Is heartburn always reflux? An update on gastro-oesophageal reflux
Diagnosis of gastro-oesophageal reflux disease (GORD) is centred on patient-driven symptom reporting. However, some functional disorders can be indistinguishable from GORD based on symptoms. Lack of appropriate management of these functional disorders can lead to poor therapeutic response and quality of life, inappropriate use of proton pump inhibitors and frustration for the patient and doctor.
- Heartburn is one of the most common symptoms in patients presenting to GPs and may have a considerable impact on a patient’s wellbeing.
- The diagnosis of gastro-oesophageal reflux disease (GORD) is usually made clinically and a trial of a proton pump inhibitor (PPI) can be a pragmatic and helpful way of confirming this diagnosis.
- Confirmatory tests including gastroscopy, pH, pH-impedance and manometry are often required, especially if there is failure to respond to standard PPI dosing, diagnostic uncertainty or concern about complications.
- Symptoms of functional heartburn, reflux hypersensitivity and GORD can be clinically indistinguishable and further testing helps to clarify the diagnosis, reducing the risk of PPI overuse and promoting symptom improvement using functional treatment approaches.
- Patients with documented GORD who fail to respond to standard PPI dosing may require escalated medical treatment and consideration for antireflux surgery.
Reflux symptoms are common and the prevalence of gastro-oesophageal reflux disease (GORD) in general practice in Australia is estimated to be 11.6%, but is up to 20% in some populations.1,2 Far more patients may experience intermittent heartburn, which is often associated with diet, is usually nontroublesome and does not meet the diagnostic criteria for GORD.
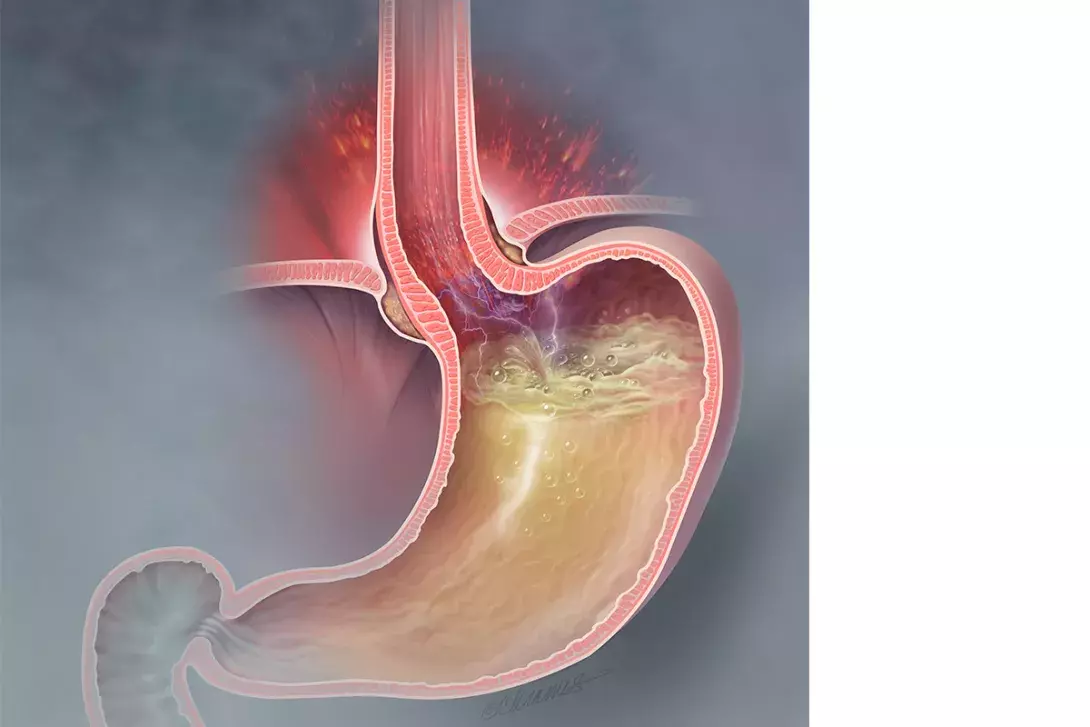
The Montreal consensus describes GORD as a condition that develops when the reflux of stomach contents causes troublesome symptoms and/or complications.3 GORD can be diagnosed either clinically, with patient-driven symptom reporting, or using investigations. The clinical diagnosis of GORD can be made based on symptoms alone if they are frequent (more than two episodes per week) or severe enough to impair quality of life. It can be confirmed on the basis of investigations that demonstrate reflux of gastric contents (e.g. gastroscopy, pH testing, impedance); however, these tests are not necessary for the diagnosis. Although further testing is not mandatory for diagnosis, it is often useful for clarifying the diagnosis when there are atypical features (including symptoms that are not responsive to proton pump inhibitors [PPIs]), assessing patients before surgery and determining the presence of complications. Complications reflect injurious effects of GORD and include oesophagitis, strictures, Barrett’s oesophagus and, rarely, oesophageal adenocarcinoma.
How patients present
The most characteristic symptoms of GORD are heartburn and regurgitation. Retrosternal burning is common and often occurs postprandially or when supine. Regurgitation is a cardinal symptom but can occur with varying degrees of severity. It may present as a bitter taste in the mouth, waterbrash or, in severe cases of volume reflux, with the regurgitation of food. Patients may present with dysphagia or odynophagia, but these symptoms may suggest a complication of GORD or an alternative diagnosis such as eosinophilic oesophagitis and should prompt endoscopic assessment.
Atypical presentations can occur but are far less common and often difficult to attribute to GORD alone. If patients present with atypical symptoms, alternative diagnoses should be considered and investigated. Atypical presenting symptoms and signs include noncardiac chest pain, laryngitis, chronic cough, asthma and dental erosions. The Montreal classification further includes proposed associations such as pharyngitis, sinusitis, idiopathic pulmonary fibrosis and recurrent otitis media; however, these are even less commonly associated with reflux and other causes should be sought primarily. Atypical chest pain, for example, should always prompt cardiac investigation as first-line management. If the chest pain occurred with typical symptoms of GORD (heartburn and regurgitation) and settled on taking an antacid or PPI, a diagnosis of GORD is likely.
Mechanisms for extra-oesophageal syndromes can be related to either direct effects of acid regurgitation (aspiration) or indirect effects, which are thought to be neurally mediated. Establishing causality for these syndromes can be clinically difficult, and it is accepted that GORD is rarely the sole cause of symptoms such as chronic cough, chronic laryngitis or asthma. Support for the premise that reflux is the sole cause of these atypical symptoms would come from complete resolution with treatment of reflux, which rarely happens.4
Diagnosis of GORD
Clinically, the approach to diagnosis of GORD is based on the patient’s description of their symptoms and their evaluation of how troublesome these symptoms are. Not only is heartburn a common presentation in general practice, but even mild symptoms on two or more days per week are associated with a significant reduction in quality of life.5 One problem with a patient-driven approach is that, clinically, symptoms of functional heartburn or functional dyspepsia can be indistinguishable from true reflux. The frequency, duration and severity of these disorders can be identical. Lack of awareness and appropriate management of these functional disorders leads to poor therapeutic response, inappropriate PPI use, poor quality of life and frustration for the patient and the treating doctor.
Endoscopy can be used to diagnose GORD and is particularly helpful for managing atypical presentations. It is important to recognise that endoscopy may still be inconclusive, particularly if the patient has already started taking a PPI, which may mask endoscopic findings of reflux. Furthermore, weakly acidic (defined as pH 4 to 6) or gaseous reflux is still defined as reflux but may not result in typical mucosal disruption patterns (erosions, erythema, ulceration, etc) used to diagnose GORD. If mild changes are seen, such as minor erosions or breaks in the distal oesophageal mucosa, these are not considered confirmatory of GORD as they may occur in people without evidence or symptoms of GORD and are subject to considerable interobserver variation (see ‘Typical endoscopic findings’, below).
Often, a pH study is required to measure the amount of acid exposure and correlate that carefully with symptom episodes to arrive at a true diagnosis. Acid exposure studies are usually conducted with a catheter-based probe inserted nasally and left in place for 24 hours. This test allows evaluation of the total time of acid exposure, the number of reflux events and the relationship between these acid events and the patient’s symptoms. Further detail about motility can be gained by oesophageal manometry, and this is usually performed with a pressure probe before the placement of the pH catheter. These studies require a high degree of patient co-operation. It is often very uncomfortable to have the probe placed and some patients struggle to keep it in for 24 hours. The patient also needs to carefully record the timing of their symptoms for correlation with acid exposure events. Patients may need to cease antireflux and promotility medication before this test, which is extremely difficult in some cases. Finally, access to this investigation in Australia is often problematic because the number of specialists who can perform and report on this procedure is limited.
A catheter-free or wireless capsule system allows an extended recording time, measuring frequency and duration of acid exposure events over 48 to 96 hours, but is less accessible and more expensive. It requires endoscopic attachment of a small device to the lower oesophageal wall. A small receiver can be used to record correlation between acid exposure and symptoms of heartburn, regurgitation and chest pain. Patients also complete a paper-based food and symptom diary.
Depending on the clinical scenario, pH monitoring is sometimes performed while the patient is taking a PPI and sometimes the PPI is withheld. For diagnostic purposes the best results are when patients withhold their PPI, but therapy is continued when assessing response to medication or the need for surgery in PPI nonresponders.
Impedance testing detects intraluminal bolus movement within the oesophagus and allows the detection of reflux independently of pH. It is useful for identifying nonacid reflux (pH >4), volume reflux or gaseous refluxate. It requires a specific impedance catheter to be placed intranasally.
When are investigations needed?
If a patient has typical symptoms of GORD and has responded to a trial of PPI no further investigation is generally necessary, although there are some scenarios where further investigation is recommended. A lack of response to a trial of PPI medication with appropriate dosing and adherence should prompt referral for a gastroscopy (Box).
At first presentation, there are several red flags that need to be screened for and should prompt immediate referral to a gastroenterologist for further investigation. These include weight loss, haematemesis, dysphagia, recurrent food bolus obstruction and anaemia. They are all suggestive of complications of GORD or an alternative diagnosis.
A gastroscopy should also be considered in patients with severe, changing or new symptoms, particularly in the elderly, current or ex-smokers, and if there is unexplained vomiting. If a gastroscopy is inconclusive, further testing with pH studies, impedance or manometry may be required. Investigation is always recommended before consideration for referral for antireflux surgery.
Typical endoscopic findings
Reflux oesophagitis is defined endoscopically by breaks in the distal mucosa. Conventionally, the Los Angeles (LA) classification of reflux oesophagitis is used to grade the severity of these mucosal changes (Figure).6 Although this should be straightforward owing to the high-quality, high-resolution gastroscopes available, the endoscopic diagnosis of GORD is somewhat fraught. There is considerable interoperator variability that leads to confusion, particularly at the very mild end of the spectrum. Patients with severe symptoms may have minimal changes endoscopically. Only 30% of patients presenting with heartburn have erosive changes, and this reduces further to under 10% if they are already taking a PPI.7 It is also recognised that many patients with low-grade changes of oesophagitis (LA grade A or B) may not have any symptoms of reflux. Mucosal breaks at this level of severity may be intermittent and the grade of mucosal injury may correlate poorly with symptoms.8
Most people with reflux symptoms presenting for endoscopy have grade A or B changes, which are considered inconclusive or borderline for the endoscopic diagnosis of GORD. These lower grades of oesophagitis with less erosive features are considered nonspecific and are subject to interobserver variation.9 Further confirmatory testing with pH studies may be required.
As such, the Lyon consensus has concluded that only grade C and D changes provide confirmatory evidence of GORD. Grade C reflux oesophagitis is defined by one or more mucosal breaks that are continuous between the tops of two or more mucosal folds but involve less than 75% of the circumference, which is quite severe oesophagitis. Grade C and D changes are seen infrequently, especially as most patients will have trialled a PPI before endoscopy, which usually downgrades the severity of mucosal changes.
Peptic stricturing and Barrett’s oesophagus also confirm oesophagitis. Endoscopy may be particularly helpful when there is concern about complications, for assessing possible hiatus hernia, or before considering surgery. It is, however, not required for a diagnosis. If there is doubt about the diagnosis at endoscopy or failure to respond to PPI after endoscopy, a 24-hour pH study will be helpful in clarifying whether the diagnosis is GORD, reflux hypersensitivity or functional heartburn.
Does a normal gastroscopy result rule out reflux?
Of patients who present with heartburn and go on to have an endoscopy, 30% have erosive oesophagitis and 70% have normal, findings.10 Of those with normal endoscopy results, if pH testing is pursued, about half have an abnormal pH test result and are diagnosed with nonerosive reflux disease. There is also recognition that refluxate can be weakly acidic or gaseous and impedance testing may be required to define this further.
If endoscopy findings are normal or inconclusive and a pH test result is normal then the diagnosis is either reflux hypersensitivity or functional heartburn, depending on whether patient-perceived symptoms correlate to any reflux events over the 24 hours of testing. A positive correlation indicates reflux hypersensitivity and a negative correlation indicates functional heartburn.
Functional heartburn and reflux hypersensitivity
Definitions
Many patients with symptoms of heartburn have a functional oesophageal disorder. Rome IV, the peak body that classifies disorders of the brain–gut interaction, recognises five functional oesophageal disorders; functional chest pain, functional heartburn, reflux hypersensitivity, globus and functional dysphagia. Functional heartburn and reflux hypersensitivity both present with symptoms of heartburn in the absence of significant endoscopic changes or evidence of excessive acid exposure. Functional heartburn is the most common explanation for failure of PPI therapy.11 Symptoms of functional heartburn are theorised to result from hypersensitivity of the visceral nerves of the oesophagus, which may be exacerbated by central sensitisation, hypervigilance, stress and anxiety.12
According to the current Rome IV criteria (https://theromefoundation.org/rome-iv/rome-iv-criteria), patients with functional heartburn:
- report retrosternal discomfort or pain at least twice per week over the past six months
- show no response to optimal PPI therapy
- show no evidence that symptoms are due to GORD, eosinophilic oesophagitis or a major oesophageal motor disorder.
To satisfy these criteria, patients must have normal gastroscopy findings and biopsies of the oesophagus must exclude eosinophilic oesophagitis. Essentially, the gastroscopy needs to be normal; the need to exclude eosinophilic oesophagitis is somewhat controversial, given the low incidence of this condition in patients who do not present with dysphagia. Also somewhat controversial, oesophageal manometry and a pH study, which may not always be easily accessible, are required to rule out abnormal acid exposure or a major motor disturbance of the oesophagus such as achalasia or spastic oesophageal conditions (diffuse oesophageal spasm, jackhammer oesophagus, etc).
Reflux hypersensitivity presents similarly to functional heartburn; however, on pH or pH-impedance testing, as mentioned above, there is evidence of triggering of symptoms by reflux events despite normal acid exposure time (i.e. less than 4%). That is, even though these patients do not meet the set threshold for total acid exposure, they still correlate their symptoms with events of acid exposure or reflux. Brief acid exposure is considered physiological and within normal limits, but these patients directly correlate such events with the generation of symptoms. Some consider this an overlap syndrome between GORD and functional heartburn. Partial responsiveness to a PPI does not exclude the diagnosis of reflux hypersensitivity. Patients often require further management to address the hypersensitivity.
Management
Management of functional heartburn or reflux hypersensitivity requires a clear diagnosis and explanation for the patient. They should be reassured that their condition is not dangerous and that progression to complications or malignancy (in the absence of Barrett’s oesophagus) is uncommon. Treatment is usually focused on reducing hypersensitivity and pain perception. Neuromodulators such as low-dose tricyclic antidepressants (off-label use) are often effective in addressing this. There is evidence that nonpharmacological approaches such as cognitive behavioural therapy or gut-directed hypnotherapy are beneficial. There is some emerging evidence that a low-FODMAP diet improves symptoms in patients with functional heartburn.13
Treatment of GORD
The aim of treatment for GORD is symptom control and prevention of complications of reflux (Flowchart). Mild symptoms may respond to dietary and lifestyle modification but most people who meet the clinical diagnosis of GORD (troublesome, frequent symptoms) require medication in addition to lifestyle measures. Endoscopy can be a useful tool for stratifying the risk of complications and the need for long-term PPI therapy.
Effectiveness of lifestyle measures
In people with mild reflux symptoms, lifestyle measures and dietary changes may provide effective treatment. It is particularly useful if the patient can recognise a precipitant and avoid it. Lifestyle advice includes weight loss, elevating the head of the bed, eating small meals, reducing intake of alcohol, caffeine, fatty foods, spicy foods, carbonated drinks and citrus, and stopping smoking. These measures need only be continued if they are controlling symptoms.
If a patient has more troublesome symptoms, dietary and lifestyle factors alone are generally insufficient for symptom control. There is some evidence that smoking and intake of alcohol, chocolate, fatty foods and citrus may adversely affect oesophageal pH, but there is little evidence that their cessation leads to clinical improvement.14 Elevating the head of the bed and weight loss have been associated with improvement in GORD symptoms but are often difficult to maintain over the longer term.
If symptoms are mild, on-demand dosing of antacids or PPIs may be appropriate; however, if patients have frequent or troubling symptoms they should be prescribed regular PPI therapy.
Effectiveness of a PPI trial
A PPI trial is probably equivalent to a history given to a GP or gastroenterologist in terms of sensitivity and specificity for diagnosing GORD but is pragmatic and may help avoid unnecessary endoscopies. A trial of a PPI is generally recommended and is endorsed by Australian guidelines. PPIs are accessible, inexpensive and safe, and a trial may provide both relief from symptoms and confidence in the diagnosis. It must be recognised, however, that a PPI trial has a low specificity and high placebo response.15 The drawbacks of this approach are the overdiagnosis of GORD and, ultimately, overuse of PPI medication.
PPI therapy
PPIs can be used to control symptoms and, additionally, response to PPIs can help confirm the clinical diagnosis of GORD. They can also help prevent complications of GORD, and an endoscopy may be helpful to assess the need for this.
A trial of a PPI generally involves four to eight weeks of standard dosing (Table). The recommended regimen is orally, once daily before meals (preferably half an hour before). The PPI can be taken either before breakfast or before dinner, depending on the pattern of symptoms that the patient has.
If symptom control is achieved, a slow step down to maintenance dosing should be recommended. This will hopefully avoid rebound hyperacidity, which is often seen after abrupt withdrawal of a PPI. It also allows for the lowest possible dosing to maintain symptom control. If long-term PPI therapy is required, its indication and clinical benefit should be regularly reassessed.
Is there a role for histamine 2 receptor antagonists?
Histamine 2 receptor antagonists have been part of the treatment for GORD since the 1970s; however, in the era of PPIs there is little evidence for their use as a first-line agent. They are often useful and occasionally overlooked as a good option for anyone who is intolerant of PPI therapy or worried about side effects, or for providing additional antacid effect for patients whose symptoms are incompletely controlled by PPI therapy. Agents such as nizatidine appear to have some promotility action, which can be helpful in patients who have symptoms of dysphagia related to GORD. They possibly carry a lower risk of osteoporotic fracture, but their efficacy is inferior to that of PPIs.
What to do when PPIs fail
If a patient has had an adequate trial of PPI at standard dosing with adherence assessed and they have failed to respond, they should be referred for a gastroscopy.
If GORD has been confirmed and they have persistent symptoms, treatment should be escalated. Options for treatment escalation include:
- revisit lifestyle factors; encourage weight loss where appropriate
- increase PPI dose; twice-daily dosing may be most effective
- add a histamine-2 receptor antagonist
- consider a promotility agent (e.g. domperidone)
- consider surgical referral for treatment of nonresponsive patients or patients with severe symptoms.
PPIs only have therapeutic benefit for functional heartburn symptoms in patients with a GORD overlap syndrome. Treatment should be directed toward the functional paradigm addressing psychological comorbidity, looking at lifestyle measures, diet, neuromodulators and possible hypnotherapy.
Antireflux surgery
Antireflux surgery should be considered in patients who have persistent or recurrent symptoms and/or complications despite medical therapy. The aim of surgery is to maximise control of reflux with minimal risk of side effects; and with this in mind, either a Nissen fundoplication or partial fundoplication is considered. Side effects of surgery include dysphagia, odynophagia, bloating and flatulence as well as an inability to belch. Many patients experience a recurrence of reflux symptoms over time, and in the long term after surgery at least 50% of patients require ongoing PPI at least intermittently.16 In general, partial fundoplication has slightly lower side effects but higher rates of reflux recurrence. Patients with established Barrett’s oesophagus require ongoing surveillance after fundoplication as there is still controversy regarding whether the procedure can reliably lead to regression of Barrett’s oesophagus or prevent progression to dysplasia or adenocarcinoma. There is no role for antireflux surgery in functional heartburn.
Conclusion
In clinical practice GORD is diagnosed based on symptoms reported by the patient. The hallmarks of GORD are troublesome heartburn and regurgitation. Chest pain may also be a presenting symptom. It is important to also consider extraoesophageal syndromes such as laryngitis, cough, asthma and dental erosions. Complications should be screened for and include stenosis or stricture, Barrett’s oesophagus and adenocarcinoma. PPIs are the recommended treatment in patients with GORD who are at risk of complications, and ultimately they should be down-titrated to the lowest effective dose. Not all patients presenting with symptoms of reflux have GORD, however; and a lack of response to a trial of PPI should prompt further evaluation. Many of these patients have functional heartburn or oesophageal hypersensitivity and treatment should be directed toward a functional paradigm. MT
COMPETING INTERESTS: None.
