LARCs underused in Australian women prescribed teratogenic medications
By Dr Emily Lathlean MB BS, FRACGP
Concurrent use of highly effective hormonal contraception at the time of first dispensing of teratogenic medications (category X medications) is low in Australia, a retrospective cohort study has found, raising concerns about the risk of unintended pregnancy and potentially preventable fetal harm.
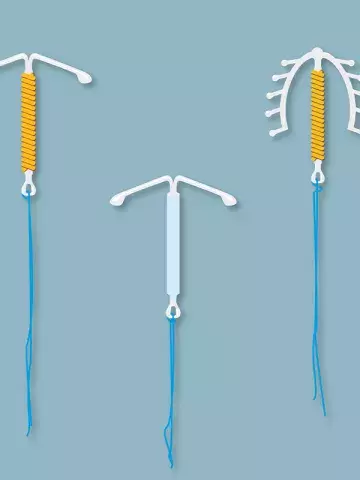
The study, published in the Medical Journal of Australia, analysed a 10% random sample of national PBS dispensing data, evaluating over 15,000 women aged 15 to 49 years. Researchers found that the prevalence of dispensing of category X medications almost doubled in Australia between 2013 and 2021 (increasing from 4.6 to 8.7 per 1000 women). The largest increase was for the dispensing of dermatological agents – in particular, isotretinoin, which was prescribed in 90% of cases. However, at the time of first dispensing of category X medications, only 22% of women had been dispensed any type of hormonal contraception and only 13% of women were using a long-acting reversible contraception (LARC).
‘... Almost one-half of pregnancies in Australia are unplanned, and an unintended pregnancy may only be recognised after the fetus has been exposed to a medication,’ wrote Dr Sarah Donald, a Public Health Physician from the University of Otago, New Zealand, in an accompanying editorial.
‘Consequently, guidelines recommend that highly effective contraceptive measures should be taken by all women of reproductive age during treatment with teratogenic medications and for an appropriate period after their discontinuation. LARC is considered very effective, with a failure rate below 1%.’ Women aged 15 to 19 years were less likely to be using LARC than older women.
‘One of the main limitations of the study is that ... the copper intrauterine device is not subsidised by the PBS, nor are several hormonal oral contraceptives that are frequently used in Australia,’ Dr Donald wrote. ‘...Despite the limitations of the dataset, contraception among women using teratogenic medications is probably unacceptably low.’
The researchers highlighted several barriers to LARC access that needed to be overcome, including poor access and awareness, misconceptions about its suitability (among both women and providers), costs and concerns about side effects.
‘...Our findings suggest that the uptake of highly effective contraceptive methods by Australian women prescribed category X medications could be improved,’ the researchers wrote.
‘Effective strategies for increasing LARC uptake in primary care include better training in contraceptive counselling and improving access to rapid referral clinics for insertion. These approaches could be adapted for use by other specialists, including dermatologists, accompanied by education of women prescribed category X medications.’
‘Ongoing surveillance of concurrent contraceptive use, as well as of unintended pregnancies and their outcomes, is also critical for refining risk management,’ the researchers wrote.
Med J Aust 2024; 221: 367-373 and 365-366; doi: 10.5694/mja2.52451 and doi: 10.5694/mja2.52445.