Metastatic melanoma: an update on treatment therapies
Metastatic melanoma is a common cancer in Australia, with BRAF gene mutations present in 40% of cutaneous melanomas. Therapies for metastatic melanoma have rapidly evolved over the past decade and include targeted molecular therapies and immunotherapies. Although these therapies greatly improve patient outcomes, they have unique toxicity profiles and the treating oncologist, in discussion with the patient, is best placed to manage these.
- Targeted therapy and immunotherapy have significantly improved survival for advanced melanoma since 2010.
- Testing for a BRAF gene mutation is now standard practice in advanced melanoma to guide therapeutic decision-making.
- If advanced melanoma is BRAF mutation positive, targeted therapy with combination BRAF/MEK inhibitors is an effective therapeutic option, either as first- or second-line therapy.
- Immunotherapies that inhibit immune checkpoints can also be used to treat advanced melanoma.
- Immunotherapies significantly improve survival and may lead to enduring disease control for a proportion of patients.
- Toxicities with targeted therapies are predictable.
- Immune-related toxicities from immunotherapy are unpredictable and require a high index of suspicion, particularly within the first three to four months of starting treatment.
- The treating medical oncologist should always be involved in managing therapy-induced toxicities.
Melanoma is a common cancer in Australia, with historically poor prognosis for patients with advanced disease. Cutaneous melanoma was the fourth most commonly diagnosed cancer in both men and women in 2019.1 In 2018, 2094 people died from melanoma in Australia. The median age at death was 77.5 years.2 Melanoma was also the most commonly diagnosed cancer in young Australians (aged 15 to 24 years) between 2010 and 2014, accounting for 15% of all cancers diagnosed.3
The therapeutic landscape for metastatic melanoma has evolved rapidly in the past 10 years. Until recently, cytotoxic chemotherapy with dacarbazine was the standard treatment, even though a survival benefit with this drug has never been demonstrated in clinical trials. Prognosis for advanced disease was extremely poor with dacarbazine therapy, with a median overall survival of just seven months, and only 25% of patients surviving longer than 12 months following diagnosis.4 Since 2013, the survival rate in patients with advanced melanoma has improved. This is because of the development of two different classes of systemic treatment; molecularly targeted drugs and immunotherapies, which allows many patients to achieve long-term control of their disease. This article discusses specific targeted and immunotherapies available in Australia, including combination therapies in the context of their efficacy in clinical trials.
Genetic mutations in melanoma
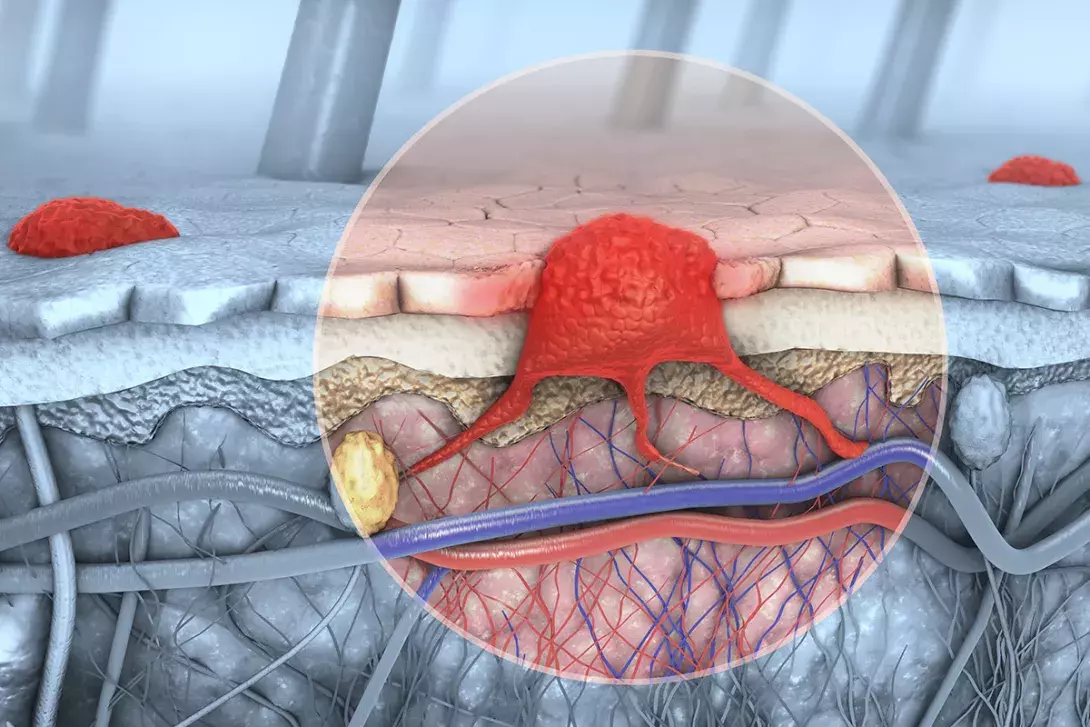
About 40% of all skin melanomas harbour a mutation in a gene called BRAF.5 The BRAF gene synthesises a protein that sends intracellular signals to promote cell growth. When the BRAF gene is mutated in melanoma cells (BRAF mutation positive), there is expression of an abnormal BRAF protein kinase within the mitogen-activated protein (MAPK) pathway (Figure 1).6,7 This promotes continuous cell growth and malignant transformation.
Testing for BRAF mutations is now standard practice in newly diagnosed advanced melanoma. There are several different BRAF gene mutations, the most common being V600E followed by V600K and V600R/D.6,8 Melanoma that does not harbour a BRAF mutation is referred to as BRAF wild-type (BRAF mutation negative). The discovery that activating BRAF mutations serve as oncogenic drivers in melanoma has led to the development of molecularly targeted treatment approaches.
BRAF inhibitors
BRAF inhibitors are drugs that block the abnormal BRAF protein kinase and aim to slow the growth of melanoma cells (Figure 1).7 There were two landmark clinical trials that showed a significant survival benefit with BRAF inhibitors compared with dacarbazine.9,10 Despite crossover in both studies, progression-free survival (PFS), overall response rates (ORR) and overall survival (OS) were superior using the targeted agents in patients with BRAF mutant melanoma. The ORR is defined as the proportion of patients with a reduction in size of the tumour of 30% or more from baseline.
Vemurafenib
Vemurafenib was the first BRAF inhibitor to demonstrate superior efficacy in metastatic melanoma. In 2010, a phase I dose escalation study with vemurafenib in patients with BRAF V600E-mutant melanoma found that with treatment, 81% of patients had a complete or partial response.11 A subsequent phase III trial reported in 2011 compared vemurafenib with dacarbazine in 675 patients who had not received any previous treatment. Vemurafenib improved median OS from nine months to 13.6 months.12
Dabrafenib
Clinical trials with dabrafenib in patients with BRAF mutant metastatic melanoma showed similar results to the trials with vemurafenib.9,13 The ORR with dabrafenib was 50% and median OS improved from nine months using dacarbazine to 18 months with dabrafenib.9 In December 2013, Dabrafenib was the first BRAF inhibitor to be listed on the PBS in Australia for patients with BRAF mutant metastatic melanoma.
Encorafenib
Encorafenib is a second-generation BRAF-targeted inhibitor and was listed on the PBS in April 2020. Encorafenib inhibits the MAPK pathway in melanoma cells that express several BRAF mutations (V600E, V600K and V600D/R). It has a much longer dissociation half-life compared with either dabrafenib or vemurafenib and this allows sustained target inhibition.14
Combination BRAF and MEK inhibition
Despite promising results with BRAF inhibitors, resistance to these therapies inevitably limits the duration of response to treatment when they are used as monotherapy. Using BRAF inhibitors in combination with other targeted drugs has proven successful in the treatment of metastatic melanoma.
The main mechanism by which melanoma cells escape BRAF inhibition is by reactivation of the MAPK pathway via MEK gene activation.6 The MEK gene produces enzymes that are downstream from BRAF in the MAPK pathway (Figure 1).7 Drugs that block the MEK enzymes therefore block this escape signal pathway. Dual inhibition of BRAF and MEK genes helps to slow malignant cell growth in BRAF mutant melanomas and leads to superior clinical results compared with BRAF inhibition alone. As such, BRAF inhibitors are now used in combination with MEK inhibitors to treat patients with advanced BRAF mutant melanoma.
Four landmark studies (COMBI-D, COMBI-V, Co-BRIM and COLUMBUS) evaluated combination BRAF/MEK inhibition and are summarised in Table 1.15-18 To date, these trials have shown the highest response rates to therapy in patients with melanoma. Compared with BRAF monotherapy, the average improvement in PFS is three to seven months with combination therapy. OS is improved by seven to 16 months with combination BRAF/MEK inhibition (depending on the specific combination). Combination therapy is now the standard of care for patients with BRAF mutant metastatic melanoma. However, the clinical utility of BRAF/MEK inhibitors is often limited by the duration of response with these therapies and treatment resistance is inevitable. Preventing resistance to targeted therapies has been studied extensively but has proven difficult to overcome.19
Trametinib
Trametinib was the first MEK inhibitor to be approved in Australia. A phase III randomised trial of dabrafenib in combination with trametinib versus dabrafenib alone found improved PFS, ORR and OS with the combination therapy. The median OS with combination treatment improved to 26 months, from almost 19 months with dabrafenib alone.15 In this trial, five-year survival was also highest among patients with good prognostic factors, which included a normal baseline lactose dehydrogenase level and fewer than three sites of metastatic disease.20 The combination of dabrafenib and trametinib compared with vemurafenib monotherapy was similarly found to have improved OS.16,20
Cobimetinib
Cobimetinib is used in combination with vemurafenib. Results from clinical trials found that there was a similar survival benefit to that seen with a dabrafenib/trametinib combination for patients with BRAF mutant metastatic melanoma.17,21
Binimetinib
The combination of binimetinib with encorafenib has demonstrated the longest disease control of any BRAF/MEK inhibitor combination. The results from the landmark COLUMBUS clinical trial were published in 2018. The median OS was 33.6 months for patients with BRAF mutant metastatic melanoma who received this combination compared with 16.9 and 23.5 months for those who received vemurafenib and encorafenib monotherapy, respectively (Table 1).18
Targeted therapy toxicity
BRAF/MEK inhibitors are generally well tolerated. The three different combinations (dabrafenib/trametinib, cobimetinib/vemurafenib and encorafenib/binimetinib) each have several unique side effects (Table 2).22 In particular, encorafenib/binimetinib has a much lower rate of photosensitivity and febrile events compared with the other combinations.
Immunotherapy
Immunotherapy aims to modulate a patient’s own immune response to tumour cells. This occurs by targeting certain checkpoints within the immune cascade, also referred to as immune checkpoint inhibition (ICI). Immunotherapy has dramatically improved survival for patients with both BRAF mutant and BRAF wild-type advanced melanoma.
There are two main immune checkpoints that are inhibited by immunotherapies in melanoma: cytotoxic T lymphocyte- associated antigen 4 (CTLA-4) and programmed cell death-1 (PD-1). CTLA-4 and PD-1 are immune checkpoint molecules that normally function to downregulate T cell activation (Figure 2).7,23,24 This is an important mechanism for immune tolerance and is the main reason why immunotherapies have side effects.
T cell activation is a complex process. Both CTLA-4 and PD-1 binding have similar negative effects on T cell activity, but the timing of downregulation, mechanisms of signalling and anatomic locations of immune inhibition by the two checkpoints differ.25 CTLA-4 inhibition is confined to T cells at the initial or priming phase of T cell activation, typically in lymph nodes. PD-1 is more broadly expressed on activated T cells, B cells and myeloid cells and functions during the later stage of the immune response, predominantly within peripheral tissues.26
CTLA-4 inhibitors
Ipilimumab
CTLA-4 is expressed on immune cells and its normal function is to inhibit T cell activation. Ipilimumab is a CTLA-4 inhibitor that blocks the interaction between CTLA-4 and cytotoxic T cells, allowing T cells to proliferate in an uninhibited manner.24 Cytotoxic T cells can then target and destroy melanoma cells (Figure 2).7
The potential for ICIs in treating cancer has been demonstrated in a 2010 clinical trial and subsequent follow-up studies. In the 2010 phase III trial, patients with advanced melanoma who had already received dacarbazine demonstrated a survival benefit with ipilimumab therapy (3 mg/kg) compared with an antimelanoma vaccine (gp100).27 A follow-up trial compared a higher dose of ipilimumab (10 mg/kg) in combination with dacarbazine with dacarbazine alone. The median OS was longer for patients receiving the ipilimumab/dacarbazine combination compared with those receiving dacarbazine alone (11 vs 9 months, respectively).28 The five-year survival rate for patients on ipilimumab/dacarbazine therapy was 18% compared with 9% in patients who only received chemotherapy.29 Ipilimumab 3 mg/kg was listed on the PBS for advanced melanoma in August 2013.
PD-1 inhibitors
Monoclonal antibodies that target other checkpoints within the immune system, including PD-1, can also be manipulated to improve survival in melanoma. PD-1 is a key inhibitory receptor expressed on the surface of activated T and B cells.6 Tumour cells express the PD-1 ligand (PD-L1). Normally, when the PD-1 receptor binds to PD-L1 an effective antitumour immune response is prohibited. Anti-PD-1 receptor antibodies work by binding to the PD-1 receptor, which blocks the inhibitory immune signal. This allows ongoing T cell activation. In essence, ICIs ‘release the breaks’ on immune tolerance, which creates an antitumour immune response.30
Pembrolizumab
A phase III trial (KEYNOTE-006) compared different dosing schedules of pembrolizumab with ipilimumab as first-line treatment for patients with advanced melanoma. After five years follow up, median OS was almost 17 months longer for patients taking pembrolizumab than those taking ipilimumab (32.7 vs 15.9 months, respectively) (Table 3).31 Pembrolizumab is administered at a fixed dose of 200 mg every three weeks for metastatic melanoma.
Nivolumab
Nivolumab has been shown to substantially improve overall survival for patients with BRAF wild-type metastatic melanoma compared with dacarbazine. After five years follow up, the median OS was 37.5 months for patients receiving nivolumab versus 11.2 months for those receiving dacarbazine, respectively (Table 3).32 There were also fewer adverse events with nivolumab compared with chemotherapy in this trial. Nivolumab is administered at a fixed dose of 480 mg every four weeks for metastatic melanoma.
Combination immunotherapy
Combining CTLA-4 inhibitors with PD-1 inhibitors has superior efficacy compared with ICI monotherapy. The landmark study for ICI combination was the CHECKMATE-067 trial. This study compared nivolumab in combination with ipilimumab with nivolumab monotherapy and ipilimumab monotherapy. The ipilimumab/nivolumab combination conferred a significant improvement in survival compared with monotherapy. After five years follow up, the median OS was not reached but the impressive survival rate was 52%. Combination ipilimumab/nivolumab also has the highest ORR seen with immunotherapy (Table 3).33 The long-term data also proved that patients who are treated with nivolumab, as monotherapy or in combination with ipilimumab, had superior outcomes compared with ipilimumab alone. This was irrespective of BRAF status.34 The combination of ipilimumab and nivolumab has set a survival benchmark for first-line therapy in metastatic melanoma.
Immunotherapy toxicity
Immunotherapy has a unique toxicity profile that is distinct from traditional cytotoxic chemotherapies. Depending on the immune checkpoint(s) targeted, the incidence and severity of toxicity varies. Immune-related adverse events (irAEs) are unpredictable and can affect any organ or tissue, although some irAEs occur more commonly than others (Table 4). The most frequently occurring irAEs affect skin, colon, endocrine organs, liver and lungs.34 Immune-related endocrinopathies are irreversible and require lifelong hormonal replacement. The onset of irAEs also varies, but usually occurs early, within weeks to three months after initiation of ICIs.34
The early clinical trials with ipilimumab helped our understanding of dose-related toxicities associated with immunotherapy. A large trial compared doses of ipilimumab (3 mg/kg vs 10 mg/kg).35 The higher dose conferred a survival benefit compared with the lower (median OS 15.7 vs 11.5 months, respectively) but was also more toxic with serious irAEs reported in 37% and 18% of patients who received ipilimumab at 10 mg/kg and 3 mg/kg, respectively. There were higher rates of severe diarrhoea (10% vs 6%), elevated liver enzymes (3% vs 1%) and hypophysitis (3% vs 2%) in patients administered ipilimumab at 10 mg/kg compared with those who received ipilimumab at 3mg/kg.35
The incidence of serious irAEs is also much higher when using combination CTLA-4/PD-1 inhibitors. In the CHECKMATE-067 trial, 59% of patients who received ipilimumab/nivolumab suffered grade 3 to 4 toxicity, compared with 21% of patients who received nivolumab alone.33
Immune-related toxicities require specific management depending on severity. Usually, this includes treatment with corticosteroids. In severe cases (grade 3 or 4), toxicities may be life threatening and patients will require hospitalisation and other immune-modulating therapies.34 The treating medical oncologist should always be involved.
Treatment decisions
Decisions regarding the choice and sequencing of treatments for advanced melanoma are complex.
BRAF mutant melanoma
Until recently, PBS requirements mandated that patients with advanced/unresectable BRAF mutant melanoma must receive targeted therapy with a BRAF/MEK inhibitor as first-line treatment. These patients were only eligible to receive immunotherapy in the event of progressive disease or intolerance to targeted therapy. However, because patients with BRAF mutant disease have a longer survival benefit with upfront immunotherapy, these restrictions were abolished in April 2020. Patients now have a choice of receiving targeted therapy or immunotherapy as first-line treatment.
The treating medical oncologist must consider patient- and disease-specific factors, including the patient’s age, comorbidities and overall burden of disease, as well as whether the treatment intent is palliation or enduring disease control. It is also crucial that treatment-specific toxicities and the effect these might have on the patient’s quality of life are considered. In addition, patient preference must always be taken into account.
BRAF wild-type melanoma
Patients with BRAF wild-type melanoma do not benefit from targeted therapy with BRAF/MEK inhibitors and treatment is therefore limited to immunotherapy. Decisions regarding whether patients should receive combination versus single-agent immunotherapy are complex and beyond the scope of this review and are best undertaken by the medical oncologist involved with managing the patient and their disease.
Conclusion
The therapeutic landscape for treating metastatic melanoma has transformed over the past decade. Cytotoxic chemotherapy is no longer used to treat advanced melanoma. Targeted therapy combinations using BRAF/MEK inhibitors for BRAF mutant melanoma and immunotherapies are highly effective treatments. These newer classes of therapies have unique toxicities that are distinct from conventional cytotoxic chemotherapy. MT
