What’s the diagnosis?
A returned traveller with a tattoo rash

Case presentation
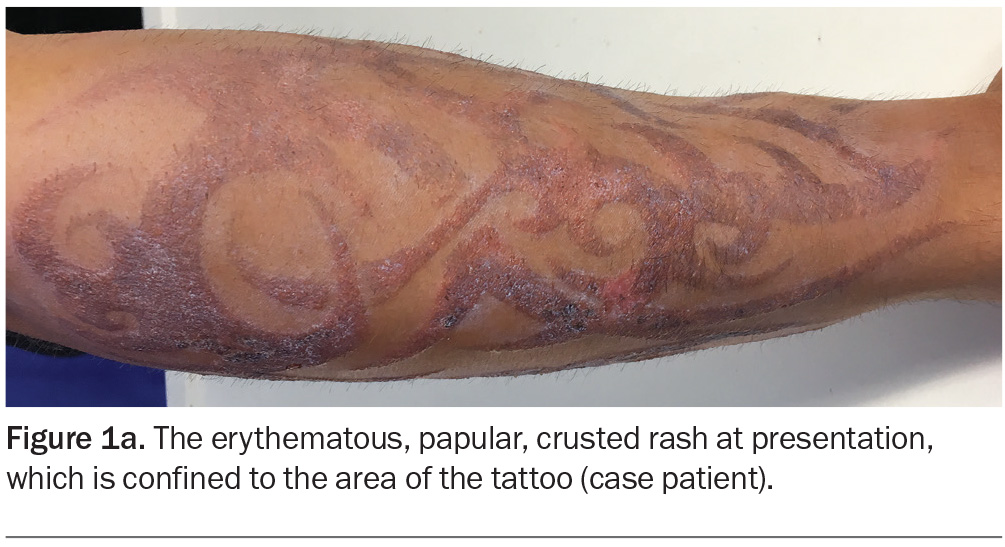
A 22-year-old man presents with a one-week history of an erythematous, papular and crusted rash on his arms following application of a temporary tattoo on each arm (Figure 1a). The rash is confined to the area of the tattoo and is pruritic but not tender. He has no significant past medical history.
The tattooing was performed 12 days earlier in Bali. The patient reports that he had been travelling with two friends who developed a similar cutaneous reaction, although this could not be confirmed. He indicated that they too had experimented with temporary tattoos while in Bali; however, these were applied at different times and locations.
Differential diagnoses
Conditions to consider among the differential diagnoses include the following.
Lichenoid tattoo reaction
Reactions to the red pigments in tattoos are well recognised. The lichenoid pattern is the most common histological type and is believed to be an expression of delayed hypersensitivity.1 Papules and plaques may occur weeks or even years after the tattooing procedure.
For the case patient, this diagnosis could be excluded because red inks were not used in his tattoo.
Atypical mycobacterial infection
Mycobacteria are acid-fast bacilli that vary in shape, as either coccobacilli or rods.2 Atypical mycobacteria, which are defined as mycobacteria other than Mycobacterium tuberculosis complex and Mycobacterium leprae, occur naturally in the environment. These mycobacteria are found primarily in water and wet soil, and can cause infections of the skin and soft tissues through transmission by inoculation.3 Clinical presentations include pustules, keratotic plaques and ulcers. Skin lesions tend to be localised in immunocompetent individuals but may occur as disseminated mucosal and cutaneous lesions in an immunocompromised host. The diagnosis is established through Ziehl-Neelsen histochemical staining, culture and polymerase chain reaction (PCR) testing.3
For the case patient, this was not the diagnosis. His rash was limited to the area of the tattoo, whereas atypical mycobacterial skin infections generally are not well-demarcated.
Granulomatous reaction
This diagnosis should be considered for a patient with a permanent tattoo. Allergic granulomatous reactions can be caused by metal salts in the pigments of permanent tattoos – culprits include mercury (red colour), chromium (green), cobalt (blue) and cadmium (yellow).4 Granulomatous reactions are rare, appearing as erythema, induration, papules and nodules a few days after application of the tattoo, and can persist for years. There are two typical histological patterns of granulomatous reactions: the foreign body type (characterised by pigment-filled giant cells) and the sarcoidal type (characterised by dense aggregates of epithelioid histiocytes, a thin peripheral ring of lymphocytes and a few giant cells).5
For the case patient, this diagnosis could be excluded because there was no induration and no nodules were present.
Allergic contact dermatitis
This is the correct diagnosis. The patient’s temporary tattoo contained ‘black henna’, which is a combination of para-phenylenediamine (PPD) and henna, a powdered leaf widely used as a dye for skin and hair in Islamic and Hindu cultures. During the past 20 years, temporary black henna tattoos have become popular among children, adolescents and young adults in Western countries and are typically available in holiday resort areas, theme parks, festivals and fairs globally.6,7
PPD is a potent allergen and, depending on concentration and duration of exposure, can elicit a type IV delayed hypersensitivity reaction.6 The concentration of PPD in black henna dye mixtures has been shown to range between 2 and 29.5%, and a single tattoo may be sufficient to induce PPD sensitisation. Black henna tattoos induce contact allergy to PPD at an estimated frequency of 2.5%.7 Exposure to PPD can also cause cross-sensitisation to structurally similar substances, such as azo dyes, parabens, rubber chemicals and benzocaine in local anaesthetic.
Allergic contact dermatitis presents one to three days after the application of a black henna tattoo if the patient is already sensitised to PPD, or four to 14 days after application if the patient is newly sensitised by the tattoo ink.8,9 Common clinical manifestations include erythema, oedema, vesicles, papules and bullae. Postinflammatory hypo- or hyperpigmentation may also occur.9 Scarring has been observed in some cases.
A clinical diagnosis of allergic contact dermatitis caused by PPD can be confirmed by patch testing, starting with a PPD concentration of 0.01%. Results of patch testing can inform the avoidance of substances encountered through occupational exposure (e.g. printers, hairdressers, industrial chemists and workers in rubber, leather and textile manufacturing industries).9 A biopsy can be considered if the diagnosis is still uncertain.
Management
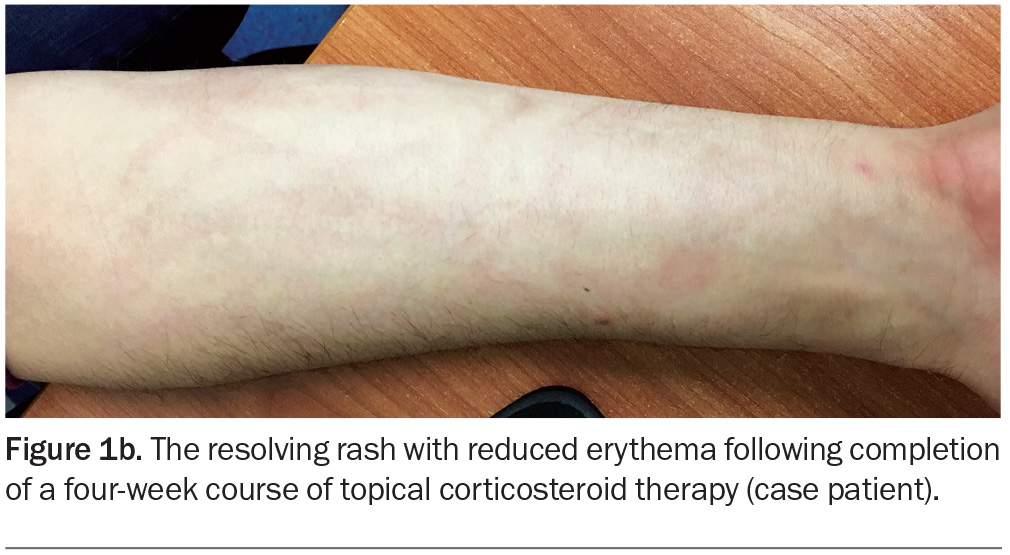
Hypersensitivity reactions to temporary tattoos are transient – treatment with potent topical corticosteroids (and time) will generally allow a reaction to resolve. If the reaction is severe then systemic corticosteroids can be prescribed in conjunction with topical corticosteroids.10 Affected patients should be counselled to avoid exposure to PPD and PPD-related compounds, which are found in cosmetic products such as hair dyes and semi-permanent eyebrow makeup.9
Outcome
The case patient had a moderate to severe inflammatory reaction to the black henna tattoo and was diagnosed with allergic contact dermatitis to PPD. Patch testing was not performed because there was strong clinical suspicion of PPD as the agent causing sensitisation. The rash responded well to a four-week course of betamethasone dipropionate 0.05% cream (Figure 1b).
Prevention
In most countries, the composition of black henna dye and the practice of henna tattoo applications by artists are unregulated.9 In Australia, use of this substance on client’s skin is illegal.11
The present case was reported to the Department of Foreign Affairs and Trade in Australia, which led to fortifying of the existing travel alert for temporary black henna tattoos (see https://www.dfat.gov.au/travel). Regular provision of information to travellers by health authorities and specialists can raise awareness of the risk of black henna tattoo reactions.9 MT
COMPETING INTERESTS: None.
References
1. Dang M, Hsu S, Bernstein E. Lichen planus or lichenoid tattoo reaction? Int J Dermatol 1998; 37: 860-861.
2. Bacterial colonizations and infections of skin and soft tissues [Section 25]. In: Fitzpatrick’s Color atlas and synopsis of clinical dermatology, 8th ed. Wolff K, Johnson RA, Saavedra AP, Roh E. New York, NY: McGraw-Hill Education; 2017.
3. Mycobacterial infections [Chapter 75]. In: Dermatology, 4th ed. Bolognia J, Schaffer JV, Cerroni L (eds). Philadelphia, PA: Elsevier; 2018.
4. Allergic contact dermatitis [Chapter 128]. In: Rook’s Textbook of dermatology, 9th ed. Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer D (eds). West Sussex: John Wiley & Son; 2016.
5. Tourlaki A, Boneschi V, Tosi D, Pigatto P, Brambilla L. Granulomatous tattoo reaction induced by intense pulse light treatment: granulomatous tattoo reaction. Photodermatol Photoimmunol Photomed 2010; 26: 275-276.
6. Rogers C, King D, Chadha L, Kothandapani JSG. ‘Black henna tattoo’: art or allergen? BMJ Case Rep 2016; bcr2015212232.
7. de Groot AC. Side-effects of henna and semi-permanent ‘black henna’ tattoos: a full review. Contact Derm 2013; 69: 1-25.
8. Calogiuri G, Di Leo E, Butani L, Pizzimenti S, et al. Hypersensitivity reactions due to black henna tattoos and their components: are the clinical pictures related to the immune pathomechanism? Clin Mol Allergy 2017; 15: 8.
9. Atwater AR, Bembry R, Reeder M. Tattoo hypersensitivity reactions: inky business. Cutis 2020; 106: 64-67.
10. Encabo Durán B, Romero-Pérez D, Silvestre Salvador JF. Allergic contact dermatitis due to paraphenylenediamine: an update. Actas Dermosifiliogr (Engl Ed) 2018; 109: 602-609.
11. Government of Western Australia Department of Health. Henna tattooing: Available online at: https://www.health.wa.gov.au/Articles/F_I/Henna-tattooing (accessed June 2023).