Nonsurgical body contouring with energy devices

Noninvasive technologies aimed at body contouring, which target fat reduction, skin tightening and muscle reduction, have become increasingly available in the past decade. As many of these technologies are considered ‘cosmetic’, they are exempt from regulatory oversight. Appropriate patient selection, adherence to precautions and awareness of the potential adverse effects are key to achieving satisfactory patient outcomes.
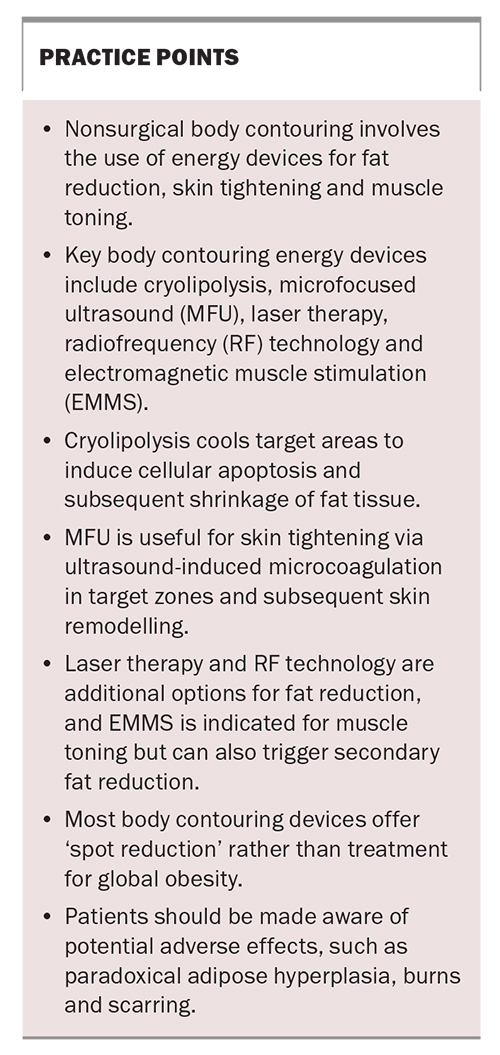
Over the past decade, there has been a proliferation of noninvasive body contouring devices for fat reduction, skin tightening and muscle toning. Cryolipolysis, microfocused ultrasound (MFU), laser therapy, radiofrequency (RF) technology and electromagnetic muscle stimulation (EMMS) are the current therapeutic options for nonsurgical body contouring.1,2 Many of these options are nonlaser-based technologies and considered ‘cosmetic’ and, therefore, are exempt from TGA regulation. Consequently, body contouring energy devices are popular with patients and consumers in both medical and nonmedical (e.g. beauty and fitness industries) settings.
With device-based fat reduction, patients must understand that fat loss is localised to the device application areas for ‘spot reduction’ rather than global weight reduction. Appropriate patient selection is a prerequisite for satisfactory patient outcomes, as device-based fat reduction is not suitable for patients with a high body mass index (BMI) or global obesity, which should be managed initially through changes in diet and exercise. This article discusses key body contouring technologies, outlining how they work, their main indications and potential adverse effects.
Cryolipolysis
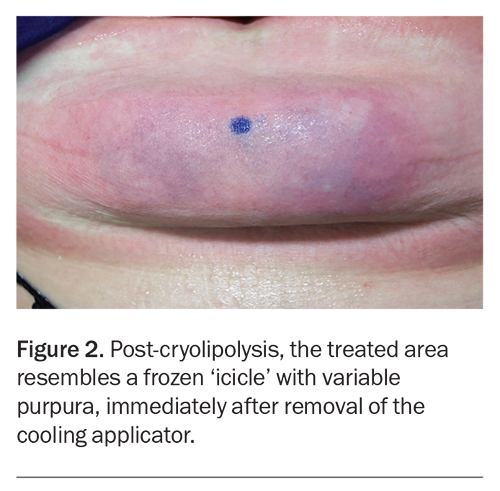
Cryolipolysis, first described in 2008, is one of the most studied and utilised methods for body contouring.3 It is a noninvasive method of ‘fat freezing’ that uses cold temperatures to selectively destroy subcutaneous fat and visibly reduce localised fat bulges without surgery.3 Cooling applicators in the shape of suction cups, in conjunction with a skin-protective gel pad, are applied to the treated area at a target temperature of –7°C to 1°C for a set time of 45 to 90 minutes.4 The low temperature induces lobular panniculitis (inflammation of subcutaneous fat), followed by apoptosis of fat cells, resulting in a reduction of skin fat (Figure 1). The appearance of the treated area after removal of the suction cup is a firm ‘icicle’ roll that may show variable purpura (Figure 2). The treated area is firmly massaged for several minutes until it softens and thaws. The same areas can be re-treated after two to three months. Typically, one to three treatments are required for optimal results in patients with an ideal body weight.
During the treatment, patients may experience initial tingling, stinging and aching due to the intense cold. Following the treatment, patients should expect mild temporary bruising, swelling and sensory changes. Dysaesthesia can occur in up to 73% of patients and last for three weeks, although it may persist for up to three months in 18% of patients.5 The dysaesthesia is self-limiting, and peripheral nerve biopsy and confocal microscopy show no alterations in the neural network.6 Cryolipolysis is not associated with alterations in serum lipid levels and liver function.7
Paradoxical adipose hyperplasia (PAH) is an uncommon but disfiguring complication where the treated area increases in size and is firm, lumpy and occasionally tender on palpation. PAH typically occurs within three to six months following cryolipolysis and requires liposuction or surgical excision to rectify, as the condition will not resolve spontaneously.8,9 In a study of 2114 patients who underwent 8658 treatment cycles of cryolipolysis, nine patients developed PAH.9 Most cases of PAH occurred after the first treatment session, although PAH can develop for the first time after two or three treatment cycles. This idiosyncratic adverse effect can occur on any treated site and occurs more commonly in men at an estimated frequency of between one in 2000 to one in 4000 treatment cycles.9 Newer unit and application models have shown a reduction in the occurrence of PAH, suggesting that mechanical issues in older models may have been a contributing factor.9
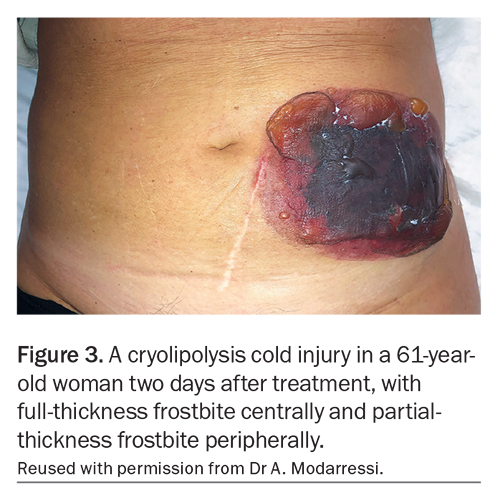
As a nonlaser-based technique, cryolipolysis is exempt from laser regulations. The technology delivers reproduceable results, making it a popular body contouring option in both medical and non-medical or retail settings. The correct use of protective gel pads is vital to prevent cold injury (frostbite) from the cold suction cups (Figure 3). Third-degree cold injuries can occur as a result of protocol deviations, such as reusing gel pads that are strictly for single use, using homemade gel pads, substituting proprietary gel pads with non-TGA-approved alternatives or using ultrasound gel as a substitute gel.
The following precautions must be taken when performing cryolipolysis:
- avoid treating over hernias
- avoid treating individuals with cold sensitivities, such as those with
- Raynaud’s disease
- cryoglobulinaemia
- cold agglutinin disease
- cold urticaria
- avoid treating individuals with global obesity
- avoid treating individuals who are pregnant or lactating.
Microfocused ultrasound
MFU targets the superficial musculoaponeurotic system (facelifting plane) for more natural and durable skin tightening. The delivery of MFU is not associated with epidermal injury and, therefore, does not require any recovery or downtime. The focused and precise energy delivery is associated with significantly fewer adverse effects, such as burns, blisters and diffuse heating with collateral damage to the adjacent epidermis or adipose tissue. Increasing the ultrasonic focal depth can target subcutaneous fat more selectively to achieve fat reduction.
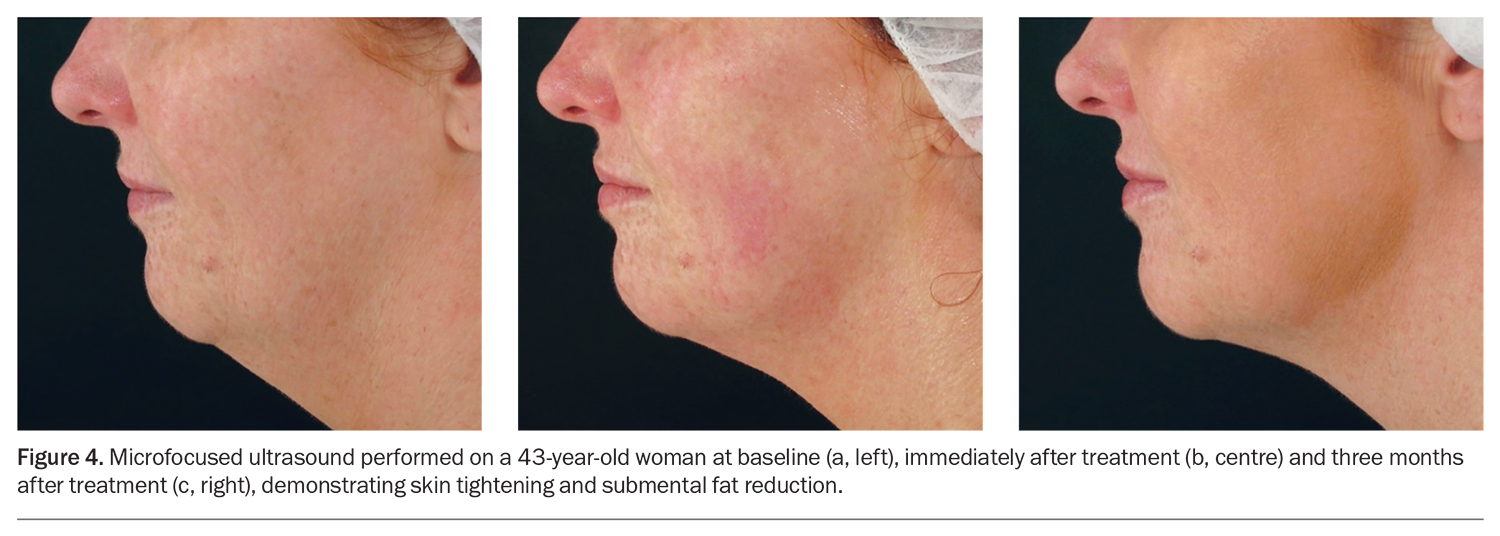
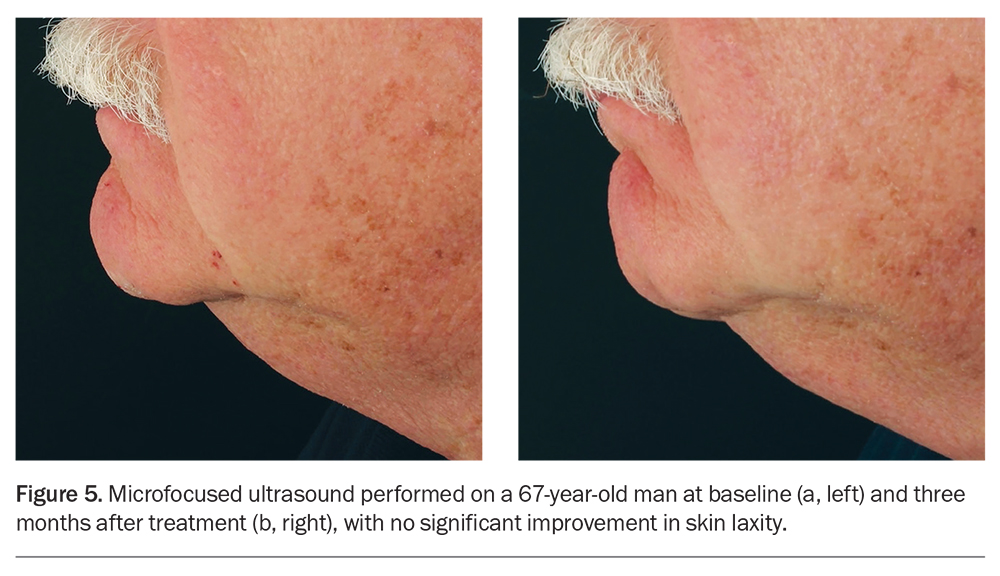
The MFU device uses ultrasonic energy to achieve precise microcoagulation zones (i.e. coagulative necrosis) deep in the dermis, subcutaneous adipose tissue and superficial musculoaponeurotic system.1,4 During the months following treatment, repair of the MFU-induced deep tissue injury leads to contraction and tissue remodelling, resulting in the desired aesthetic effect of skin tightening (Figure 4).1,4 The superficial dermis and collateral tissues are spared, which not only limits scarring and downtime, but potentially permits MFU to be used for coloured or darker skin types. However, in common with all tissue- heating options for skin tightening, interindividual variations in the response to MFU treatment are significant. Studies have shown that MFU can visibly improve skin laxity in more than 80% of cases.4,10 However, in our experience, up to 25% of patients may not perceive an improvement (Figure 5). Individuals with a high BMI, excessive skin laxity or advanced age may not respond adequately to skin-tightening procedures. Hence, preprocedural counselling to establish realistic expectations and judicious patient selection are key to achieve patient satisfaction.
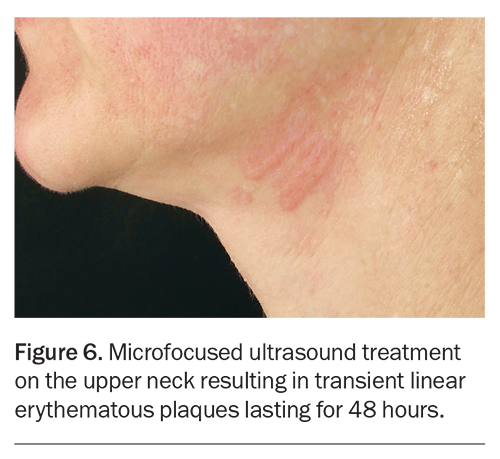
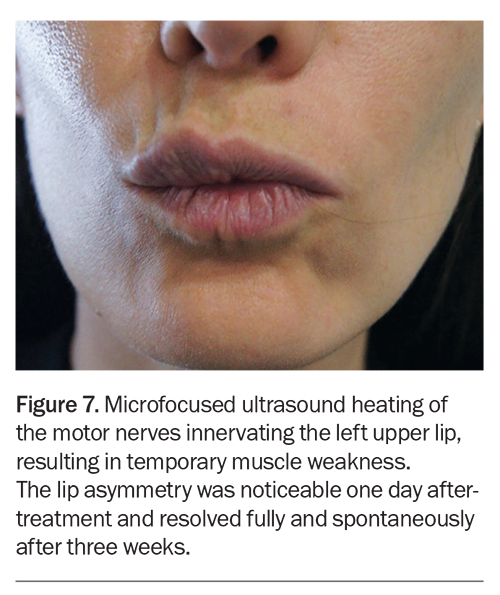
The safety of MFU is well established, with a very low reported incidence of adverse events.1 Overheating of the skin with inappropriately high energy settings can result in blisters and reticulate scars, but the associated pain will usually prevent this from happening and, indeed, there are no reports of MFU-related scarring.1 Patients may experience transient mild linear erythematous plaques (Figure 6), but these generally last for less than 24 hours. Lesions persisting for longer than 24 hours will resolve fully and promptly with the use of topical steroids. When linear plaques become noticeable during treatment, a decrease in fluence is recommended. Patients may also experience transient thermal neuropraxia from collateral MFU heating of the motor nerves, resulting in temporary muscle weakness (Figure 7). Any branch of the facial nerve may be susceptible; however, the temporal nerve (temple) and marginal mandibular nerve (lateral chin and jawline) are more vulnerable to thermal neuropraxia and are ‘caution areas’ during MFU therapy. Uncommonly, transient sensory thermal neuropraxia presenting as tingling and numbness may occur.
The following precautions must be taken when performing MFU:
- avoid setting unrealistic expectations
- avoid treatment if the individual’s target event is within three months (to avoid transient facial muscle weakness)
- avoid treating individuals who are pregnant or lactating.
Laser therapy
Laser therapy with a wavelength of either 635 nm or 1060 nm has been used for body contouring. The 635 nm laser is delivered as a noncontact, low-intensity laser that nonthermally disrupts adipocytes by creating temporary microscopic openings within their cell membranes, allowing lipids to leak out without apoptosis (low-level laser therapy). The absence of adipocyte apoptosis calls into question the permanence of this method of fat reduction.1,2 The more recently introduced 1060 nm laser is a contact device (with contact cooling) that can be applied to multiple areas of the body to cause heat-induced adipocyte apoptosis and subsequent fat loss. The exposure time is typically 20 to 30 minutes and requires two to 12 treatment sessions.1 Mild to moderate pain may result from tissue heating with the 1060 nm laser. Like cryolipolysis, there is no detectable elevation in serum lipid levels during the treatment.1,2 Laser lipolysis has a favourable safety profile, with no reports of skin burns, scarring or pigmentary changes.1,2 More recently, devices that combine both wavelengths have been developed with good safety and efficacy.11
The following precautions must be taken when performing laser therapy:
- avoid setting unrealistic expectations
- avoid treating over
– tattoos
– scars
– abdominal hernias
– metal implants - avoid treating individuals who are pregnant or lactating.
Radiofrequency technology
RF devices contour the body through volumetric heating of the skin and subcutaneous tissue via applied electrical fields interacting with the inherent target tissue electrical resistance, in accordance with Ohm’s law.4 The heat induces collagen contraction and remodelling, resulting in the desired clinical endpoint of skin tightening. Stimulation of regional blood flow and improved lipolysis is thought to account for the beneficial effects seen in the treatment of cellulite.4 The epidermis is spared from thermal damage by contact cooling.
Early devices were uncomfortable and time consuming to administer and delivered inconsistent results; however, advances in handpiece design, together with the use of bipolar (and tripolar or multipolar) RF, have improved efficacy and patient comfort.1,4 The adverse effect profile of RF is favourable, with transient erythema and oedema occurring commonly but blistering, scarring and contour changes occurring rarely and only with aggressive parameters.1,4 RF can also be directed into the subcutaneous tissue to achieve localised fat reduction, with multiple treatment sessions yielding better results.1,4
The following precautions must be taken when using RF technology:
- avoid setting unrealistic expectations
- avoid treating individuals with pacemakers and defibrillators
- avoid treating individuals who are pregnant or lactating.
Electromagnetic muscle stimulation
EMMS has been used for several decades in sports and rehabilitation therapy and is a more recent entry into the body contouring sphere. EMMS devices deliver high-intensity, focused electromagnetic stimulation to target muscles, with an indirect effect on adjacent fat.1,2 Multiple stimulated contractions occur with subsequent strengthening and hypertrophy of the treated muscles. Repetitive muscular contractions are also associated with secondary fat loss over the treated areas.1,2 The typical target areas are the buttocks and abdomen, and the EMMS applicator pads can be either directly applied on the abdomen or incorporated into a seat to target the buttocks and perineum. The device is popular for toning and sculpting the abdominal area and buttocks, as well as improving muscular definition through associated fat loss over the treated sites. EMMS has also been promoted as an effective noninvasive treatment option for female pelvic floor dysfunction.12
The treatment involves at least four 30-minute sessions spread evenly over the course of two weeks. Following this, one treatment every three to six months is recommended to maintain the results. The strength of the contractions can be adjusted from 0 to 100%. Although well tolerated by most individuals, some may experience painful spasm-like discomfort; individuals with a high BMI may not notice visible results, which has been quantified as up to a 15% reduction in fat and 19% increase in muscle thickness.2
The following precautions must be taken when performing EMMS:
- be aware that a cramp-like sensation may occur that can be intolerable to some individuals
- avoid treating individuals who have a high BMI
- avoid setting unrealistic expectations
- avoid treating individuals who are pregnant or lactating.
Vaginal recontouring: a cautionary tale
Since 2016, there has been a rapid uptake of vaginal ‘rejuvenation’ procedures with re-tooling of the existing energy-based technologies, such as fractional ablative lasers (CO2 or Erbium:YAG) and fractional RF.13 In this procedure, the laser or RF energy is delivered to the wall of the vaginal vault via a probe inserted into the vaginal cavity. Vaginal rejuvenation is the umbrella term for procedures undertaken to increase vaginal tone and reverse genitourinary syndrome of menopause (GSM), which involves symptoms such as vaginal dryness, dyspareunia and urinary incontinence.13 The popularity of vaginal rejuvenation was bolstered by early case reports and uncontrolled studies showing post-procedure clinical and histological improvements in women with GSM.14,15
In 2018, following three cases of third-degree vaginal laser burns, the FDA issued a warning that vaginal therapies can have serious adverse events and lacked evidence of clinical efficacy.16 This FDA statement appeared after several consensus papers recommending similar caution because of the lack of high-quality, unbiased studies.17-19 In 2021, a New Zealand-based prospective study including 85 randomised participants comparing vaginal laser therapy with placebo (laser with sham parameters) found no difference between the two groups.20 This prompted an editorial call for a ‘pause’ on the use of vaginal lasers.16
Although cosmetic devices (lasers and other energy devices) require regulatory approval (e.g. FDA, TGA), they are held to a lower standard than therapeutic drugs.21 Consequently, the promotion and uptake of novel devices, such as energy-based vaginal laser therapies, can precede evidence-based studies by some years before reliable data are available to adequately inform and guide stakeholders. In the case of vaginal energy-based device therapies for GSM, after several years of hype and intervention, evidence has subsequently emerged that the procedure may not benefit patients and can be associated with significant costs and potential morbidity.20
In the past few years, cosmetic procedures have featured prominently on social media through the confluence of industry (laser vendors), consumers (‘influencers’) and providers (‘TikTok doctors’). Following a series of well-documented breaches in liposuction health regulatory standards resulting in patient harm in 2021 and 2022, the Australian Health Practitioner Regulation Agency has published a set of surgical and nonsurgical cosmetic procedural guidelines to assist practitioners in meeting minimum safety standards and providing ethical patient care.22,23 The guidelines cover body dysmorphia screening, informed consent, information about complaint avenues, continuing professional development requirements, financial consent and advertising.23
Conclusion
Energy devices for fat reduction, skin tightening and muscle toning are popular with patients and consumers and are available in medical clinics, beauty salons and health spas. These devices can assist with ‘spot reduction’ of specific areas resistant to diet and exercise. Although generally safe, energy devices can lead to significant tissue injury, such as burns and frostbite, or persistent complications, such as cryolipolysis-induced PAH. Patients should be made aware of potential adverse effects, such as paradoxical adipose hyperplasia, burns and scarring. Practice points for GPs are provided in the Box. MT
COMPETING INTERESTS: Dr Patel: None. Conjoint Professor Sebaratnam has received payment or honoraria from Abbvie, Galderma, Novartis, Pfizer, Janssen-Cilag, LEO Pharma, Sun Pharmacentical Industries and Viatris; has received support for attending meetings and/or travel from Galderma; has been a Board Member for Novartis; has contributed to the Australasian College of Dermatologists’ General Practitioner Taskforce; and has received support from Syneron Candela Corporation Australia Pty Ltd and HEINE Optotechnik. Dr Lim is a member of the Australian Medical Council Cosmetic Surgery Technical Advisory Group; is Board Director of the Australasian College of Dermatologists; and holds stocks in EBOS Australia. Dr Lim’s partner is a paid advisor for the aesthetic device division of EBOS Australia.
References
1. Mazzoni D, Lin MJ, Dubin DP, et al. Review of non-invasive body contouring devices for fat reduction, skin tightening and muscle definition. Australas J Dermatol 2019; 60: 278-283.
2. Murgia RD, Noell C, Weiss M, et al. Body contouring for fat and muscle in aesthetics: Review and debate. Clin Dermatol 2022; 40: 29-34.
3. Manstein D, Laubach H, Watanabe K, et al. Selective cryolysis: a novel method of non-invasive fat removal. Lasers Surg Med 2008; 40: 595-604.
4. Stewart N, Lim AC, Lowe PM, et al. Lasers and laser-like devices: part one. Australas J Dermatol. 2013; 54: 173-183.
5. Garibyan L, III WS, Jillian H, et al. Three-dimensional volumetric quantification of fat loss following cryolipolysis. Lasers Surg Med 2014; 46: 75-80.
6. Coleman S, Sachdeva K, Egbert B, et al. Clinical efficacy of noninvasive cryolipolysis and its effect on peripheral nerves. Aesthetic Plast Surg 2009; 33: 482-488.
7. Klein KB, Zelickson B, Riopelle JG, et al. Non-invasive cryolipolysis for subcutaneous fat reduction does not affect serum lipid levels or liver function tests. Lasers Surg Med 2009; 41: 785-790.
8. Singh SM, Geddes ER, Boutrous SG, et al. Paradoxical adipose hyperplasia secondary to cryolipolysis: An underreported entity? Lasers Surg Med 2015; 47: 476-478.
9. Nikolis A, Enright KM. A multicenter evaluation of paradoxical adipose hyperplasia following cryolipolysis for fat reduction and body contouring: a review of 8658 cycles in 2114 patients. Aesthet Surg J 2021; 41: 932-941.
10. Alam M, White LE, Martin N, et al. Ultrasound tightening of facial and neck skin: a rater-blinded prospective cohort study. J Am Acad Dermatol 2010; 62: 262-269.
11. Moon IJ, Choi JW, Jung CJ, et al. Efficacy and safety of a novel combined 1060-nm and 635-nm laser device for non-invasive reduction of abdominal and submental fat. Lasers Med Sci 2022; 37: 505-512.
12. Dolman M. Electromuscular stimulation for urinary incontinence: Levator 100. Br J Community Nurs 2000; 5: 214-215, 217-220.
13. Tadir Y, Gaspar A, Lev-Sagie A, et al. Light and energy based therapeutics for genitourinary syndrome of menopause: consensus and controversies. Lasers Surg Med 2017; 49: 137-159.
14. Zerbinati N, Serati M, Origoni M, et al. Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment. Lasers Med Sci 2015; 30: 429-436.
15. Gambacciani M, Palacios S. Laser therapy for the restoration of vaginal function. Maturitas 2017; 99: 10-15.
16. Adelman M, Nygaard IE. Time for a "pause" on the use of vaginal laser. JAMA 2021; 326: 1378-1380.
17. Preti M, Vieira-Baptista P, Digesu GA, et al. The clinical role of LASER for vulvar and vaginal treatments in gynecology and female urology: An ICS/ISSVD best practice consensus document. Neurourol Urodyn 2019; 38: 1009-1023.
18. Digesu GA, Tailor V, Preti M, et al. The energy based devices for vaginal "rejuvenation," urinary incontinence, vaginal cosmetic procedures, and other vulvo-vaginal disorders: an international multidisciplinary expert panel opinion. Neurourol Urodyn 2019; 38: 1005-1008.
19. Romero-Otero J, Lauterbach R, Aversa A, et al. Radiofrequency-based devices for female genito-urinary indications: position statements from the European Society of Sexual Medicine. J Sex Med 2020; 17: 393-399.
20. Li FG, Maheux-Lacroix S, Deans R, et al. Effect of fractional carbon dioxide laser vs sham treatment on symptom severity in women with postmenopausal vaginal symptoms: a randomized clinical trial. JAMA 2021; 326: 1381-1389.
21. Van Norman GA. Drugs, devices, and the FDA: part 2: an overview of approval processes: FDA approval of medical devices. JACC Basic Transl Sci 2016; 1: 277-287.
22. Carroll L. Top doctors back calls for crackdown on cosmetic surgery ‘cowboys’. The Sydney Morning Herald April 22 2022.
23. Independent review of the regulation of medical practitioners who perform cosmetic surgery. Melbourne: Australian Health Practitioner Regulation Agency; 2022. Available online at: https://www.ahpra.gov.au/News/Cosmetic-surgery-independent-review-of-patient-safety.aspx (accessed Aug 2023).