Osteoarthritis: best-evidence care

Evidence-based, first-line osteoarthritis management should be person-centred, support self-management and take an interdisciplinary or multidisciplinary approach that revolves around lifestyle and behavioural interventions with optional use of adjunctive therapies. In settings where there are no interdisciplinary or multidisciplinary teams, evidence-based and reliable online resources and support may be helpful.
- Osteoarthritis is a common condition in Australia that can be debilitating.
- Core components of best-evidence, first-line osteoarthritis management are education and support for self-management, increasing physical activity and weight management (if appropriate).
- First-line management strategies can be supplemented with adjunctive therapies, including analgesic medication, bracing and orthoses, and walking aids. However, the evidence on the effectiveness of these therapies is conflicting.
- Joint replacement surgery for osteoarthritis is a last-resort option and is only indicated if the condition is significantly impacting a person’s quality of life and other nonsurgical management strategies have either failed or are not appropriate.
- Care for people with osteoarthritis needs to be person-centred, support self-management and ideally use an interdisciplinary or multidisciplinary approach.
- In settings where there are no interdisciplinary or multidisciplinary teams to collaborate and help deliver best-evidence osteoarthritis care, clinicians can opt to use online resources and support when available.
Osteoarthritis is a serious condition, affecting the structures of synovial joints, including the cartilage, subchondral bone, ligaments, muscles and synovial fluid. It is a disease of the whole joint, and affects more than 3 million people in Australia.1,2 Symptomatic osteoarthritis is a debilitating condition that is often associated with significant pain and impaired function, thereby negatively impacting quality of life.3
In Australia, osteoarthritis contributed to 2.5% of the total disease burden and 20% of musculoskeletal disease burden in 2023 (disability-adjusted life years).4 Even more concerning is that people with osteoarthritis have twice the risk of all-cause mortality compared with their peers without the condition.5 Although the reason for this is unclear, it may be attributed to associated comorbidities. People with osteoarthritis shoulder a high comorbidity burden, with the most prevalent conditions associated with osteoarthritis being hypertension, and circulatory and metabolic diseases.6
It is well known that osteoarthritis is a very costly condition. Healthcare for osteoarthritis in Australia was estimated to cost around $4 billion in 2020–21, with most of this cost being attributed to surgical procedures.4 Most (86%) of the costs were associated with hospital services, with only 9% spent on primary care and 5% on other referred services, such as imaging. Knee arthroplasty is the most common surgical procedure, with 64,846 procedures performed in 2022 (compared with 52,863 hip and 8,636 shoulder arthroplasties). Although it is considered to be an effective procedure in people with severe end-stage osteoarthritis, around 20% of knee arthroplasty recipients are dissatisfied with the results following the procedure, suggesting that patient selection for the procedure should be improved.7 People with osteoarthritis commonly present for joint arthroplasty without having tried the recommended first-line lifestyle and behavioural interventions, namely education for self-management, therapeutic exercise, physical activity and weight management. In Australia, analyses from 2019 showed that $875 million would have been saved if 68% of people with knee osteoarthritis avoided surgery, and adopted first-line lifestyle and behavioural interventions.8 Delivery rates of these first-line strategies remain substantially lower than rates of surgical referrals and pharmacological treatments.9 This could be attributed to the need for more support for primary care clinicians, such as GPs and physiotherapists, in delivering and implementing these strategies in management plans for people with osteoarthritis.10 This article highlights the current evidence around evidence-based osteoarthritis management and discusses recommendations to facilitate this care in clinical practice.
What is evidence-based, first-line osteoarthritis management?
International osteoarthritis clinical guidelines consistently recommend that at the core of best-evidence, first-line osteoarthritis management are lifestyle and behavioural interventions, including education and support for self-management, increasing incidental physical activity and participation in structured exercise, and weight management, if appropriate.11,12
Education and supporting self-management
Providing education about what osteoarthritis is and guidance on how to self-manage it is an essential component of providing high-value osteoarthritis care.13,14 Education is at the crux of self-management programs, which are designed to encourage people with osteoarthritis to modify their behaviour by engaging in lifestyle interventions (e.g. increasing physical activity levels) and to be actively managing their own condition. Ultimately, the goal is to empower people with osteoarthritis and promote self-efficacy by helping them develop skills such as problem solving, shared decision-making with their health professionals, and knowing how and where to identify helpful resources.15
What can I recommend?
Health professionals can support people with osteoarthritis in self-managing their condition by employing a range of strategies, such as:
- sharing information with patients about the diagnosis and available treatment, and expectations from diagnosis and treatment, as well as patient-facing education to help people understand their condition(s) to improve their health
- consulting and collaborating with patients through shared decision-making, goal-setting and following up, and allowing them to set the agenda by asking their perspective for the consultation
- partnering with the patient and developing strategies for self-management together.15
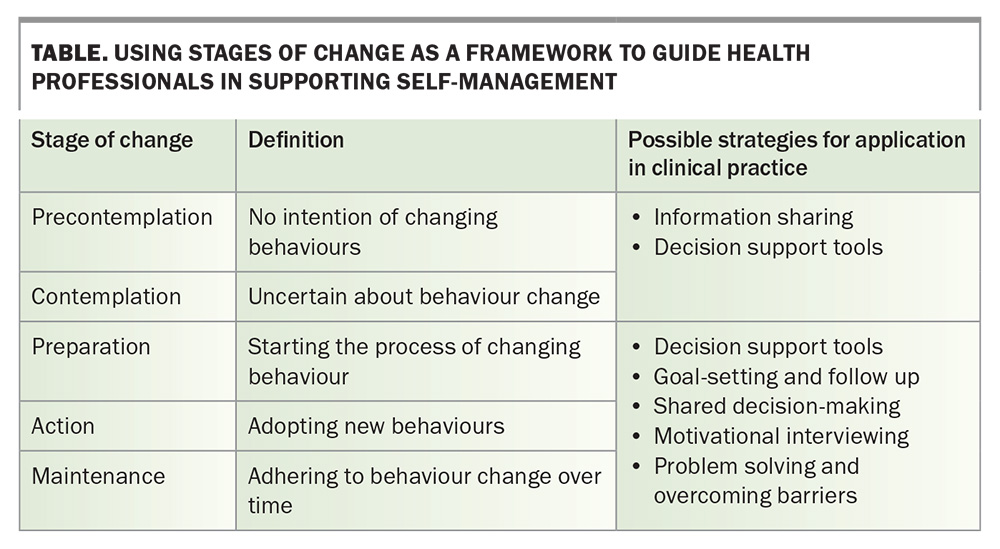
It is important to note that information sharing alone is unlikely to improve outcomes and motivate behaviour change, and active behaviour change interventions are unlikely to be effective if the person is not willing and motivated to self-manage their condition.15 The Stages of Change framework may be helpful for health professionals to identify the appropriate strategies that can help with this (Table).15,16
Physical activity and exercise
Increasing physical activity or engaging with exercise is strongly recommended for people with osteoarthritis.12 A recent network meta-analysis showed that exercise was more effective than usual care for pain relief and functional improvement in people with hip or knee osteoarthritis, and reached minimal clinically important differences.17 This meta-analysis also demonstrated that exercise was just as effective for pain relief and functional improvement compared with oral NSAIDs and paracetamol.17
What can I recommend?
Although it is widely accepted that increasing physical activity and exercise is beneficial for people with osteoarthritis, it is often difficult to know what exactly to recommend to patients. Another network meta-analysis demonstrated that aerobic and mind-body exercises (such as yoga and tai-chi) were the most effective in improving pain and function in people with knee and hip osteoarthritis compared with usual care.18 Strength and flexibility exercises had lower effect sizes but were still effective compared with usual care.18 Therefore, the evidence has shown that any form of exercise is beneficial for people with osteoarthritis. There are many recommendations that you could make for a person with osteoarthritis, but the focus should be on helping people to identify physical activity and exercise forms that they enjoy, are likely to engage with for the long term and are happy to progress. Another option is to refer people with osteoarthritis to allied health professionals who are experienced in prescribing and developing physical activity and exercise plans, such as physiotherapists and exercise physiologists.
Weight management
Clinical guidelines strongly recommend weight management as a core strategy for people with osteoarthritis.12 Evidence shows that a 5 to 10% reduction in weight significantly improves osteoarthritis symptoms in people who are overweight or obese and that there is a dose-response relationship.19,20 Most of the literature focuses on the effect of consuming anti-inflammatory diets (such as the Mediterranean diet) and low calorie diets on osteoarthritis symptoms, with varying results and high heterogeneity across studies.21 A meta-analysis demonstrated that very low calorie diets (less than 800 kilocalories per day) were the most effective dietary intervention for weight loss and improved physical function in people with osteoarthritis who were overweight or obese.22 Furthermore, a recent randomised controlled trial in Melbourne showed that a very low calorie diet was effective in achieving clinically relevant weight loss and was considered safe for people with knee osteoarthritis who were overweight or obese.23 However, it is important to be cautious with recommending this strategy as it has little long-term benefits, and is not nutritionally sufficient.24
What can I recommend?
Very low calorie diets, such as meal replacements, may be an appropriate strategy to recommend to a person with osteoarthritis who is overweight or obese to achieve significant short-term weight loss and improve function. However, adhering to a very low calorie diet can be challenging. Instead, long-term weight loss can be achieved by:
- an initial significant weight loss
- reaching the self-determined goal weight
- adopting a physically active lifestyle
- having a regular meal rhythm
- healthy eating
- controlling overeating habits
- self-monitoring lifestyle behaviours.25
As per the strategies above, it is important to focus on the willingness and motivation of the patient to adopt new behavioural strategies. Referral to dietitians or nutritionists may benefit a person with osteoarthritis who may require further food education and strategies for behaviour change.
Other treatments and management strategies
First-line management strategies can be supplemented with adjunctive therapies, including analgesic medication, bracing and orthoses, and walking aids.26 However, the evidence on the effectiveness of these therapies is conflicting, and they should only be used when their benefit may help facilitate an individual’s adherence to first-line interventions or to enhance the effects of these treatments.27,28 Analgesic medication, specifically NSAIDs, can be used to manage increased pain or flare-ups but are not recommended for long-term use.29 The current Royal Australian College of General Practitioners (RACGP) guidelines recommend the use of oral NSAIDs ‘at the lowest effective dose for a short period’ and to inform patients of possible adverse events, such as gastrointestinal, renal and cardiovascular effects.11
There is limited evidence for the efficacy of other adjunctive therapies, such as supplements or nutraceuticals and intra-articular injections. There are currently no supplements or nutraceuticals that are recommended by any guidelines for osteoarthritis management.27 In fact, glucosamine, chondroitin, fish oil (or omega 3) and vitamin D are strongly recommended against for managing osteoarthritis symptoms because of the lack of evidence in high-quality clinical trials and publication bias (industry-sponsored trials).27,30 As for intra-articular injections, most clinical guidelines recommend against their use, except for corticosteroid injections, which are recommended for managing knee osteoarthritis.27 The RACGP Guideline for the Management of Hip and Knee Osteoarthritis recommends the use of corticosteroid injections for short-term pain relief; however, these recommendations were based on very low-quality evidence and the guideline also warned of their potential harms if used repeatedly.11
Although joint replacement surgery is a cost-effective intervention, particularly for people with end-stage knee or hip osteoarthritis, not everyone with osteoarthritis will need joint replacement.31,32 Between 20 and 40% of people who undergo joint replacement surgery do not need it and up to 25% will not be satisfied with their outcomes.33,34 Joint replacement surgery for osteoarthritis should only be indicated if the condition is significantly impacting a person’s quality of life and other nonsurgical management strategies have either failed or are not appropriate.35 Surgical intervention should be the last resort.
Facilitating best-evidence, first-line osteoarthritis management
To facilitate best-evidence care for people with osteoarthritis, it is important that the right health professionals are delivering the right care at the right time and in the right place. Care for people with osteoarthritis needs to be person-centred, support self-management and use an interdisciplinary or multidisciplinary approach.36
In the NSW public health system, the Osteoarthritis Chronic Care Program (OACCP) serves to provide care for people with osteoarthritis that is tailored and person-centred, and uses a team of health professionals to deliver optimal care.37,38 Depending on the location, the team may include physiotherapists, rheumatologists, dietitians, psychologists, social workers, occupational therapists, orthotists and orthopaedic surgeons. The OACCP has improved access to best-evidence, first-line osteoarthritis care for people in NSW public hospitals. In some people, the OACCP has improved osteoarthritis symptoms sufficiently to enable them to delay joint arthroplasty or avoid it altogether.39 Unfortunately, osteoarthritis management programs, such as the OACCP, are not widely available across Australia. In primary care settings, multidisciplinary care is probably more appropriate, where best-evidence care is also delivered through collaborations between health professionals, drawing on the strengths of different disciplines.40 Building and maintaining professional networks to facilitate team-based care, and knowing when and where to refer patients, are key to all clinicians involved in best-evidence osteoarthritis care.41
Online resources and support
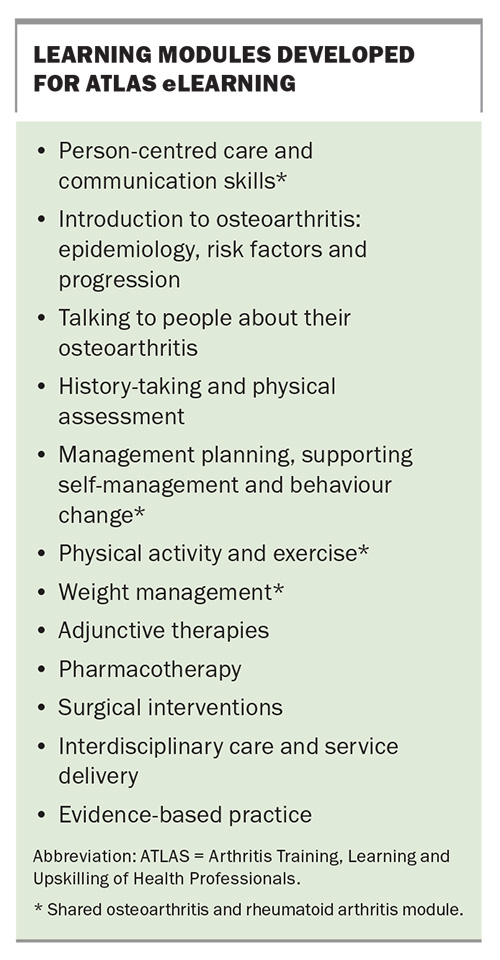
In settings where there are no interdisciplinary or multidisciplinary teams to collaborate and help deliver best-evidenced osteoarthritis care, clinicians can opt to use online resources and support when available. A new eLearning program for all health professionals has been launched to support the development of knowledge and skills in best-evidence osteoarthritis care: the Arthritis Training, Learning and Upskilling of Health Professionals program (ATLAS). ATLAS was developed as a result of the National Strategic Action Plan for Arthritis and the National Osteoarthritis Strategy, which identified seven priorities to ensure that all Australians at risk of or with osteoarthritis, regardless of where they are on their osteoarthritis journey, receive best-evidence care and support for self-management.10,42-44 ATLAS aims to help build workforce capacity to deliver the right arthritis care at the right time, with the right team and in the right place. The program features several learning streams for health professionals wanting to improve their knowledge and skills in arthritis care that include best-evidence management of both osteoarthritis and rheumatoid arthritis (RA). The learning content (Box) was developed by internationally renowned clinical and research experts in the area using a capability-driven approach and a core capabilities framework for health professionals delivering osteoarthritis care.36,45
A similar framework was used to develop the RA content, and some modules are common to both osteoarthritis and RA. These modules serve to provide knowledge to all healthcare professionals on best-evidence osteoarthritis care, particularly health professionals working in under-resourced settings where immediate expertise in the area from specialists and allied health professionals may not be readily available. For example, weight management is a core management strategy for people with osteoarthritis who are overweight or have obesity. However, some clinical settings may not have access to a dietitian or nutritionist who can support the person with osteoarthritis in their weight loss. The module on weight management provides evidence-based information on weight management strategies for people with osteoarthritis using the most up-to-date clinical guidelines and recently published high-quality papers, such as systematic reviews or randomised controlled trials. ATLAS learners have access to these publications, as well as downloadable patient-facing resources that they can give to their patients and support their practice. ATLAS is currently freely available for health professionals to use and can be accessed online (https://www.atlasarthritis.com.au).
Reliable, evidence-based and freely available consumer-facing resources can also be used to facilitate the delivery of and educate patients about best-evidence osteoarthritis care, such as:
- My Joint Pain or My OA (https://myoa.org.au/)
- Joint Action Podcast (https://www.jointaction.info/podcast)
- Arthritis Australia (https://arthritisaustralia.com.au/types-of-arthritis/osteoarthritis/)
- Osteoarthritis of the Knee (https://arthritisaustralia.com.au/wordpress/wp-content/uploads/2022/09/ArthAus_Osteoarthritis_knee_Sept
2022.pdf) - Versus Arthritis (https://versusarthritis.org/)
- Osteoarthritis Action Alliance (https://oaaction.unc.edu/en/).
Conclusion
Best-evidence, first-line osteoarthritis management involves lifestyle and behavioural interventions (such as education about osteoarthritis and how it is managed), techniques to support self-management, increasing physical activity and managing weight, if required. Interdisciplinary or multidisciplinary team approaches, similar to the OACCP, are considered the ‘gold standard’ for delivering the different elements of a tailored and person-centred management plan, where people with osteoarthritis are either managed in an interdisciplinary team or referred on to other disciplines with clinical expertise in other areas. However, not all settings may have access to other disciplines, and there are a whole host of other reasons why this may not be possible. Upskilling and training through education that uses evidence-based content and provides patient-facing supporting resources can help health professionals in under-resourced settings to deliver evidence-based osteoarthritis care. MT
COMPETING INTERESTS: Professor Hunter has been supported by an NHMRC Investigator Grant; is a Board Member for the Osteoarthritis Research Society International; provides consulting advice on Scientific Advisory Boards for Pfizer, Lilly, TLCBio and Novartis; is Editor in Chief for the Osteoarthritis and Cartilage section and Section Editor for Osteoarthritis at UpToDate; and has participated on a Data Safety Monitoring Board for Success trial for spinal stenosis (ACTRN12617000884303) and ICM-203 for knee osteoarthritis (NCT04875754). Dr Eyles has been supported by an NHMRC Investigator Grant. Dr Kobayashi: None.
References
1. Bijlsma JWJ, Berenbaum F, Lafeber FPJG. Osteoarthritis: an update with relevance for clinical practice. Lancet 2011; 377: 2115-2126.
2. Ackerman IN, Pratt C, Gorelik A, Liew D. Projected burden of osteoarthritis and rheumatoid arthritis in Australia: a population‐level analysis. Arthritis Care Res (Hoboken) 2018; 70: 877-883.
3. Steinmetz JD, Culbreth GT, Haile LM, et al. Global, regional, and national burden of osteoarthritis, 1990–2020 and projections to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Rheumatol 2023; 5: e508-e522.
4. Australian Institute of Health and Welfare (AIHW). Chronic musculoskeletal conditions: osteoarthritis 2024 [updated 17 June 2024]. Canberra: AIHW. Available online at: https://www.aihw.gov.au/reports/chronic-musculoskeletal-conditions/osteoarthritis (accessed February 2025).
5. Swain S, Coupland C, Sarmanova A, et al. Healthcare utilisation and mortality in people with osteoarthritis in the UK: findings from a national primary care database. Br J Gen Pract 2023; 73: e615-e622.
6. Zemedikun DT, Lee H, Nirantharakumar K, et al. Comorbidity phenotypes and risk of mortality in patients with osteoarthritis in the UK: a latent class analysis. Arthritis Res Ther 2022; 24: 231.
7. Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJK, Robertson BW. Patient dissatisfaction following total knee arthroplasty: a systematic review of the literature. J Arthroplasty 2017; 32: 3854-3860.
8. Ackerman IN, Skou ST, Roos EM, et al. Implementing a national first-line management program for moderate-severe knee osteoarthritis in Australia: a budget impact analysis focusing on knee replacement avoidance. Osteoarthr Cartil Open 2020; 2: 100070.
9. Bennell KL, Bayram C, Harrison C, et al. Trends in management of hip and knee osteoarthritis in general practice in Australia over an 11-year window: a nationwide cross-sectional survey. Lancet Reg Health West Pac 2021; 12: 100187.
10. Eyles JP, Hunter DJ, Briggs AM, et al. National osteoarthritis strategy brief report: living well with osteoarthritis. Aust J Gen Pract 2020; 49: 438-442.
11. The Royal Australia College of General Practitioners (RACGP). Guideline for the management of knee and hip osteoarthritis. 2nd ed. East Melbourne, Vic: RACGP. 2018.
12. Gray B, Gibbs A, Bowden JL, et al. Appraisal of quality and analysis of the similarities and differences between osteoarthritis clinical practice guideline recommendations: a systematic review. Osteoarthritis Cartilage 2024; 32: 654-665.
13. Bowden JL, Hunter DJ, Deveza LA, et al. Core and adjunctive interventions for osteoarthritis: efficacy and models for implementation. Nat Rev Rheumatol 2020; 16: 434-447.
14. Ackerman IN, Busija L. Access to self-management education, conservative treatment and surgery for arthritis according to socioeconomic status. Best Pract Res Clin Rheumatol 2012; 26: 561-583.
15. Mihalko SL, Cox P, Kobayashi S, Eyles JP. Core components of best evidence OA care: management planning, education, supporting self-management and behavior change. In: Hunter DJ, Eyles JP, editors. Osteoarthritis health professional training manual. Cambridge, Massachusetts: Academic Press; 2023. p. 55-72.
16. Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot 1997; 12: 38-48.
17. Weng Q, Goh S-L, Wu J, et al. Comparative efficacy of exercise therapy and oral non-steroidal anti-inflammatory drugs and paracetamol for knee or hip osteoarthritis: a network meta-analysis of randomised controlled trials. Br J Sports Med 2023; 57: 990-996.
18. Goh S-L, Persson MS, Stocks J, et al. Relative efficacy of different exercises for pain, function, performance and quality of life in knee and hip osteoarthritis: systematic review and network meta-analysis. Sports Med 2019; 49: 743-761.
19. Atukorala I, Makovey J, Lawler L, Messier SP, Bennell K, Hunter DJ. Is there a dose-response relationship between weight loss and symptom improvement in persons with knee osteoarthritis? Arthritis Care Res (Hoboken) 2016; 68: 1106-1114.
20. Messier SP, Resnik AE, Beavers DP, et al. Intentional weight loss in overweight and obese patients with knee osteoarthritis: is more better? Arthritis care res (Hoboken) 2018; 70: 1569-1575.
21. Henriksen M, Dai Z. Weight control. In: Hunter DJ, Eyles JP, editors. Osteoarthritis health professional training manual. Cambridge, Massachusetts: Academic Press; 2023. p. 95-109.
22. Webb EJ, Osmotherly PG, Baines SK. Physical function after dietary weight loss in overweight and obese adults with osteoarthritis: a systematic review and meta-analysis. Public Health Nutr 2021; 24: 338-353.
23. Allison K, Jones S, Hinman RS, et al. Alternative models to support weight loss in chronic musculoskeletal conditions: effectiveness of a physiotherapist-delivered intensive diet programme for knee osteoarthritis, the POWER randomised controlled trial. Br J Sports Med 2024; 58: 538-547.
24. Raynor HA, Champagne CM. Position of the academy of nutrition and dietetics: interventions for the treatment of overweight and obesity in adults. J Acad Nutr Diet 2016; 116: 129-147.
25. Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev 2005; 6: 67-85.
26. Gray B, Eyles JP, Grace S, et al. Best evidence osteoarthritis care: what are the recommendations and what is needed to improve practice? Clin Geriatr Med 2022; 38: 287-302.
27. Gibbs AJ, Gray B, Wallis JA, et al. Recommendations for the management of hip and knee osteoarthritis: a systematic review of clinical practice guidelines. Osteoarthritis Cartilage 2023; 31: 1280-1292.
28. French HP, Abbott JH, Galvin R. Adjunctive therapies in addition to land-based exercise therapy for osteoarthritis of the hip or knee. Cochrane Database Syst Rev 2022; 10: CD011915.
29. da Costa BR, Reichenbach S, Keller N, et al. Effectiveness of non-steroidal anti-inflammatory drugs for the treatment of pain in knee and hip osteoarthritis: a network meta-analysis. Lancet 2017; 390: e21-e33.
30. Liu X, Machado GC, Eyles JP, Ravi V, Hunter DJ. Dietary supplements for treating osteoarthritis: a systematic review and meta-analysis. Br J Sports Med 2018; 52: 167.
31. Kamaruzaman H, Kinghorn P, Oppong R. Cost-effectiveness of surgical interventions for the management of osteoarthritis: a systematic review of the literature. BMC Musculoskelet Disord 2017; 18: 183.
32. Skou ST, Roos EM, Laursen MB, et al. Total knee replacement and non-surgical treatment of knee osteoarthritis: 2-year outcome from two parallel randomized controlled trials. Osteoarthritis Cartilage 2018; 26: 1170-1180.
33. Riddle DL, Jiranek WA, Hayes CW. Use of a validated algorithm to judge the appropriateness of total knee arthroplasty in the United States: a multicenter longitudinal cohort study. Arthritis & Rheumatol 2014; 66: 2134-2143.
34. Dowsey M, Smith A, Choong P. Latent class growth analysis predicts long term pain and function trajectories in total knee arthroplasty: a study of 689 patients. Osteoarthritis Cartilage 2015; 23: 2141-2149.
35. Choong PFM, Dowsey MM. Surgery for osteoarthritis. In: Hunter DJ, Eyles JP, editors. Osteoarthritis health professional training manual. Cambridge, Massachusetts: Academic Press; 2023. p. 147-163.
36. Hinman RS, Allen KD, Bennell KL, et al. Development of a core capability framework for qualified health professionals to optimise care for people with osteoarthritis: an OARSI initiative. Osteoarthritis Cartilage 2020; 28: 154-166.
37. Teoh LS, Eyles JP, Makovey J, Williams M, Kwoh CK, Hunter DJ. Observational study of the impact of an individualized multidisciplinary chronic care program for hip and knee osteoarthritis treatment on willingness for surgery. Int J Rheum Dis 2017; 20: 1383-1392.
38. Agency for Clinical Innovation. Osteoarthritis Chronic Care Program Model of Care: Agency for Clinical Innovation; 2012. Sydney: Agency for Clinical Innovation. online at: https://aci.health.nsw.gov.au/__data/assets/pdf_file/0003/165306/ACI-MSK-Osteoarthritis-chronic-care-program-MOC.pdf (accessed February 2025).
39. Deloitte access economics. Osteoarthritis Chronic Care Program evaluation. 2014. Available online at: https://aci.health.nsw.gov.au/__data/assets/pdf_file/0004/338242/OACCP_Evaluation.pdf (accessed February 2025).
40. Körner M. Interprofessional teamwork in medical rehabilitation: a comparison of multidisciplinary and interdisciplinary team approach. Clin Rehabil 2010; 24: 745-755.
41. Bowden JL, Pratt C, Kobayashi S, van der Esch M. The interprofessional team, service delivery, and professional development. In: Hunter DJ, Eyles JP, editors. Osteoarthritis health professional training Manual. Cambridge, Massachusettes: Academic Press; 2023. p. 165-194.
42. Arthritis Australia. The National Strategic Action Plan for Arthritis. Australian Government Department of Health; 2019.
43. de Melo LRS, Hunter D, Fortington L, et al. National osteoarthritis strategy brief report: prevention of osteoarthritis. Aust J Gen Pract 2020; 49: 272-275.
44. Wang X, Hunter DJ, Dowsey M, et al. National osteoarthritis strategy brief report: advanced care. Aust J Gen Pract 2020; 49: 582-584.
45. Kobayashi S, Allen K, Bennell K, et al. A framework to guide the development of health care professional education and training in best evidence osteoarthritis care. Clin Geriatr Med 2022; 38: 361-384.