Beyond the wheeze – a fresh look at adolescent asthma

The management of adolescents and young people with asthma can be challenging and requires clinicians to consider life stage, development and psychosocial factors to ensure treatment is both appropriate and effective.
- Confirm the diagnosis of asthma with objective tests and monitor regularly to avoid over- or undertreatment.
- Review the young person alone for at least part of the consultation and provide reassurance regarding confidentiality.
- Develop, discuss and update an asthma action plan at every visit.
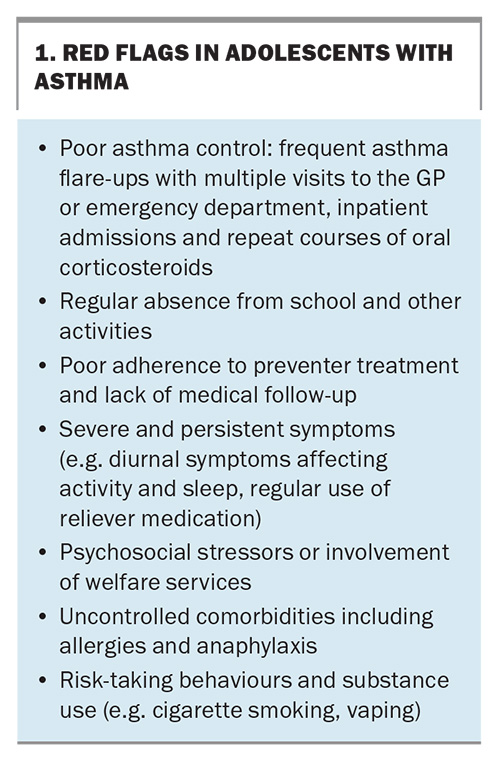
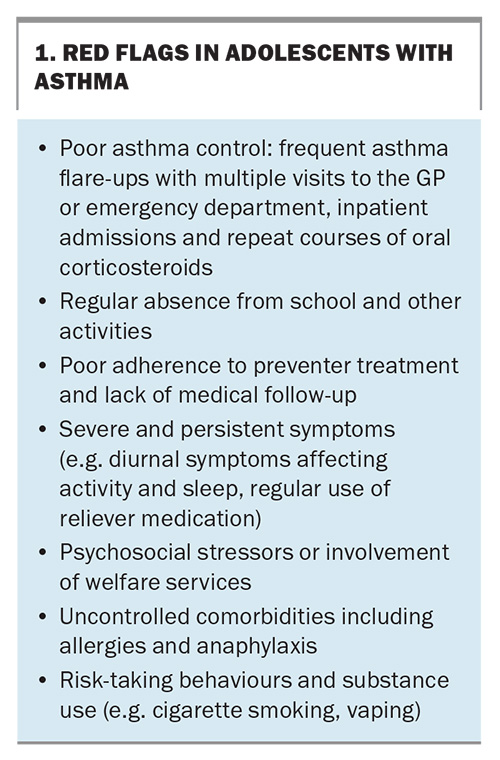
- Red flags for patients at high-risk of asthma include poor asthma control, nonadherence, under-recognition of symptoms, psychosocial stressors, risk-taking behaviours and communication barriers.
- Embrace digital health technologies in clinical practice, as they have been shown to improve adherence and symptom control.
Adolescents with asthma present a unique set of challenges for the discerning clinician associated with their developmental stage, physiological changes and the emergence of psychosocial factors that can impact management. Adolescents may modify their behaviours because of poor asthma control or under-recognise their symptoms, leading to poor adherence to treatment. Nonadherence to asthma medications is a well-known problem among the adolescent age group, further complicated by risk-taking behaviours, such as cigarette smoking, vaping and other substance use, which can lead to unexpected exacerbations and complications.
Parents are often surprised when their teenage child has an asthma episode, having been told they would outgrow their childhood asthma. Although some children with asthma do seem to recover, adolescents with childhood asthma should continue to be actively screened for symptoms of wheeze, chest tightness and shortness of breath. Data from the Australian Bureau of Statistics showed that in 2022, the prevalence of asthma in young people aged 15 to 24 years was about 8% in males and 12% in females aged 15 to 24 years, and 10% in boys and 6% in girls aged 14 years and younger.1 Puberty does not predict the remission of asthma and almost two-thirds of children with chronic asthma have persistent symptoms throughout puberty.2 Additionally, it is relatively common for asthma to first present during adolescence and this occurs more commonly in girls than boys.3
GPs play a key role in the assessment and management of adolescents and young people with asthma. Most primary care providers are well versed in the use of National Asthma Action Plans (AAPs) such as those available via the National Asthma Council Australia.4 Written and digital AAPs are some of the most effective clinical interventions we have and should be revisited at every consultation. Regularly updated AAPs have been shown to:
- improve adherence
- reduce school absenteeism
- reduce GP presentations
- reduce visits to the emergency department and hospital inpatient admissions.
- As GPs rightly continue to provide the bulk of care for adolescents with asthma, it is important to consider the following during clinic visits:
- identify adolescents who are vulnerable or at high risk (Box 1)
- address poor adherence and comorbid psychosocial issues
- promote ongoing self-management and emerging independence
- refer patients early for further assessment when the diagnosis is uncertain, there is treatment failure or red flags emerge (Box 1).
Diagnosis
Asthma is characterised by episodes of wheeze with shortness of breath, often precipitated by triggers such as viral infections or environmental factors. The Australian Asthma Handbook version 2.2, published in April 2022, is an online evidence-based clinical guideline for asthma management and contains a section specifically for asthma management in adolescents.5
As primary care providers, it is important to be clear about what constitutes asthma and what may otherwise be masquerading as variable airflow limitation. A detailed history and physical examination, use of objective measures of airway function and assessment of atopic status are needed to confirm a diagnosis of asthma. Investigations to consider that may require specialist referral include:
- spirometry including postbronchodilator response (withhold inhaled bronchodilators for a minimum of four hours before testing)
- fractional exhaled nitric oxide measurement, which is helpful in identifying the asthma phenotype (often associated with eosinophilic airway inflammation) and informing treatment decisions5,6
- allergen skin testing for common environmental and food allergens
- bronchial provocation (challenge) or exercise testing to establish evidence of airway hyper-responsiveness or reveal the cause of exercise-related symptoms; challenge tests are useful for excluding a diagnosis of asthma as the cause of current symptoms, are performed at accredited lung function laboratories and are indicated when asthma is suspected but initial spirometry does not demonstrate reversible airflow limitation7,8
- peak expiratory flow monitoring, which although not routinely recommended, can be helpful in some circumstances to establish evidence of airflow variability and motivate adherence to treatment.
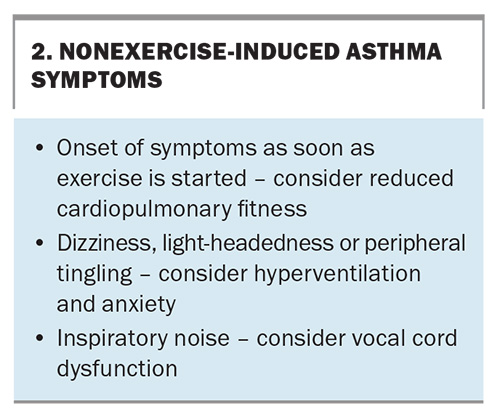
Exercise-related symptoms are common in the adolescent age group and may be caused by a variety of underlying factors not related to asthma. Adolescents may avoid exercise because of unrecognised asthma symptoms and therefore underappreciate the extent of their exercise limitations. Patients with exercise-related symptoms require accurate assessment to differentiate exercise-induced asthma from poor cardiopulmonary fitness, vocal cord dysfunction, hyperventilation, dysfunctional breathing and anxiety (Box 2).6,9
Recurrent cough as the predominant or only symptom can be misleading. Somatic cough disorder (previously known as psychogenic cough or habit cough) is often misdiagnosed as asthma and patients are treated inappropriately with inhaled corticosteroids (ICS).10 Anxiety and psychosocial factors may mimic or trigger acute asthma; however, these symptoms are associated with normal auscultation, lung function testing and oximetry findings. History is key in such cases and will often reveal a rapid improvement of symptoms once the psychosocial trigger has been addressed.
Assessment
Alongside the respiratory review, consider other issues that may be contributing to the clinical presentation. Often the cause of poor adherence, escalating symptoms or ‘treatment failure’ in adolescents may be caused by the following factors.
Allergies
Allergic rhinitis is an independent risk factor for developing asthma and frequently coexists with asthma.11 As many as 75% of patients with asthma also have allergic and nonallergic rhinitis, although estimates vary widely.12 The unified airway disease concept of a single inflammation affecting both the upper and lower airways has become increasingly recognised in the literature as contributing to comorbid allergic rhinosinusitis and asthma.13 Studies have shown that children and adolescents aged 5 to 18 years with comorbid allergic rhinitis had worse asthma control and therefore stand to benefit from simultaneous treatment of both interrelated conditions.14,15
Sleep
Chronic sleep deprivation and sleep disorders are common in adolescents, made worse by poor asthma control with night-time awakening and daytime sleepiness negatively impacting healthcare outcomes and academic achievement.16,17 Obstructive sleep apnoea and sleep disordered breathing are both independent risk factors for severe asthma, and treating these conditions will improve asthma control.16,18 Night-time symptoms with awakening suggest uncontrolled asthma and possibly hypoxia. Consider referral to a specialist and performing overnight oximetry or polysomnography if night-time symptoms persist despite treatment.
Obesity
Being overweight can affect lung mechanics with a reduced functional residual capacity, expiratory reserve volume and, to a lesser extent, total lung capacity. Obesity is also thought to be a risk factor for asthma because of the mechanisms of underlying inflammation and genetics, and is currently an area of active research.19,20 Social prescribing with goal setting for your adolescent patient with asthma to increase activity levels (join a gym, enrol in an extracurricular activity or sport) and eat healthily can be a feature of every consultation. Exercise-induced asthma need not be a barrier to exercise, and optimal use of reliever medications 10 to 20 minutes before physical activity can be part of adolescent patients’ AAPs and communicated to all caregivers.
Hormonal changes
Early puberty, often associated with obesity, is an independent risk factor for the persistence and severity of asthma into adolescence and thereafter. Although the mechanisms are unclear, hormonal fluctuation during puberty affect asthma control and preventer treatment may need to be adjusted accordingly.21 Exacerbations of asthma symptoms may worsen during the premenstrual phase in 40% of females and, if poorly controlled, hormonal management should be considered.22
Mental health
Anxiety, depression and other mood disorders often emerge during adolescence, and early recognition, assessment and support is important to achieve optimal asthma outcomes. Poor adherence to treatment may be an early indicator of family problems, psychological distress and stressful life events.23 Anxiety may either mimic asthma symptoms or trigger them, and exercises to help control breathing, meditation, mindfulness exercises, cognitive behavioural therapy and distraction strategies to reduce environmental stressors can help with self-management and improve outcomes for adolescents with asthma.24,25
Environment
Exposure to smoke and increased air pollution from bushfires can adversely affect lung health, leading to increased asthma exacerbations, hospital admissions and, in some cases, death. The 2019–20 ‘Black Summer’ bushfires caused multiple fatalities and significant respiratory morbidity, particularly across the eastern seaboard of Australia.26 In this context, population exposure to atmospheric particulate matter with a diameter less than 2.5 micrometres can cause widespread respiratory disease through oxidative stress and inflammation, and is a major public health concern.27
Thunderstorm asthma, seen not uncommonly during the spring and summer months in Australia, is triggered by massive loads of pollen allergen particles being released into the air. On days of high pollen count, fast-changing wind, temperatures and humidity can cause allergen particles to enter the bronchioles, causing airway inflammation. The Melbourne thunderstorm asthma event in November 2016 led to 10 deaths and a 672% increase above the three-year average of respiratory-related presentations to emergency departments across Victoria.28
Substance use
Ask adolescents routinely about their substance use, including cigarette smoking, vaping and use of other recreational drugs. Among those aged 12 to 17 years, cannabis remains the most used illicit substance.29 In the 2022–23 Australian Secondary Students’ Alcohol and Drug survey, a significantly higher proportion of students reported either vaping or smoking (16% vs 10%) or exclusively vaping (13% vs 2%), compared with proportions in 2017.29 Concerningly, there was an increase in susceptibility to smoking among Australian secondary school students who had never smoked, in both younger and older students, over these five years.29
Most alarming is the significant rise in vaping among Australian secondary school students. Since 2017, the proportion of ‘ever vaping’ has increased from 14% to 30% and ‘past month’ vaping from 4% to 16% overall in 2022–23. Most secondary school students in Australia reported using disposable vaping devices (80%), generally sourced from a friend (60%) or purchased from a vape shop (29%) or the Internet (20%), and almost two-thirds reported using e-cigarettes or e-liquids with nicotine content.29
Vaping appears to significantly increase the likelihood of subsequent smoking, potentially ushering in a new generation of tobacco users. Among students who had used an e-cigarette, 69% reported that they had never smoked a tobacco cigarette before their first experience with vaping. Furthermore, of these students who had never smoked before using an e-cigarette, 20% went on to smoke tobacco cigarettes, even if only a few puffs.
Regular smoking and vaping of marijuana confer considerable risk to pulmonary health, may trigger or exacerbate asthma symptoms and should be discussed with young people so they are aware of the risks.30,31
COVID-19 pandemic
Children and adolescents with asthma who have COVID-19 infection have less severe disease than adults and are less likely to present to the emergency department. However, those who had presented to the emergency department were significantly more likely to be admitted, required ventilatory support and had more severe forms of COVID-19 compared with children and adolescents without asthma.32
Effective management of adolescents with COVID-19 and asthma involves maintaining adherence to asthma medications and keeping asthma action plans up-to-date to accommodate any changes in symptoms or health status. It is also important to encourage COVID-19 and annual influenza vaccinations to reduce severe disease risks.
For those on ICS-containing treatments, reassure them of the importance of continued use, as discontinuation may lead to severe flare-ups triggered by viral infections. Preventive medications, which helped maintain respiratory health during the COVID-19 pandemic, remain important to mitigate the risk of severe asthma exacerbations.
An approach to management
Clear, evidence-based, stepwise treatment recommendations are easily accessible in the Australian Asthma Handbook.6 The Asthma and COPD Medications Chart, updated in September 2024, is also available to guide treatment selection (https://www.nationalasthma.org.au/living-with-asthma/resources/health-professionals/charts/ asthma-copd-medications-chart). When seeing an adolescent or young person with asthma, we recommend using the following approach and resources to maximise clinical effectiveness and engagement alongside the online resources outlined in Box 3.
Set the scene
- See the young person alone for at least part of the consultation and provide reassurance regarding privacy and confidentiality.
- Consider cultural perspectives and health beliefs that may potentially impact the patient and their family.
- Engage the family in the adolescent’s care and, for patients from non-English-speaking backgrounds, directly address parents and carers with the help of health interpreters.
Educate
- Explore and encourage the adolescent’s self-management capacity by helping them to set goals and expectations around therapy.
- Regularly assess their understanding and provide re-education about medications and side effects and address any concerns.
- Routinely check and reinforce correct inhaler technique to ensure effective medication delivery.
- Ask, in confidence, about smoking, vaping and other substance use, and educate the young person (and their family) about potential harms and how they exacerbate asthma symptoms.
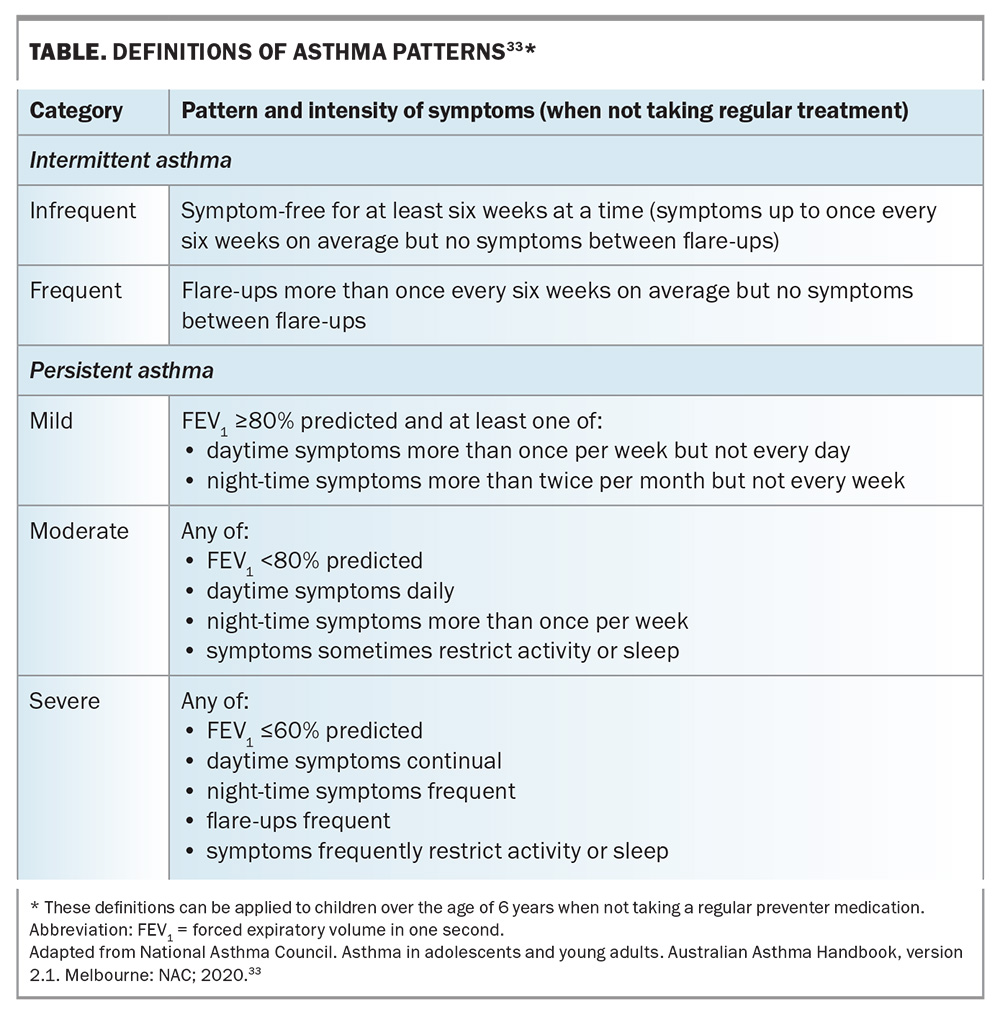
- It is also important to educate on the risks associated with severe asthma episodes. Highlight the dangers of the excessive use of short-acting beta agonists (SABAs) such as salbutamol, which can lead to tachyphylaxis, and emphasise the importance of seeking medical review if their asthma is worsening (Table)33 or if they find themselves using their rescue inhaler more frequently.
Adherence
- Ask open-ended questions to determine the degree to which the adolescent is participating with the agreed treatment plan. Find out what is working well and what is challenging for them to follow.
- Negotiate the treatment plan to engage the young person and provide an opportunity for shared decision-making.
- Promote regular routines and link taking medications to existing activities or set times of the day (e.g. before brushing teeth).
- Simplify treatment plans by choosing medications that need to be taken less frequently, for instance, a once-daily ICS such as ciclesonide or fluticasone furoate, or combination therapy such as fluticasone furoate and vilanterol trifenatate.
- Giving the patient a choice of preventer or reliever device, of which there is a dizzying number available, can help to empower and promote self-management (e.g. terbutaline sulfate turbuhaler is a useful reliever for patients unwilling to use a spacer, and easier to carry in a pocket or bag).
- Offer strategies to improve adherence and motivation including the use of digital apps, phone reminders and notifications (Box 3).
Identify risk factors
- Red flags for adolescents with asthma are outlined in Box 1. This cohort of patients will benefit from more regular GP review, engagement of the practice nurse and, if there are persisting issues, referral for specialist assessment.
- HEEADSSS 3.0 (home environment, education and employment, eating, peer-related activities, drugs, sexuality, suicide/depression, sleep and safety from injury and violence) is a helpful psychosocial screening instrument (available electronically; Box 3) to identify areas of concern for adolescents.34
- A home visit, particularly if the asthma is severe, is usually informative in identifying triggers (e.g. animal allergens, house dust mites, mould, smoke).
- Changing school, moving homes or family disruptions can disrupt treatment plans and mask symptoms, leading to poor control.
Treatment
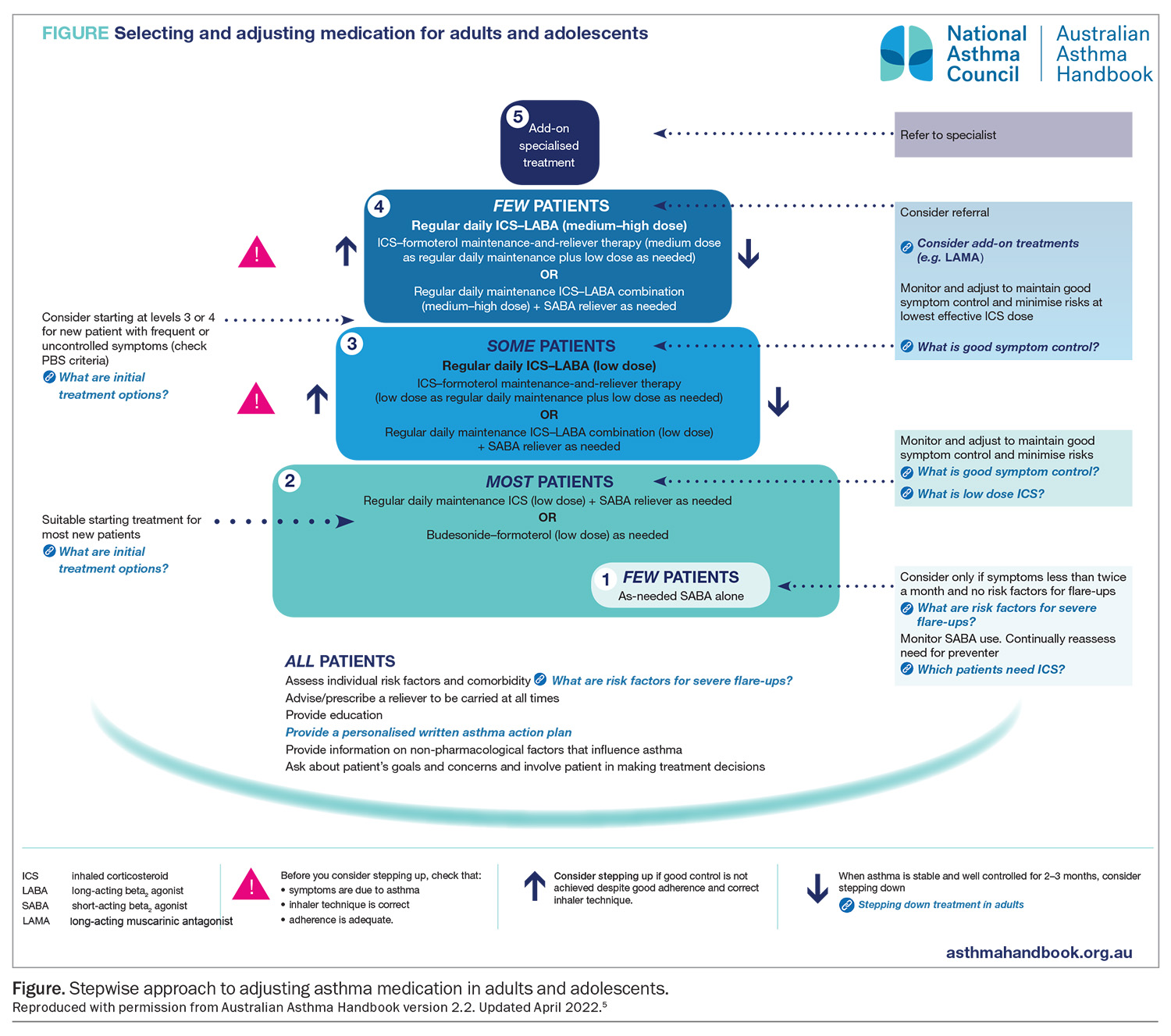
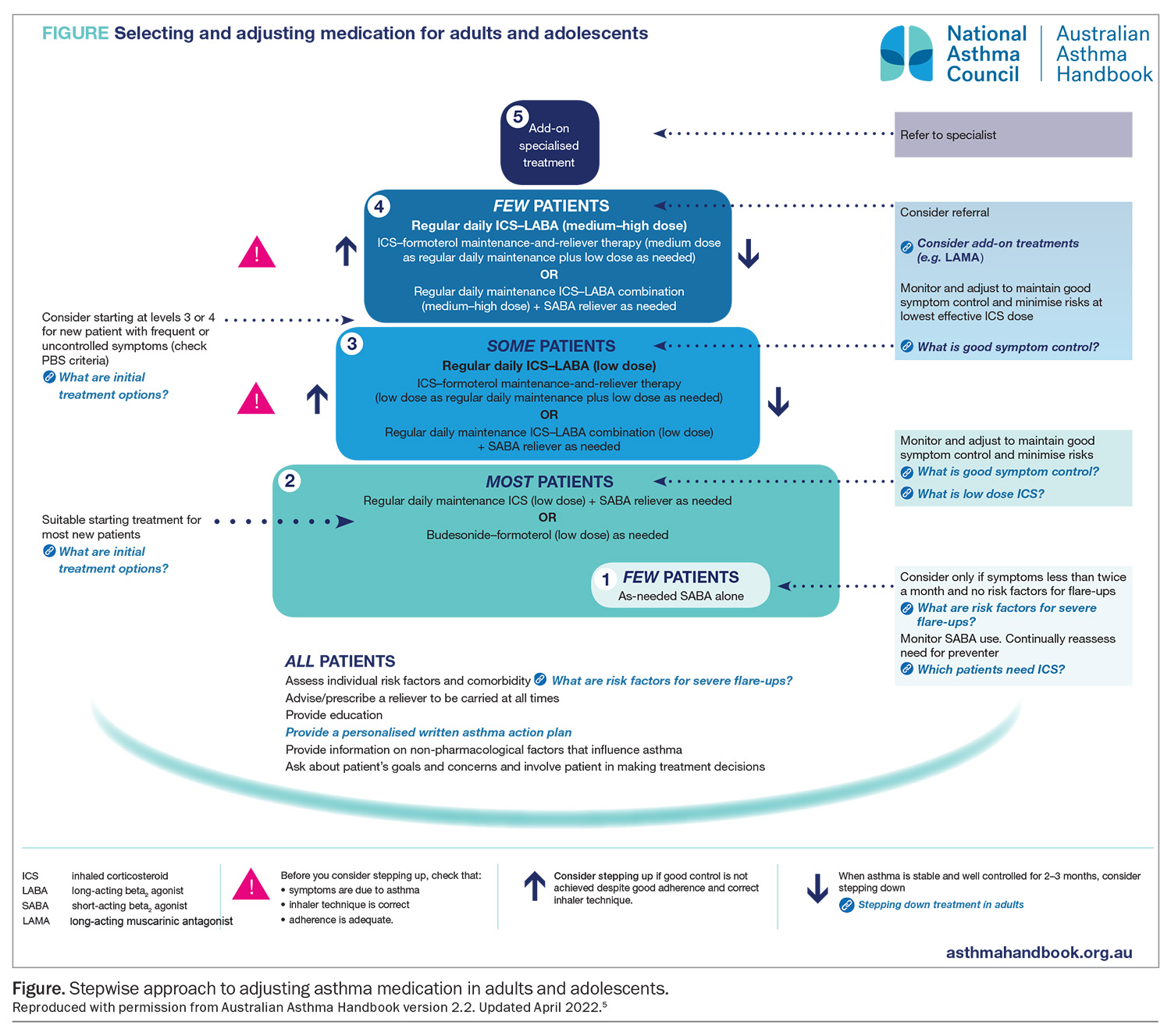
- Asthma is classified according to the frequency and persistence of symptoms. When selecting initial and subsequent preventer medications, consider the young person’s pattern of asthma, risk factors and comorbidities (Figure).5
- Before stepping up therapy, revisit the diagnosis, check symptoms are associated with asthma, inhaler technique is correct and adherence is adequate.
- By mid-adolescence (around 14 to 16 years), consider applying adult management guidelines in most situations.
- Monitor and adjust therapy to maintain good control at the lowest effective dose of preventer medications. When asthma is stable and well controlled for at least three months, consider stepping down the dose.
- Combination therapy medications (ICS plus long-acting beta2 agonists [ICS/LABA]) have been proposed as an option for some adolescents when starting treatment (Figure);5 however, data in this age group are limited.
- For most patients, consider low-dose budesonide/formoterol combination or regular daily maintenance ICS (low dose) and short-acting beta2 agonist (SABA) as reliever therapy for adolescents aged 12 years and older.
- For new patients with frequent or uncontrolled symptoms, consider starting at treatment levels 3 or 4 (Figure).5
- In 2019, the Global Initiative for Asthma (GINA) revised its guidelines, advising against SABA-only treatment for adults and adolescents because of its association with an increased risk of severe exacerbations. The GINA recommends that all adults, adolescents and most children with asthma should receive ICS-containing therapy to reduce the risk of severe exacerbations, either taken regularly, or (for adults and adolescents with ‘mild’ asthma) as combination ICS-formoterol, taken as needed for symptom relief. For patients with moderate-severe asthma, the preferred regimen is maintenance-and-reliever therapy (MART) with ICS-formoterol.35
- The pharmacological approach to treating allergic rhinitis usually consists of treatment with antihistamines, oral leukotriene antagonists (advise the family about potential adverse neuropsychiatric effects of montelukast in young people) and intranasal corticosteroids, the last being the most efficacious. Intranasal corticosteroids, often first-line treatment, are effective in reducing congestion, itching, rhinorrhoea, sneezing and ocular symptoms for adolescents with allergic rhinitis.12
- During bushfire season and periods of heavy air pollution, advise young people at high risk to stay indoors with windows and doors closed and to reduce strenuous physical exercise. Consider stepping up preventer therapy (e.g. increased corticosteroid dose) early if symptoms or exacerbations increase, particularly for those living in bushfire-prone areas. Update AAPs, reinforce adherence, and emphasise the importance of always carrying their reliever inhaler. For detailed guidelines on managing asthma during landscape fire events, refer to the Thoracic Society of Australia and New Zealand’s position statement, ‘Asthma and Landscape Fire Smoke’.36
Support
- Refer adolescents (and parents and carers) early for smoking cessation and provide opportunistic brief interventions at every episode.
- Offer concurrent psychological support for adolescents who express feelings of hopelessness, anxiety or depression.
- Recommend patients to peer-led programs in which adolescents are trained to teach their peers about asthma self-management. Peer-led programs have consistently been shown to improve health-related quality of life measures.37,38
- Family support and education is needed to help parents and carers look after their adolescent with a chronic condition. This is important not only to reinforce treatment routines but also to facilitate school, social and peer interactions.39
- Community asthma educators provide invaluable self-management support, education and training and can be accessed directly through Asthma Australia (Box 3).
Digital health technologies40
- Adolescents and young people are tech savvy and expect us to be too. A variety of digital health apps and resources are listed in Box 3.
- Multiple randomised controlled trials have demonstrated that web-based interventions (e.g. e-learning modules, AAP generators, medication lists, symptom diaries, online videos) are particularly effective in improving asthma scores and symptom-free days.
- Digital health apps have also been shown to improve both asthma control and adherence to treatment in adolescents.
- Text messaging and phone call reminders are effective in improving follow-up rates and appointment attendance.
Transition
Transition to adult care is an important consideration, especially for young people with complex asthma who are engaged with specialist paediatric services. GPs play an important role in transition planning, which incorporates re-education, self-management promotion and self-advocacy. Later in adolescence, it is helpful to establish an individual transition plan with early referrals made to appropriate adult services to ensure that the young person does not fall through the gaps.
Conclusion
All asthma deaths are preventable, and although the overall number has dropped considerably over the past several years in Australia, there has been little change in the rate of mortality due to asthma in the 5- to 34-year-old age group.41 Consequently, adolescence offers an important opportunity for intervention, with early referral to specialist multidisciplinary services indicated when the diagnosis of asthma remains uncertain, symptoms are inconsistent or uncontrolled, significant comorbidities exist and lung function testing does not demonstrate variable airflow limitation.
Our understanding and treatment options of ‘difficult’ or ‘therapy-resistant’ asthma have made considerable advances recently and a new era of immunotherapy and biologics (e.g. omalizumab, benralizumab, dupilumab and mepolizumab) offers hope for a subset of adolescents with complex asthma. However, for the most part, early recognition, regular monitoring and psychosocial support offer the greatest opportunity to give young people the best start in life.
Adolescence is a critical period in development, maturation and identity formation when opportunistic interventions and therapy planning may be especially beneficial. For adolescents with asthma, as with other chronic conditions, the role of the GP is crucial in maintaining good physical health, identifying risk factors that may contribute to poor control and recognising the developmental and psychosocial factors that affect their long-term outcomes. MT
COMPETING INTERESTS: None.
ACKNOWLEDGEMENT: Dr Louisa Owens, Head of Department of Respiratory Medicine, Sydney Children’s Hospital, Conjoint Lecturer, UNSW Sydney, Sydney, NSW, serves on the Professional Advisory Committee for Asthma Australia.
References
1. Australian Bureau of Statistics (ABS). Asthma [Internet]. Canberra: ABS; 2022. Available from: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/asthma/latest-release (accessed October 2024).
2. Nicolai T, Illi S, Tenbörg J, Kiess W, Mutius EV. Puberty and prognosis of asthma and bronchial hyper-reactivity. Pediatr Allergy Immunol 2001; 12: 142-148.
3. Towns SJ, van Asperen PP. Diagnosis and management of asthma in adolescents. Clin Respir J 2009; 3: 69-76.
4. National Asthma Council (NAC). Asthma action plan library. Australian asthma handbook, version 2.2. Melbourne: NAC; 2022. Available online at: https://www.nationalasthma.org.au/health-professionals/asthma-action-plans/asthma-action-plan-library (accessed October 2024).
5. National Asthma Council (NAC). Australian Asthma Handbook, version 2.2. Melbourne: NAC; 2022. Available online at: https://www.nationalasthma.org.au/health-professionals/australian-asthma-handbook (accessed October 2024).
6. Fielding S, Pijneneburg M, de Jongste JC, et al. Change in FEV1 and Feno measurements as predictors of future asthma outcomes in children. Chest 2019; 155: 331-341.
7. Anderson SD. Indirect challenge tests: airway hyperresponsivenes in asthma: its measurement and clinical significance. Chest 2010; 138(2 Suppl): 25S-30S.
8. Anderson SD. Bronchial challenge tests: usefulness, availability and challenges. Breathe 2011; 8: 53-60.
9. Boulding R, Stacey R, Niven R, Fowler SJ. Dysfunctional breathing: a review of the literature and proposal for classification. Eur Respir Rev 2016; 25: 287-294.
10. Morice AH, Milqvist E, Bieksiene K, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J 2020; 55: 1901136.
11. Rochat MK, Illi S, Ege MJ, et al; Multicentre Allergy Study (MAS) group. Allergic rhinitis as a predictor for wheezing onset in school-aged children. J Allergy Clin Immunol 2010; 126: 1170-5.
12. Brozek JL, Bosquet J, Baena-Cagnani CE, et al; Global Allergy and Asthma European Network; Grading of Recommendations Assessment, Development and Evaluation Working Group. Allergic rhinitis and its impact on asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol 2010; 126: 466-476.
13. Rimmer J, Ruhno JW. Rhinitis and asthma: united airway disease. Med J Aust 2006; 185: 565-571.
14. de Groot EP, Nijkamp A, Duiverman EJ, Brand PLP. Allergic rhinitis is associated with poor asthma control in children with asthma. Thorax 2012; 67: 582-587.
15. Szefler S, Phillips BR, Martinez FD, et al. Characterization of within-subject responses to fluticasone and montelukast in childhood asthma. J Allergy Clin Immunol 2005; 115: 233-242.
16. Wenzel SE, Brillhart S, Nowack K. An invisible disease: severe asthma is more than just ‘bad asthma’. Eur Respir J 2017; 50: 1701109.
17. Kansagra S. Sleep disorders in adolescents. Pediatrics 2020; 145 (Suppl 2): S204-S209.
18. Gibson PG, Reddel, McDonald VM, et al. Effectiveness and response predictors of omalizumab in a severe allergic asthma population with a high prevalence of comorbidities: the Australian Xolair Registry. Internal Med J 2016; 46: 1054-1062.
19. Canöz M, Erdenen F, Uzun H, Müderrisoglu C, Aydin S. The relationship of inflammatory cytokines with asthma and obesity. Clin Invest Med 2008; 31: E373-E379.
20. Melén E, Granell R, Kogevinas M, et al. Genome-wide association study of body mass index in 23,000 individuals with and without asthma. Clin Exp Allergy 2013; 43: 463-474.
21. Patton GC, Viner R. Pubertal transitions in health. Lancet 2007; 369: 1130-1139.
22. Rao CK, Moore CG, Bleecker E, et al. Characteristics of perimenstrual asthma and its relation to asthma severity and control: data from the Severe Asthma Research Program. Chest 2013; 143: 984-992.
23. Bender BG. Risk taking, depression, adherence, and symptom control in adolescents and young adults with asthma. Am J Respir Crit Care Med 2006; 173: 953-957.
24. Lavoie KL, Boudreau M, Plourde A, et al. Association between generalized anxiety disorder and asthma morbidity. Psychosom Med 2011; 73: 504-513.
25. Theoharides TC, Enakuaa S, Sismanopoulos N, et al. Contribution of stress to asthma worsening through mast cell activation. Ann Allergy Asthma Immunol 2012; 109: 14-19.
26. Vardoulakis S, Jalaludin BB, Morgan GG, et al. Bushfire smoke: urgent need for a national health protection strategy. Med J Aust 2020; 212: 349-353.
27. Lodovici M, Bigagli E. Oxidative stress and air pollution exposure. J Toxicol 2011; 487074.
28. Thien F, Beggs BJ, Csutoros D, et al. The Melbourne epidemic thunderstorm asthma event 2016: an investigation of environmental triggers, effect on health services, and patient risk factors. Lancet Planet Health 2018; 2: e255-e263.
29. Australian Government Department of Health and Aged Care. Australian secondary school students alcohol and drug) survey. Canberra: Australian Government; 2024. Avaliable online at: https://www.health.gov.au/resources/collections/australian-secondary-school-students-alcohol-and-drug-survey (accessed October 2024).
30. Australian Institute of Health and Welfare (AIHW). Alcohol, tobacco and other drugs in Australia. Canberra: AIHW; 2020. Available online at: https://www.aihw.gov.au/reports/alcohol/alcohol-tobacco-other-drugs-australia (accessed October 2024).
31. Thanavala Y, Goniewicz ML. Vaping-induced severe respiratory disease outbreak: what went wrong? Lancet Respir Med 2019; 7: 1014-1015.
32. Robbins E, Daoud S, Demissie S, James P. The impact of asthma on COVID-19 disease severity in children and adolescents. J Asthma 2023; 60: 1097-1103.
33. National Asthma Council (NAC). Asthma in adolescents and young adults. Australian Asthma Handbook, version 2.1. Melbourne: NAC; 2020. Available online at: https://www.asthmahandbook.org.au/management/adolescents (accessed October 2024).
34. Klein DA, Goldenring JM, Adelman WP. HEEADSSS 3.0: the psychosocial interview for adolescents updated for a new century fueled by media. Contemporary Paediatrics 2014, Jan 1. Available online at: https://www.contemporarypediatrics.com/view/heeadsss-30-psychosocial-interview-adolescents-updated-new-century-fueled-media (accessed October 2024).
35. Levy ML, Bacharier LB, Bateman E, et al. Key recommendations for primary care from the 2022 Global Initiative for Asthma (GINA) update. NPJ Prim Care Respir Med 2023; 33: 7.
36. McDonald VM, Bardin PG, Upham JW, et al. Asthma and landscape fire smoke: a Thoracic Society of Australia and New Zealand position. Respirology 2023; 28: 1023-1035.
37. McCallum GB, Chang AB, Wilson CA, et al. Feasibility of a peer-led asthma and smoking prevention project in Australian schools with high Indigenous youth. Front Pediatr 2017; 5: 33.
38. Rhee H, Belyea MJ, Hunt JF, Brasch J. Effects of a peer-led asthma self-management program for adolescents. Arch Pediatr Adolesc Med 2011; 165: 513-519.
39. Szyndler JE, Towns SJ, van Asperen PP, McKay KO. Psychological and family functioning and quality of life in adolescents with cystic fibrosis. J Cystic Fibros 2005; 4: 135-144.
40. Unni E, Gabriel S, Ariely R. A review of the use and effectiveness of digital health technologies in patients with asthma. Ann Allergy Asthma Immunol 2018; 121: 680-691.
41. Australian Institute of Health and Welfare (AIHW). Chronic respiratory conditions: Asthma. Canberra: AIHW; 2024. Available online at: https://www.aihw.gov.au/reports/chronic-respiratory-conditions/asthma (accessed October 2024).