Laser skin resurfacing – more than a cosmetic procedure

Ablative lasers are used for skin resurfacing to promote tissue remodelling and skin rejuvenation, with advancements in technology leading to safer devices, including fractional delivery systems. Common indications for treatment with ablative fractional lasers include photoageing, the appearance of lines and wrinkles, actinic dysplasia, acne and burn scars, and benign facial papules. Patients must be informed of the potential adverse effects of laser skin resurfacing, as well as the postprocedure recovery process.
Ablative lasers vaporise layers of skin to induce tissue remodelling and subsequent skin rejuvenation. Over the years, technological improvements have led to safer devices, such as those yielding fractional delivery with both cosmetic and medical indications. This article provides an overview of the types of lasers used for skin resurfacing, as well as some indications and complications of this procedure.
Evolution of laser devices used for skin resurfacing
The classic ablative lasers are the carbon dioxide (CO2) and erbium:yttrium-aluminium-garnet (erbium:YAG) lasers. The CO2 laser was the first ablative laser, introduced almost 60 years ago, and became a popular skin resurfacing tool for wrinkles and scars from the 1990s.1 The erbium:YAG laser was introduced in the mid-1990s and was rapidly established as a versatile resurfacing laser because of its capability of vapourising tissue with less collateral damage than the CO2 laser. Both the CO2 and erbium:YAG lasers remain popular resurfacing lasers today.
CO2 versus erbium:YAG ablative lasers
The CO2 laser emits infrared radiation at a wavelength of 10,600 nm, mainly targeting water. The laser facilitates tissue ablation and underlying tissue coagulation. The erbium:YAG laser delivers a wavelength of 2940 nm with an at least 10-fold greater affinity for water compared with the CO2 laser.2 The erbium:YAG laser also produces more superficial ablation per pass with less thermal coagulation, resulting in shorter healing times and less post-treatment erythema and postinflammatory hyperpigmentation. Conversely, a reduction in thermal heating is correlated with reduced haemostasis and less impressive skin tightening with erbium:YAG laser resurfacing.3
In the early days, the energy delivery of the CO2 laser was continuous, with crude control of the energy output resulting in frequent overheating and burns. The development of pulsed technology allows for enhanced control of the energy output and a reduction in complications, making CO2 resurfacing of the full face safer. However, erbium:YAG lasers can be manipulated to incorporate subablative pulses to increase residual thermal heating and improve the skin-tightening effects. The advent of fractional laser technology in the mid-2000s reinvigorated skin resurfacing by further reducing the procedural downtime and potential complications of ablative lasers.4
Fractional lasers
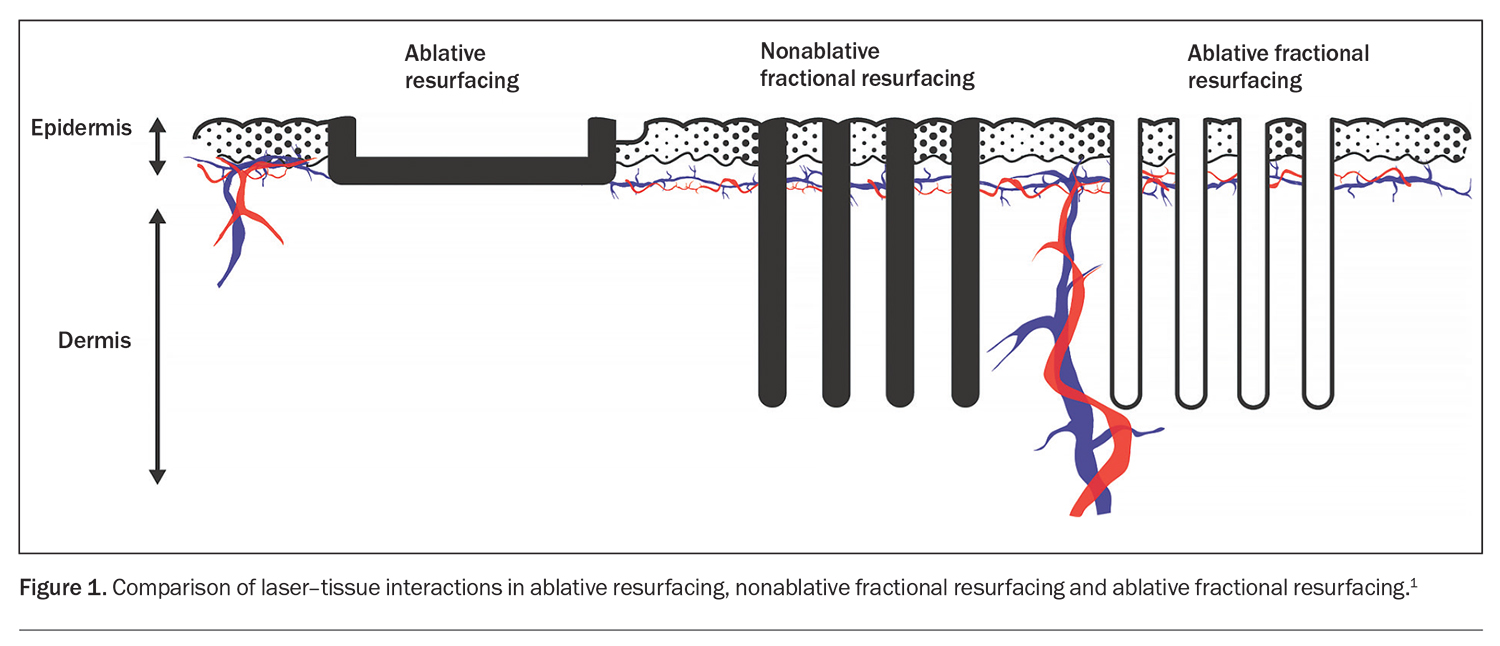
Fractional laser devices deliver microchannels of energy to the skin with intervening areas of untreated tissue. The microchannels are known as microthermal zones and can penetrate depths of up to 1.5 mm and a width of 100 to 400 mcm, with up to 6400 microchannels per cm2 (Figure 1).1,4 Typically, only 5 to 20% of the surface area is targeted. The normal intervening skin acts as a reservoir for tissue regeneration by providing nutritional support and an intact microstructure for keratinocyte and fibroblast migration.
The 1550 nm nonablative laser was the first fractional device to appear on the market in the mid-2000s and is still widely used today. Other popular nonablative fractional lasers include the 1927 nm wavelength laser and lasers with wavelengths between 1320 and 1550 nm.1,4 The inherent advantages of nonablative fractional lasers include short recovery times; improved patient tolerability; and their suitability as an ideal adjunct to other procedures, such as intense-pulsed-light and vascular lasers. In the late 2000s, the classic ablative lasers – CO2 and erbium:YAG – were reconfigured as fractional laser devices, giving the ablative lasers a new lease of life for skin rejuvenation treatments.
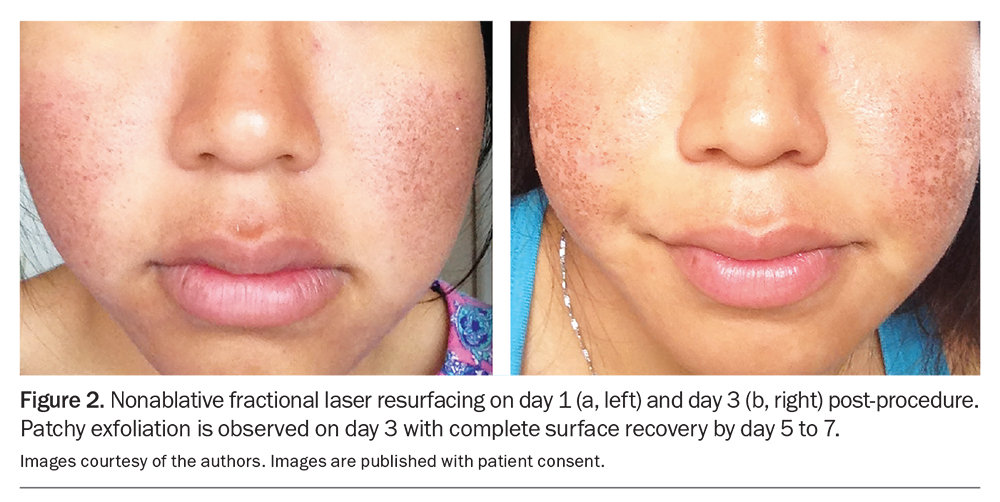
Ablative fractional lasers are more effective than their nonablative fractional counterparts, with greater improvements in collagen remodelling and skin tightening, but with longer recovery times and more potential adverse effects, such as persistent erythema and postinflammatory hyperpigmentation, although these adverse effects are significantly reduced when compared with traditional non-fractional ablative lasers.5 Nonablative fractional lasers typically lead to erythema and oedema lasting two to three days postprocedure, followed by micro-exfoliation without bleeding or oozing (Figure 2). By comparison, ablative fractional lasers produce pinpoint bleeding for one to two days and moderate to marked erythema lasting one to three weeks. Nevertheless, ablative fractional lasers have a much more favourable side effect profile compared with their nonfractional counterparts.
Indications of laser skin resurfacing
Given their favourable efficacy and adverse effect profile, ablative fractional lasers are now considered the gold standard for skin resurfacing.1,4,6 Common indications for treatment with ablative fractional lasers include photoageing, the appearance of lines and wrinkles (rhytides), actinic dysplasia, acne and burn scars and benign facial papules.6-8
Skin rejuvenation
Since the 1990s, fully ablative laser resurfacing with the CO2 laser initially, followed by the erbium:YAG laser, has been the mainstay of therapy. With the advent of fractional lasers in the mid-2000s, the popularity of skin resurfacing has risen. In our experience, the erbium:YAG laser is best suited for fine to medium rhytides and darker skin tones on account of its superior safety profile. By comparison, the CO2 laser is better suited for deeper rhytides, with the aim of skin tightening. Fractional ablative lasers (CO2 and erbium:YAG) have an established role in the management of photoageing and rhytides and can complement other rejuvenative procedures, such as the use of injectables (e.g. botulinum toxin and fillers) and other energy devices (e.g. intense-pulsed-light and vascular lasers).9
Actinic dysplasia
Photodamage is often accompanied by actinic dysplasia, which can be improved with skin resurfacing, especially with the use of traditional ablative (nonfractional) lasers. Historically, ablative lasers, such as the CO2 and erbium:YAG lasers, have been used to treat actinic keratoses; these compare favourably with field 5-fluorouracil and trichloroacetic acid (30%) peels.10,11 Ablative lasers are generally not the first-line options for actinic dysplasia because of issues related to their access and cost. However, fully ablative (nonfractional) lasers remain a popular treatment option for actinic cheilitis (Figure 3). Laser-assisted drug delivery with fractional lasers is being implemented increasingly to create microchannels for faster and improved penetration of topical agents to increase their clinical response and efficacy (e.g. to enhance topical aminolaevulinic acid penetration in photodynamic therapy for actinic dysplasia and skin cancers).12
Scarring
Acne scars
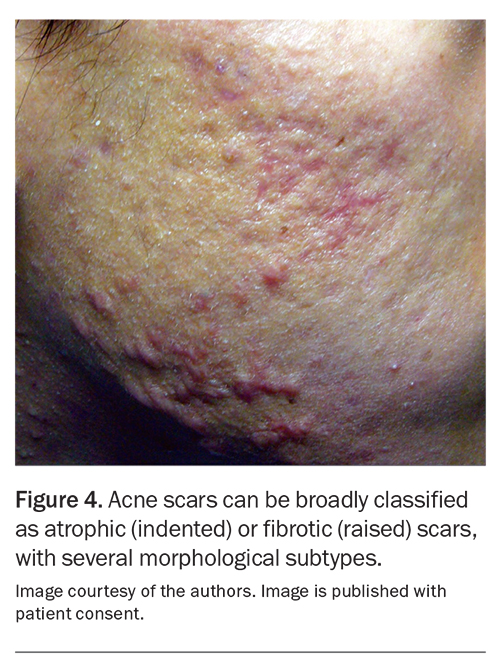
Acne scars can be broadly classified as atrophic or fibrotic scars, with several subtypes according to their morphology (Figure 4). Fractional nonablative lasers (e.g. 1550 nm) and fractional ablative CO2 and erbium:YAG lasers have been shown to improve the appearance of atrophic acne scars.7,13 A systematic review concluded that ablative fractional lasers offer an improvement range of 26 to 83%, compared with 26 to 50% for nonablative fractional resurfacing.13 Acne scarring is a key indication for fractional laser resurfacing and can be performed as a standalone procedure or in combination with traditional nonfractional resurfacing.
Burn scars
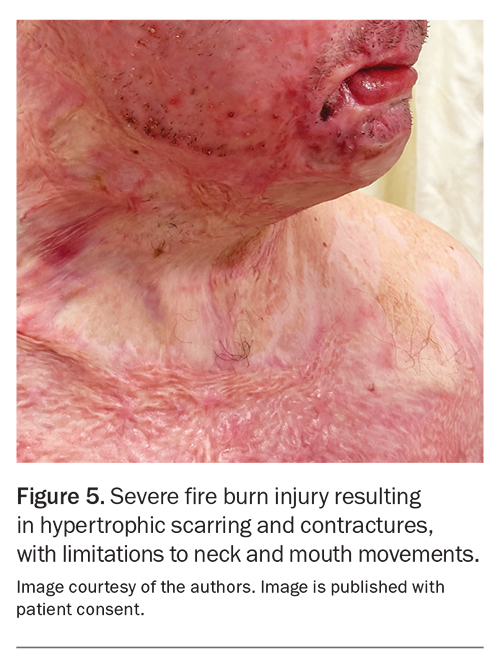
Hypertrophic burn scars can result from various thermal and caustic injuries, such as those caused by fire, scalding water, chemicals and electricity. Burn scars can result in significant functional and psychological morbidity, especially as scar contractures limit movement and with scar dysaesthesia (Figure 5). Hypertrophic burn scars are managed with physical therapies, intralesional corticosteroids, surgical revisions and fractional ablative lasers. Fractional ablative lasers can improve scar appearance and symptoms through the delivery of ablative microchannels inducing scar remodelling. A typical regimen is three sessions of fractional CO2 at one- to three-month intervals, resulting in improvements in scar pliability; texture; vascularity; pigmentation; and symptoms of itch, pain and dysaesthesia.8 Additionally, topical triamcinolone is routinely applied to the treated scar for optimum penetration (via laser-assisted drug delivery) to facilitate corticosteroid-induced scar remodelling.14
Focal ablative resurfacing
Focal or spot ablative resurfacing is commonly used for small skin lesions, typically on the face, where laser precision and control are advantageous. A constellation of benign facial papules, ranging from seborrhoeic keratosis to syringomas, can be effectively treated with spot resurfacing using ablative CO2 and erbium:YAG lasers. Depending on the device, the laser spot size can vary from smaller than 1 to 4 mm or larger, to match the size of the target lesion. Box 1 presents some considerations before referring a patient for laser spot ablation.
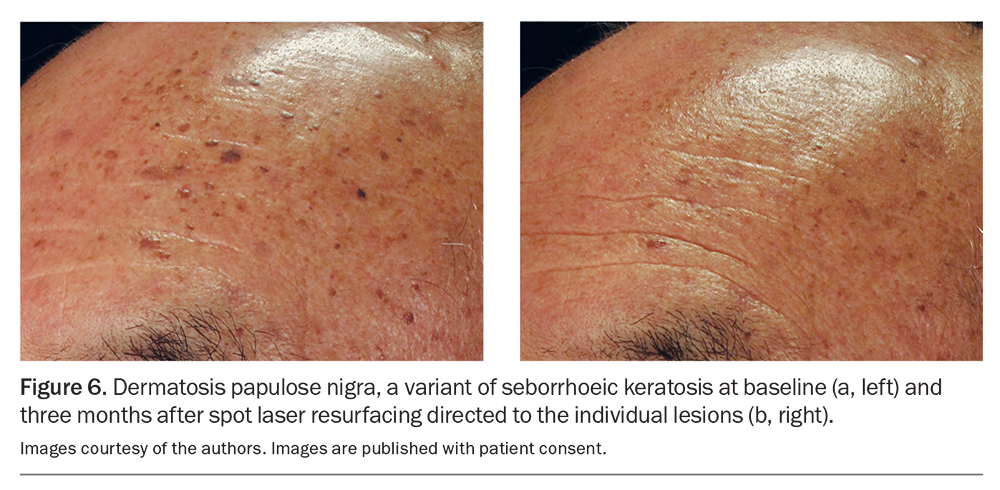
Benign facial papules
One of the most common cosmetic presentations is dermatosis papulosa nigra, a subtype of seborrhoeic keratosis (Figure 6). Many cases are amenable to cryotherapy, gentle curettage and cautery, all of which are reasonable firstline therapies. However, for cosmetically sensitive locations, such as the eyelids, nose and lips, lasers offer superior control and finesse. These growths can be treated with ablative lasers using spot sizes of 1 to 2 mm in diameter.
Other types of benign facial papules include dermal naevi, angiofibromas, sebaceous hyperplasias, syringomas (sweat duct tumours), neurofibromas and xanthelasma (cholesterol deposits), all of which are amenable to ablative laser removal. However, many of these tumours, particularly syringomas, will eventually recur, as it is not possible to completely remove the deeper portion of the lesion without the risk of scarring.
Rhinophymas
Ablative lasers can be used effectively to treat rhinophymas secondary to rosacea. A practitioner’s preference and familiarity with a particular device will determine the resurfacing modality that is used. Studies comparing laser resurfacing with electrosurgery or scalpel excision have shown similar outcomes.15 Severe rhinophyma can also be debulked efficiently using electrosurgery wire loops. Mild rhinophymas can be sculpted either using a fully ablative laser with a variable spot size (e.g. in the range of 3 to 6 mm) or high-density fractional ablative lasers, followed by a second ‘touch-up’ treatment, if required.
Complications of laser skin resurfacing
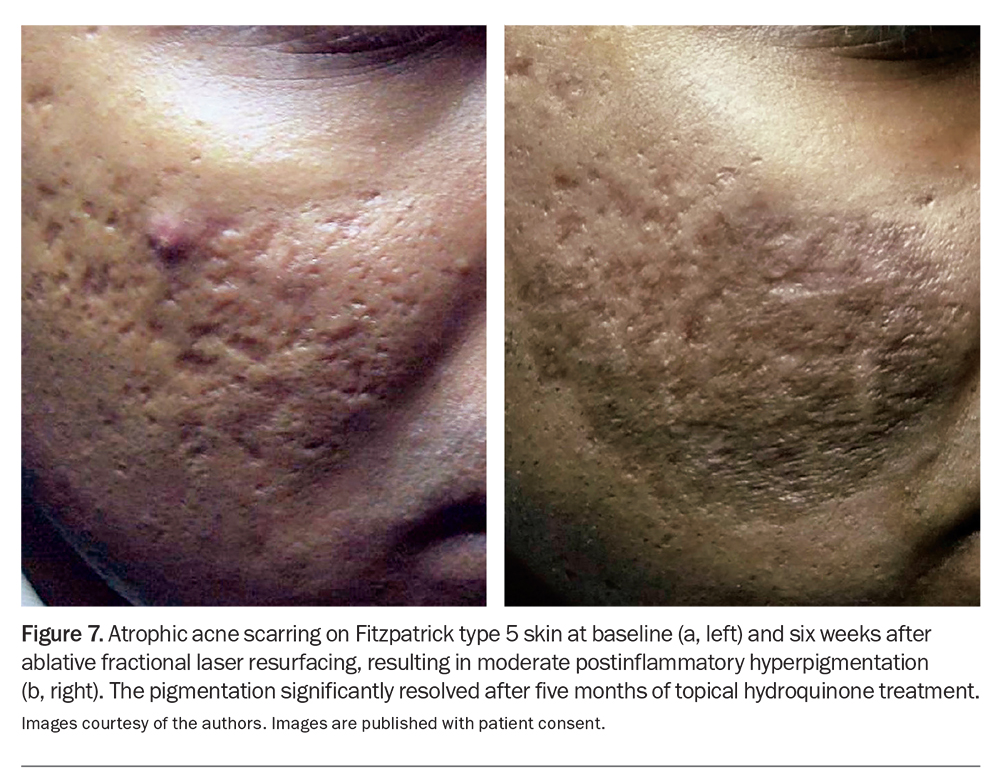
The safety of laser therapy is well established, although, as with any intervention, adverse effects are possible. Preoperative clinical review should include an evaluation of the Fitzpatrick skin phototype, recent or planned sun exposure, recent artificial tan application, immunological or inflammatory comorbidities, any history of herpes simplex virus infection, allergies, scarring, previous cosmetic or surgical procedures and the medication history for risk stratification purposes. Photograph-containing documentation before and after the procedure should be mandatory. Transient adverse effects of laser skin resurfacing include post-treatment discomfort, oozing, crusting, itching, bruising, swelling, skin sensitivity, redness and acne breakouts. Bacterial, viral and candidal infections can complicate resurfacing procedures, and prophylactic antimicrobials are often considered. Depending on the laser employed, potential longer-term sequelae include permanent hypopigmentation or prolonged hyperpigmentation (Figure 7) and, rarely, scarring. The patient’s informed consent should include detailed information of the recovery process, recovery time and after-care procedures (e.g. sun avoidance), along with a discussion of potential complications. For resurfacing procedures, patients are routinely invited to submit a series of postprocedure smartphone ‘selfies’ (Figure 8) to allow for remote monitoring for any potential complications. Box 2 presents practice tips related to informing patients about the postprocedure recovery process and aftercare monitoring process.16,17
Conclusion
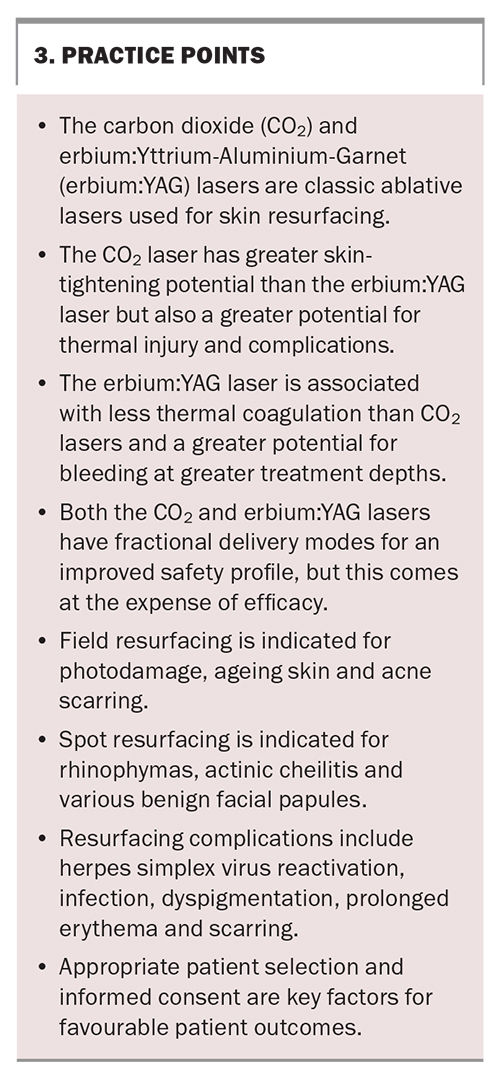
Ablative lasers for skin resurfacing remain a valuable dermatological tool for both cosmetic and medical indications. The CO2 and erbium:YAG lasers remain popular resurfacing devices and have been reimplemented in a fractional delivery mode for an improved safety profile. Nevertheless, complications, such as infections and dyspigmentation, can occur, which need to be fully discussed with patients, along with the expected recovery time for the proposed procedure. Box 3 presents some practice points for GPs. MT
COMPETING INTERESTS: Associate Professor Lowe: None. Conjoint Associate Professor Sebaratnam has received a payment or honoraria from Abbvie, Galderma, Novartis, Pfizer, Janssen-Cilag, LEO Pharma, Sun Pharmacentical Industries and Viatris; has received support for attending meetings and/or travel from Galderma; has been a Board Member for Novartis; has contributed to the Australasian College of Dermatologists’ General Practitioner Taskforce; and has received support from Syneron Candela Corporation Australia Pty Ltd and HEINE Optotechnik. Dr Lim is a member of the Australian Medical Council Cosmetic Surgery Technical Advisory Group; is Board Director of the Australasian College of Dermatologists; and holds stocks in EBOS Australia. Dr Lim’s partner is a paid advisor for the aesthetic device division of EBOS Australia.
References
1. Stewart N, Lim AC, Lowe PM, et al. Lasers and laser-like devices: part one. Australas J Dermatol 2013; 54: 173-183.
2. Geiges ML. History of lasers in dermatology. Curr Probl Dermatol 2011; 42: 1-6.
3. Alexiades-Armenakas MR, Dover JS, Arndt KA. The spectrum of laser skin resurfacing: nonablative, fractional, and ablative laser resurfacing. J Am Acad Dermatol 2008; 58: 719-737; quiz 738-740.
4. Saedi N, Petelin A, Zachary C. Fractionation: a new era in laser resurfacing. Clin Plast Surg 2011; 38: 449-461, vii.
5. Tajirian AL, Goldberg DJ. Fractional ablative laser skin resurfacing: a review. J Cosmet Lasr Ther 2011; 13: 262-264.
6. Katz B. Efficacy of a new fractional CO2 laser in the treatment of photodamage and acne scarring. Dermatol Ther 2010; 23: 403-406.
7. Sebaratnam DF, Lim AC, Lowe PM, et al. Lasers and laser-like devices: part two. Australas J Dermatol 2014; 55: 1-14.
8. Choi KJ, Williams EA, Pham CH, et al. Fractional CO(2) laser treatment for burn scar improvement: a systematic review and meta-analysis. Burns 2021; 47: 259-269.
9. Kearney C, Brew D. Single-session combination treatment with intense pulsed light and nonablative fractional photothermolysis: a split-face study. Dermatol Surg 2012; 38: 1002-1009.
10. Hantash BM, Stewart DB, Cooper ZA, et al. Facial resurfacing for nonmelanoma skin cancer prophylaxis. Arch Dermatol 2006; 142: 976-982.
11. Ostertag JU, Quaedvlieg PJ, van der Geer S, et al. A clinical comparison and long-term follow-up of topical 5-fluorouracil versus laser resurfacing in the treatment of widespread actinic keratoses. Lasers Surg Med 2006; 38: 731-739.
12. Zaleski-Larsen LA, Fabi SG. Laser-assisted drug delivery. Dermatol Surg 2016; 42: 919-931.
13. Ong MW, Bashir SJ. Fractional laser resurfacing for acne scars: a review. Br J Dermatol 2012; 166: 1160-1169.
14. Issler-Fisher AC, Waibel JS, Donelan MB. Laser modulation of hypertrophic scars: technique and practice. Clin Plast Surg 2017; 44: 757-766.
15. Laube S, Lanigan SW. Laser treatment of rosacea. J Cosmet Dermatol 2002; 1: 188-195.
16. Chee SN, Lowe P, Lim A. Laser skin resurfacing: a patient-centred classification based on downtime. Australas J Dermatol 2015; 56: 186-191.
17. Chee SN, Lowe P, Lim A. Smartphone patient monitoring post-laser resurfacing. Australas J Dermatol 2017; 58:e216-e222.