Furthermore, certain occupational exposures have been associated with the development of sinonasal squamous cell carcinoma (nickel, softwood dust) and adenocarcinoma (hardwood dust).
Investigations
Quality of life (QoL) measures
The sinonasal outcome test (SNOT-22) is a multi-language validated self-administered CRS-specific questionnaire of 22 items rated from 0 (no problem at all) to 5 (worst possible symptom) to help measure disease severity in patients with CRS. Total scores greater than 50 reflect a severe impact of CRS and a cut-off score of 40 or more is incorporated into the criteria for biological therapy.1,17 Other QoL measures include the nasal obstruction and symptom evaluation (NOSE) scale, the 36-item short form survey (SF-36) and visual analogue scales (VAS).
Imaging
Noncontrast CT of the paranasal sinuses is the primary imaging modality and provides sufficient information regarding disease extent and anatomical factors relevant for surgery in most patients. The presence of a double density on the soft tissue sequences is a hallmark of fungal disease. However, there are limitations in differentiating opacification due to the presence of polyps, mucous and neoplasms, as well as delineating extent of disease beyond the paranasal sinuses. The Lund-Mackay score was developed to stratify the severity of disease based on CT, with higher scores predicting greater risk of disease recurrence.18 Contrast enhanced CTs are rarely performed for CRS, as MRI provides greater detail without the added radiation exposure. MRI with gadolinium enhancement provides the greatest detail regarding the nature and extent of sinonasal disease. Mucous, polyps (T2-hyperintense), neoplasms (T1 with contrast enhancement) and fungus (T1 and T2 signal void) can be clearly distinguished, and disease extension into surrounding regions (e.g. intracranial, intraorbital, infratemporal fossa) mapped. The principal limitations of MRI are availability, cost and lack of clear bony anatomy for surgical planning. For both CT and MRI, current imaging technology permits submillimetre image slicing that can be merged with real-time patient landmarks to allow use of intraoperative navigation systems that assist with localisation for difficult cases. This has been demonstrated to reduce major and total complications.19
Sinus x-rays no longer have a primary role in sinonasal disease, as multidetector and cone beam CT reduce radiation exposure by shortening scan time and using postprocessing techniques to preserve image quality and anatomical accuracy.
Nasal function assessment
Peak nasal inspiratory flow and rhinomanometry can be used to quantitatively assess nasal obstruction (pre- and post-treatment). The University of Pennsylvania Smell Identification Test (UPSIT) and European Sniffin’ Sticks can be used for assessment of hyposmia/anosmia.
Other tests
Routine preoperative haematology and biochemistry are often performed to exclude undiagnosed thrombocytopenia, coagulopathy or other abnormalities that may impact on general anaesthesia or surgery. Serum total and specific IgE can help elicit an underlying allergic process, but skin prick testing is preferred. Further serological testing (e.g. autoimmune and vasculitic screen, genetic testing for CF) is directed by clinical suspicion of a possible underlying aetiology for CRS.
Differential diagnosis
The clinical presentation of CRS can overlap with a variety of other sinonasal and neurological disorders. Facial pain as a primary presentation in the absence of other rhinological symptoms is rarely due to CRS. In a prospective study where CT scans were performed acutely in patients presenting with suspected recurrent acute rhinosinusitis, only one patient (of 48) had findings consistent with sinusitis whereas the remainder had rhinitis (47%), headache/migraine (37%) or facial pain otherwise undefined (12.5%).12 A careful history of symptoms and symptom duration, the presence of red flag features, findings on nasendoscopy and imaging can assist in differentiating CRS from other conditions such as rhinitis (viral, postviral, bacterial, allergic) sinonasal neoplasms, migraine, headache, trigeminal neuralgia, temporomandibular joint disorder dysfunction and midsegment facial pain.
Management
Management of CRS entails complementary medical and surgical interventions to suppress the sinonasal inflammatory burden, minimise symptoms and maximise quality of life. Corticosteroids are fundamental to achieving these goals, and surgery offers a means for topical administration to achieve disease control and avoid systemic exposure. Nasal saline irrigations, antibiotics and management of comorbidities (e.g. allergy, GORD, autoimmune/vasculitis) supplement overall care.
Intranasal corticosteroids
High-quality evidence supports the long-term efficacy and safety of intranasal corticosteroids (INCS).1 Superiority of one type over another (e.g. mometasone, budesonide, fluticasone, beclomethasone) has not been demonstrated; however, higher doses may be associated with an increased risk of epistaxis.20 Symptom reduction is greatest in patients with nasal polyps by reducing polyp size and preventing recurrence. Delivery of INCS through a nasal irrigation medium has been shown to improve sinonasal penetration and symptom and disease control in postoperative patients compared with simple spray devices.21 High-volume, high-pressure delivery achieves the desired anti-inflammatory effects with almost negligible systemic absorption.
Concerns about the impact of prolonged INCS use have been quashed, with no significant effects on the hypothalamic–pituitary axis, cortisol levels, childhood growth rate, bone mineral density, intraocular pressures, lens opacification or local mucosal atrophy demonstrated in multiple studies.22-24 Common local adverse effects occur in 5 to 10% of patients and include epistaxis, throat irritation, nasal dryness, and burning and stinging sensations. Except for epistaxis, the incidence of such side effects is similar to placebo, and they are mild in severity, usually resolving without discontinuation of treatment.25
Systemic corticosteroids
Systemic corticosteroids, with or without local corticosteroid treatment, significantly reduce symptoms and nasal polyps.1 Dosage and duration have not been standardised but most studies report courses of two to three weeks, with or without tapering regimens.26,27 One to two courses of systemic corticosteroids per year can be a useful adjunct to regular INCS treatment; however, if more frequent courses are required, surgery should be considered. Adverse effects include hypothalamic–pituitary–adrenal axis inhibition, hyperglycaemia and diabetes, osteoporosis, avascular necrosis of the femoral head, gastrointestinal disturbance and peptic ulceration, cataract formation, glaucoma, infection, hypertension, acute myocardial infection, neuropsychiatric effects and cushingoid features. Fortunately, besides minor sleep disturbance and gastrointestinal upset, most of these side effects are extremely rare and have not been demonstrated with infrequent, short courses. Nonetheless, all patients prescribed systemic corticosteroids must be counselled about the possible adverse effects, especially those with vulnerable comorbidities (e.g. diabetes, psychiatric disorders, peptic ulcer disease).26
Antibiotics
The role of antibiotics in CRS is unclear and, when used, it is chiefly for their immunomodulatory, not antimicrobial, activity. The most commonly used antibiotics for CRS are doxycycline and macrolides (e.g. clarithromycin, roxithromycin, azithromycin).
Doxycycline is a tetracycline antibiotic most effective in CRS with a type 2 inflammatory endotype. Anti-inflammatory effects are exerted by inhibiting the activity of matrix metalloproteinases, suppressing proinflammatory cytokines (e.g. tumor necrosis factor [TNF]-α, interleukin [IL]-1b, and IL-6) and decreasing eosinophil and neutrophil activity in CRS with nasal polyposis.28 Benefit has been shown with short (<3 weeks) and long (12 weeks) courses of doxycycline, typically administered at a 100 mg daily dose. Common side effects include gastrointestinal upset (e.g. nausea, vomiting, abdominal pain, diarrhoea) and skin reactions (e.g. rash, pruritis, photosensitivity), particularly the increased susceptibility to sunburn.28 Enamel hypoplasia and teeth discolouration has been a historic concern; however, due to the reduced calcium binding of doxycycline compared with other tetracyclines, this risk is extremely low, and up to a 21-day course of doxycycline in children of any age is supported by the American Academy of Paediatrics.29
Macrolides have antineutrophilic and anti-inflammatory (TNF-α, IL-8) properties, with greatest benefit demonstrated in Th1-mediated noneosinophilic CRS (nontype 2 CRS).1,30 Dose appears to be less significant than duration of treatment, and a minimum 12-week course is recommended to determine response.28 Before initiation, a thorough cardiac history and baseline ECG are recommended as macrolides can cause a prolonged QT interval and lead to the torsades de pointes arrhythmia.
Nasal saline irrigation
Nasal irrigation with isotonic saline or Ringer’s lactate is effective in patients with CRS. Irrigation can provide symptomatic relief and serve as a medium for delivery of INCS. The addition of baby shampoo, honey or dexpanthenol, as well as high temperatures and high salt concentrations, have not been shown to confer an additional benefit.1 Head position during irrigation can impact on saline distribution, with head positioned down providing improved penetration of the frontal sinuses.31
Other medical therapies
Immunotherapy is a primary treatment for patients with CCAD and can be initiated pre- or postoperatively to achieve durable symptom relief. Postoperative aspirin desensitisation can be considered in cases of NERD to reduce symptoms in those who need revision functional endoscopic sinus surgery (FESS), in those who require systemic corticosteroids and to improve asthma and respiratory control. For CRS alone, antihistamines, decongestants, antifungals and proton pump inhibitors have not been shown to have significant benefit and are not recommended.1 However, benefit may be seen on a case-by-case basis depending on comorbidities.
Surgery
The endoscope has revolutionised modern surgical management of acute and chronic, benign and malignant sinonasal disease. Straight and angled endoscopes and instruments permit reach into previously difficult-to-access regions, with clear delineation of anatomy and disease, and minimal intra- and postoperative morbidity. Intraoperative surgical navigation has further improved safety and fostered surgical innovation to address intracranial and intraorbital disease via an endonasal endoscopic approach.
The term functional endoscopic sinus surgery was coined to reflect operative objectives of disease eradication and creation of a functional sinonasal cavity that incorporated the natural sinus ostia, allowed adequate sinus ventilation, facilitated mucociliary clearance and enabled instillation of topical therapies. In this regard, FESS involves removal of the bony sinus partitions that obscure the natural, narrow (<2 to 3 mm) sinus drainage pathways, to create wide openings to achieve the aforementioned objectives. The extent of surgery is tailored to the patient’s anatomy and distribution and severity of disease. Complications include postoperative bleeding, infection, scarring and disease recurrence that may necessitate revision surgery. Major complications are extremely rare (<1%) but include skull base breach and cerebrospinal fluid leak, nasolacrimal and orbital injury, anosmia and major vessel bleeding (carotid artery).
Underlying septal deformities and turbinate hypertrophy are often addressed concurrently with FESS to provide an unobstructed nasal passage for breathing and delivery of topical medications.
Biological therapy
Since 2019, biological therapy has entered the CRS management paradigm for select patients with refractory disease despite maximal medical and surgical therapy (Box 4). Biological therapy has shown efficacy in reducing nasal symptoms (congestion, rhinorrhoea, hyposmia, postnasal drip) and polyp scores. Predicated on our understanding of the united airway and their established role in severe asthma, the following monoclonal antibodies target factors driving the type 2 inflammatory pathway:
- dupilumab (IL-4/IL-13)
- mepolizumab (IL-5)
- reslizumab (IL-5)
- benrazlizumab (IL-5 receptor)
- omalizumab (IgE).
However, cost effectiveness remains a concern. Although dupilumab, mepolizumab and omalizumab are TGA approved for CRS, they are not PBS listed and, as such, patients can expect to incur costs exceeding $1500 per month for treatment.
Refractory CRS
Despite optimal medical and surgical management, some patients may continue to experience significant symptoms of CRS and demonstrate nasal polyp recurrence. In such cases, factors to consider include:
- patient compliance with postoperative and maintenance management
- smoking and recreational drug use
- occupational chemical exposure
- alternative diagnoses (e.g. odontogenic sinusitis, AFRS, granulomatous and autoimmune conditions, CF, PCD, NERD, Samter’s triad)
- exacerbating comorbidities (e.g. allergic rhinitis, asthma, laryngopharyngeal reflux)
- surgical factors, such as unaddressed sinuses, missed natural sinus ostia (predisposing to a recirculation phenomenon), scarring and cicatrisation, middle turbinate lateralisation, and sumping and mucostasis.
Repeat CT imaging and a more exhaustive panel of investigations, including skin prick allergy testing, an autoimmune and vasculitic screen and histopathological assessment for CRS endotype, ciliary abnormalities and granulomatous conditions, can be considered. Systemic corticosteroids and a prolonged course of doxycycline or macrolide antibiotics can be trialled as a means of medical salvage. Multidisciplinary input from an immunologist and/or a respiratory physician for immunotherapy, aspirin or fungal desensitisation, biological agents and management of lower airway disease if present may be required. If unsuccessful, revision surgery with more extensive FESS, including medial maxillectomy and modified endoscopic Lothrop procedures, could be considered.
Paediatric CRS
The definition of paediatric CRS differs slightly from adults in that cough replaces hyposmia or anosmia as a cardinal symptom.1 Prevalence is estimated to be 2% and is reported to have a greater impact on QoL than asthma and juvenile arthritis.32 The aetiology is multifactorial and includes immune function immaturity; viral, bacterial and fungal infection; allergy; adenoiditis; environmental factors (e.g. cigarette smoke exposure, daycare attendance); and systemic disorders (e.g. CF, PCD).
Clinical features include nasal obstruction or congestion, anterior and posterior rhinorrhoea, cough, facial pain or pressure, hyposmia or anosmia, fever, irritability, headaches, halitosis, fatigue, dental pain, ear pain/pressure/fullness and nasal polyps. Paediatric-specific differential diagnoses include adenoiditis, intranasal foreign body, choanal atresia or stenosis, CF and PCD. Initial investigations include allergy testing and swabs of nasal discharge for culture-directed antibiotic therapy. Plain x-rays have a limited role; however, lateral views can assess adenoid size. CT (or MRI) is reserved for patients who do not respond to treatment or if surgery is considered. Additional investigations include genetic and sweat testing for CF and haematology for immunodeficiency. Given the rarity of nasal polyps in children, all presenting with such should undergo investigation for CF. The diagnosis of PCD requires mucosal biopsy.
First-line management with nasal saline irrigation and INCS is recommended. In the absence of acute bacterial suprainfection, there is no robust evidence to support the use of short- or long-term topical, oral or intravenous antibiotics. However, small retrospective series have reported success with long-term (four weeks or greater) culture-directed intravenous antibiotics following surgery.1 Treatment with systemic corticosteroids tapered over 30 days and combined with amoxicillin and clavulanate was shown to be beneficial in improving symptoms, CT scores and relapse rates compared with amoxicillin and clavulanate treatment alone.33 Antihistamines, decongestants and antileukotrienes are not recommended.34
Adenoidectomy is typically the first surgical intervention and provides symptom resolution in about 50% of cases.1 Research has shown adenoids (of any size) to harbour pathogenic bacteria, with biofilm formation present in over 80% of paediatric patients with CRS. Maxillary sinus (antral) lavage can be performed concurrently to obtain specimens to guide antibiotics and is recommended in children with comorbid asthma who have more severe disease on preoperative CT.1 There is a high-rate concordance of cultures obtained from the adenoids, middle meati and maxillary sinus. FESS can be performed as the primary surgical intervention, or after adenoidectomy, with symptom reduction, minimal morbidity and no clinically significant impact on facial growth seen in almost 90% of patients.35 Balloon sinuplasty may have a role in paediatric CRS treatment, by providing greater intraoperative access than antral lavage with less postoperative care required than FESS due to increased tissue preservation.36
Role of the GP
GPs have an important role in the management of adult and paediatric patients with CRS (Box 5). Through history taking, examination and appropriate investigations, an accurate provisional diagnosis can be made and CRS differentiated from conditions with overlapping symptoms. Medical management in the form of saline irrigation, INCS and short courses of oral corticosteroids can be initiated, and education provided on the natural history of CRS and compliance with therapy. Low (or ultra low) dose, noncontrast CT of the paranasal sinuses is a noninvasive investigation with minimal radiation exposure that can assist with diagnosis and should be performed before referral. Specialist referral is recommended if symptoms persist or recur, or red flag features are evident on presentation, so that a correct diagnosis can be established and a treatment plan formulated.
Conclusion
CRS is a heterogeneous disorder that can develop in patients of all ages. Endotyping and phenotyping enables appropriate patient counselling regarding their disease and implementation of tailored, stepwise, medical and surgical interventions to alleviate symptoms and improve QoL. MT
COMPETING INTERESTS: None.
