Youth, obesity and worn knees. A trifecta of trouble
An morbidly obese 38-year-old woman with advanced osteoarthritis has disabling knee pain. Is immediate knee replacement surgery appropriate for this patient?
Case scenario
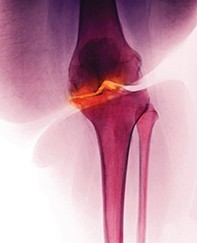
Millie is a very overweight 38-year-old woman with a BMI of 42 kg/m2. She has advanced osteoarthritis with relentless pain, particularly in her right knee, imaging of which has shown complete breakdown of cartilage as well as bone oedema and cysts. She has three young children and is finding it difficult physically to cope with all the necessary activities of daily living. She has been told that a knee replacement cannot be contemplated until she reaches the age of 50 years.
Is this age for knee replacement a widely accepted orthopaedic guideline, or might she have been told this as part of a vigorous attempt to get her to lose weight? What can be done for Millie?
Commentary
This case scenario describes an increasing problem throughout the Western World for which we are grappling to find a solution. The WHO describes obesity as a global epidemic about to surpass malnutrition and infectious disease.1 The past decade has seen an increase in obesity of 50% and evidence of its association with cardiovascular, endocrine, malignancy and musculoskeletal problems, but sadly many obese people are not aware of the dramatic reduction of both the quality and quantity of their life.
The US Centers for Disease Control and Prevention estimates that two-thirds of obese people will have knee osteoarthritis, compared with 45% of the normal population.2 British epidemiology studies suggest a sixfold increase in knee osteoarthritis and an 18-fold increase in bilateral arthritis in people who are obese.3 People who are morbidly obese fair far worse. The patient in the case scenario, Millie, considers herself as overweight but her BMI of 42 kg/m2 classifies her as morbidly obese; if she was 165 cm tall, she would weigh 115 kg, which is considerably more than her optimal weight of 62 kg (BMI, 22 kg/m2).
National joint registries have shown a sustained increase in the portion of total knee replacements being performed in younger patients.4,5 Over the past decade there has been a doubling in the number of men and almost tripling in the number of women in the 45 to 54-years age group having total knee replacements.5 Overall the demand for joint replacement surgery is escalating at an ever-increasing rate.
How to evaluate the patient
The standard approach of history, examination and further tests is applicable to all orthopaedic conditions. Morbidly obese patients usually have a range of comorbidities that often have far more pressing issues than the presenting complaint that is the focus of the patient’s attention. The literature can only be described as depressing on every psychological, physiological and musculoskeletal parameter. When assessing these patients, it is most important to obtain a good rapport in a nonjudgemental and supportive fashion, particularly as the goal is to direct the patient to improved lifestyle choices.
Knee pain is present in about 50% of obese people, compared to in 12% of underweight people.6 It is anticipated that obese patients will have patellofemoral pain associated with the use of stairs and chairs; this relatively benign chronic weight-related pain can be managed by weight loss or decreasing patellofemoral activities. Medial and lateral compartment pain is associated with weight-bearing activities and is usually progressive.
Important historical elements are the magnitude of the existing disability and handicap of this chronic affliction that will inevitably worsen. The occurrence of minor trauma and acute exacerbating events causing knee pain are of less concern when a diagnosis of advanced osteoarthritis is made because the presenting event is only the beginning of a longer-term treatment program.
Investigations
Imaging of obese patients with osteoarthritic symptoms should be limited to plain radiographs. A standing x-ray is the optimum imaging to delineate the magnitude of osteoarthritis, which is associated with a decrease in joint space on weight-bearing films. The role of MRI is negligible in the context of osteoarthritis and this imaging has no use in patients with morbid obesity. Millie’s MRI describes the hallmarks of osteoarthritis; these MRI findings are anticipated from the history and add little to the prognosis or management options.
A full blood count, biochemical profile and liver function tests are warranted investigations in an obese patient with osteoarthritis to provide a baseline. Malnutrition and endocrine abnormalities are the norm for morbidly obese patients.
Approach to management
Morbid obesity and osteoarthritis are both chronic conditions that inevitably erode the patient’s quality of life. It is highly desirable to have the patient work with a health practitioner in a co-operative fashion but many patients fail to appreciate the magnitude of their problems and are often reluctant to confront them. Many obese patients live within a sustained belief of denial and the rapid development of pain and loss of function may be the first time they are confronted with the implications of their being overweight. It is important to establish rapport as many patients will find discussions of their obesity embarrassing, and many have underlying psychological triggers that have initiated the event leading to their pathological weight gain.
The most efficacious treatment for the resolution of knee pain is substantial and sustained weight loss, a treatment that patients find hard to accept at initial consultations. The Framingham study concluded that a decrease in BMI of two points (equivalent to a 5-kg weight loss) led to a 50% reduction in the development of knee arthritis in women at 10 years.7 A useful ploy is to work with the patient in the context of preparing them for future surgical encounters for which the risks are excessive at this time.
Successful and sustained weight loss programs usually involve a multidisciplinary approach. Bariatric surgery has been shown to be a clinically effective and cost-effective intervention for patients with morbid obesity compared with nonsurgical intervention. Conversely, it is a sad disappointment that the common belief that patients will lose weight following knee replacement surgery is untrue, so it can be assumed that knee surgery has no benefit on weight-related medical conditions.
Medical treatment of osteoarthritis is a well-trodden path and the most effective interventions have been well studied. The effect size of placebo is 0.2, thus many patients have successfully encountered nontherapeutic drug and herbal treatments; most of these are futile but harmless. The routine medications of paracetamol and anti-inflammatories each have an effect size of 0.5 and are well recommended with consideration of an individual’s risk–benefit ratio. Opioids are inappropriate in young patients. Unloading painful joints with walking aids is usually successful, and the use of a single stick may unload the limb by 40% although the suggestion of this treatment is often poorly received.
Surgery for osteoarthritis
Morbidly obese patients with knee pain and osteoarthritis may be candidates for knee surgery. There is no role for joint salvaging procedures such as arthroscopic interventions or osteotomies. From a mechanical perspective, each kilogram of excessive weight loads the knee by four times. Thus our morbidly obese patient Millie, who weighs about 50 kg more than her ideal body weight, will load her knee with an additional 200 kg and not surprisingly will have pain and decreased function.
In comparative studies, there is limited information on knee replacement surgery in patients who are morbidly obese. Obese patients tend to have a similar magnitude of knee improvement following surgery as nonobese patients but they start, and end, at a much lower level of function (including walking distance, the use of walking aids, psychological scores and use of global pain relief).
For nonobese young patients with osteoarthritis and knee pain, the goals are to optimise their conservative management, essentially to bide time and reduce their time-dependant risk of wear-related revision knee surgery. However, they have a dramatic erosion of their quality of life that must be risk-weighted against their likelihood of outliving a joint replacement. For disabled young patients, the timing of their first joint replacement is a strategic plan many decades in length, often anticipating further revision surgeries in mid and later life. There are no strict age-related limits for joint replacement surgery. Younger patients predictably wear their joint replacements at a substantially faster rate and have a greater life expectancy, and will therefore require more revision surgery. In Australia, patients aged 65 to 77 years have a knee replacement failure rate of 4.2% at 10 years after the surgery compared with 11.4% at 10 years for those aged under age 55 years.4
Obese patients considering knee replacement surgery are strongly advised to optimise their risk profile, especially to minimise the risk of infection and perioperative mortality. Morbidly obese patients have a greater prevalence of deep prosthetic infection (three to nine times) compared with controls. Successful treatment of an infected joint replacement is profoundly more complex and dramatically less successful in obese patients. Also, the primary surgery is more complex in obese patients, who are at risk of wound healing problems, ligament damage, reduced range of motion and perioperative medical complications.
The risk–benefit profiles of morbidly obese patients are very different from those of nonobese patients. Their surgical risks are dramatically increased in the perioperative period but their limited demands and dramatically shortened life expectancies probably mitigate their long-term revision risks compared with similarly aged non-obese patients. As the lifespan of an obese patient is decreased by eight to 10 years, Millie’s projected life expectancy at her present age of 38 years is reduced to a further about 38 years, which is similar to that of a 50-year-old Australian woman (from life tables; http://aga.gov.au/publications/life_table_2010-12/). Although Millie would overload her replaced knee should she have the surgery, her decreased activity profile would minimise the number of cycles (steps) per year. Embarking upon the challenges of knee surgery is consequently more akin to the challenges faced by a less active and older patient with multiple comorbidities.
When to refer to an orthopaedic surgeon
The management of patients with osteoarthritis and knee pain will usually involve a multidisciplinary team of which the orthopaedic surgeon is likely to be the last to intervene, when a knee replacement is required. Wherever possible, patients should be educated and optimised before considering a referral for orthopaedic surgery. Most episodes of acute knee pain will settle with time and the use of walking aids and analgesics, and rarely need surgical review.
Referral for knee replacement surgery should be considered when patients have stabilised their weight after a weight-reduction program, optimised their medical health and have a reasonable risk profile for surgery. Morbidly obese patients have a higher prevalence of complications in all studies. The risk profile of a morbidly obese patient is dominated by their weight-related comorbidities and less influenced by age, and is more similar to that of a much older medically infirm patient than to a nonobese patient of their own age.
Once it has been decide that surgery should be performed, patients should be optimised in preparation for it. Paradoxically weight loss is associated with malnutrition and muscle atrophy, and maintenance of muscle tone with nonweight-bearing exercises such as swimming and nonimpact gym work is an important adjunct to weight loss interventions.
Conclusions
Osteoarthritis and knee pain are anticipated associations with morbid obesity. Disabling knee pain in a morbidly obese patient may be the focus of the patient’s attention but is merely the tip of the iceberg of a host of medical and psychological problems. Knee replacement surgery may be the conclusion of the therapeutic spectrum but has considerable risk and it would be remiss not to optimise the patient’s global comorbidities. A multidisciplinary program aimed at normalising body mass and maintaining muscle tone is likely to reduce knee pain and improve lifespan. Symptomatic knee osteoarthritis will inevitable progress and surgery is likely to be required and repeated several times over the patient’s lifespan. MT