5-fluorouracil and salicylic acid solution: a combined topical option to treat actinic keratoses

Actinic keratoses are a common issue that pose a risk for progression to squamous cell carcinoma. The surrounding sun-damaged skin is also at a heightened risk of malignant transformation and requires attention. The first topical combined solution for treating actinic keratoses in Australia, 0.5% 5-fluorouracil and 10% salicylic acid, offers an alternative treatment option that may improve efficacy and patient adherence.
- Early detection of actinic keratoses (AKs) and intervention are crucial, as AKs can progress to invasive squamous cell carcinoma, particularly if the lesions have not been adequately managed.
- The first combined topical solution to treat AKs in Australia is 0.5% 5-fluorouracil with 10% salicylic acid (5-FU/SA).
- 5-FU/SA is recommended for patients with mild to moderate AKs and is suitable for both individual lesions and field treatment. It is currently only recommended for use on the face, forehead and bald scalp. It requires adherence to a daily application regimen until the lesions have completely cleared or for a maximum of 12 weeks.
- 5-FU/SA provides a noninvasive treatment approach that may be preferred by some patients, potentially improving both adherence and therapeutic outcomes.
Actinic keratoses (AKs) are a common concern because of their potential to progress to squamous cell carcinoma (SCC). Early identification and treatment of AKs are therefore crucial to minimise this progression, making them a significant focus in skin cancer prevention strategies. AKs are highly prevalent and increase dramatically with age and accumulation of actinic damage caused by the high ultraviolet exposure in Australia. There are multiple treatment options for AKs, but balancing efficacy, patient adherence and cosmetic outcomes can be challenging.
The combination solution of 0.5% 5-fluorouracil and 10% salicylic acid (5-FU/SA) has been available internationally for over a decade. In Australia, it has seen broader availability and promotion since 2023 and provides an alternative treatment option for AK for both patients and healthcare providers. This article explores the unique position of 5-FU/SA as the first combined solution available to treat AKs in Australia, with an emphasis on its efficacy and safety. Practical guidance on its use in a clinical setting is also provided.
Definition and epidemiology of actinic keratoses
AKs, also known as solar keratoses (and colloquially as sunspots), are dysplastic epidermal lesions that result from prolonged exposure to ultraviolet radiation. They represent a spectrum of keratinocyte dysplasia, ranging from mild atypia to severe dysplasia, which may develop into invasive SCC if left untreated.1 AKs are highly prevalent in Australia, with estimates suggesting a prevalence of about 60% in adults over 40 years of age.2 However, the transformation of AK into invasive SCC is rare, with estimates ranging from 0 to 0.53% per lesion per year.3 This risk increases among individuals with high cumulative ultraviolet exposure and those with fair skin phenotypes, typically linked to red hair, freckles and a tendency to burn rather than tan.4
Clinical presentation and diagnosis
AKs typically present as solitary or multiple flat, scaly lesions on sun-exposed areas such as the face, scalp and arms. They often have an erythematous base and a rough texture but are usually nontender. Diagnosing AKs can be challenging because of their spectrum of dysplasia, which requires a thorough examination in a well-lit setting. The concept of field cancerisation is particularly relevant, as surrounding skin may harbor atypical keratinocyte changes because of chronic ultraviolet exposure that are not clinically detectable, yet pose an increased risk of malignant transformation. The use of dermoscopy and palpation may help to differentiate AKs from other lesions such as seborrhoeic keratoses or early SCC and determine if a biopsy is required. Early detection and intervention are crucial, as AKs can regress spontaneously or progress to invasive SCC, particularly if the lesions have not been adequately managed.3
5-FU/SA combination therapy
Until recently, 5% 5-FU, 4% 5-FU and cryotherapy have been commonly used as monotherapies for the management of AKs. 5-FU/SA is the first and only combination topical prescription medicine for AKs in Australia, combining the chemotherapeutic agent 5-FU with SA. In contrast with the 5-FU creams, which need to be rubbed into the skin, 5-FU/SA is produced as a solution that is applied using a brush applicator. The introduction of 5-FU/SA provides an alternative treatment option that may be preferred by some patients, potentially improving both compliance and therapeutic outcomes.5 Its availability on the Australian market brings a need for specific guidance to assist GPs in effectively integrating this treatment into clinical practice.
Composition and mechanism of action
5-FU works by inhibiting thymidylate synthase, leading to disruption of DNA and RNA synthesis, which slows the growth of rapidly proliferating atypical keratinocytes.6 SA serves as a keratolytic agent, helping to soften and exfoliate the hyperkeratotic stratum corneum, enhancing the penetration and efficacy of 5-FU in treating the underlying dysplasia.
Efficacy and safety profile
Clinical studies have demonstrated the efficacy of 5-FU/SA in treating AKs. A phase 3 multicentre clinical trial comparing daily application of 5-FU/SA with a vehicle control in a 25 cm² field-directed treatment over 12 weeks showed significantly higher complete clearance rates in the 5-FU/SA group (49.5%) compared with the control group (18.2%) eight weeks after treatment completion.7 In another double-blind randomised controlled trial, 5-FU/SA achieved a complete clinical clearance rate of 55.4% at eight weeks post-treatment, compared with 32.0% for diclofenac 3% in hyaluronic acid and 15.1% for placebo.8 Additionally, a retrospective study of 72 patients comparing 5-FU/SA with cryotherapy and CO2 laser reported similar efficacy but with less pain and better cosmetic outcomes for 5-FU/SA.9
For 4% 5-FU applied once daily, complete clearance rates varied between 24% and 80%, whereas for 5% 5-FU applied twice daily, complete clearance rates ranged from 58% to 96% at eight weeks post-treatment.10 These variations may be influenced by treatment frequency, baseline AK burden and study design, making direct comparisons challenging. A split-face study demonstrated that the 0.5% 5-FU cream was as effective as the 5% formulation in reducing AKs, while offering better tolerability.11 The once-daily application of 5-FU/SA, if better tolerated, may be more appealing to some patients compared with treatments needing a twice-daily regimen. 5-FU/SA does, however, require a longer treatment duration of up to 12 weeks compared with the three to four weeks for the twice-daily regimen of 5% 5-FU.
Although there are no head-to-head trials comparing 5-FU/SA with imiquimod, a placebo-controlled, randomised controlled trial of imiquimod reported a complete clearance rate of 45.1% at eight weeks post-treatment.12 Unlike 5-FU/SA, which works independently of the immune system, imiquimod is thought to augment both innate and acquired immune responses, which may limit its use in immunocompromised patients, but this has not been conclusively established.13
Safety and side effects
The common side effects of 5-FU/SA include erythema, inflammation and scabbing at the application site, with occasional burning and itching sensations.7-9 These side effects are generally manageable and are indicative of the treatment’s activity on the skin.
Practical guidance for GPs
Indications and use
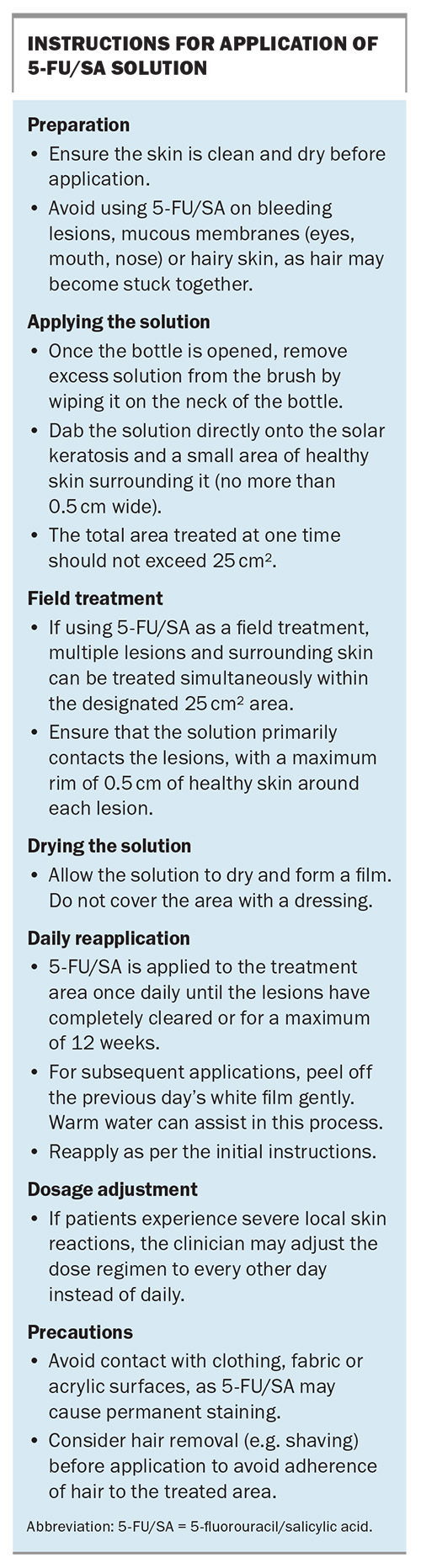
5-FU/SA is recommended for patients with mild to moderate AKs and is suitable for both individual lesions and field treatment. It is currently only recommended for use on the face, forehead and bald scalp. 5-FU/SA requires adherence to a daily application regimen. Instructions for application of 5-FU/SA are outlined in the Box.
Monitoring and follow up
Treatment response is typically indicated by local skin reactions, such as erythema and inflammation, which may be observed as early as four weeks into treatment.14 If there is difficulty tolerating side effects, the application frequency can be reduced to every other day. Complete healing and response may take up to eight weeks post-treatment.8 Patients should be monitored for changes in lesion size and appearance that may indicate progression to SCC, in which case definitive management should be initiated promptly.
Conclusion
5-FU/SA represents a valuable addition to the range of treatment options for AKs, offering a combined topical approach that may improve efficacy and patient adherence. It is suitable for patients seeking targeted and minimally invasive treatments. MT
COMPETING INTERESTS: Dr Punchihewa: None. Associate Professor Foley is on the Advisory Boards and has received honorarium from Mayne Pharma and CSL. He is also a board member for the Skin Health Institute and he is on the Medicine and Therapeutics Advisory Committee.
This article is for general information purposes only, and the full Product Information should be consulted before prescribing any of the mentioned medications.
References
1. Bakshi A, Shafi R, Nelson J, et al. The clinical course of actinic keratosis correlates with underlying molecular mechanisms. Br J Dermatol 2020; 182: 995-1002.
2. Frost CA, Green AC, Williams GM. The prevalence and determinants of solar keratoses at a subtropical latitude (Queensland, Australia). Br J Dermatol 1998; 139: 1033-1039.
3. Werner RN, Sammain A, Erdmann R, Hartmann V, Stockfleth E, Nast A. The natural history of actinic keratosis: a systematic review. Br J Dermatol 2013; 169: 502-518.
4. Memon AA, Tomenson JA, Bothwell J, Friedmann PS. Prevalence of solar damage and actinic keratosis in a Merseyside population. Br J Dermatol 2000; 142: 1154-1159.
5. Garofalo V, Geraci F, Di Prete M, et al. Early clinical response to 5-fluorouracil 0.5% and salicylic acid 10% topical solution in the treatment of actinic keratoses of the head: an observational study. J Dermatolog Treat 2022; 33: 2664-2669.
6. de Berker D, McGregor JM, Mohd Mustapa MF, Exton LS, Hughes BR. British Association of Dermatologists’ guidelines for the care of patients with actinic keratosis 2017. Br J Dermatol 2017; 176: 20-43.
7. Stockfleth E, von Kiedrowski R, Dominicus R, et al. Efficacy and safety of 5-fluorouracil 0.5%/salicylic acid 10% in the field-directed treatment of actinic keratosis: a phase iii, randomized, double-blind, vehicle-controlled trial. Dermatol Ther 2017; 7: 81-96.
8. Stockfleth E, Kerl H, Zwingers T, Willers C. Low-dose 5-fluorouracil in combination with salicylic acid as a new lesion-directed option to treat topically actinic keratoses: histological and clinical study results. Br J Dermatol 2011; 165: 1101-1108.
9. Conforti C, Giuffrida R, Dianzani C, et al. Effectiveness and tolerability of treatment for isolated actinic keratoses: a restrospective comparison between cryotherapy, CO(2) laser and 5-fluorouracil 0.5%/salicylic acid 10. Dermatol Ther 2021; 34: e14846.
10. Ezzedine K, Painchault C, Brignone M. Use of complete clearance for assessing treatment efficacy for 5-fluorouracil interventions in actinic keratoses: how baseline lesion count can impact this outcome. J Mark Access Health Policy 2020; 8: 1829884.
11. Loven K, Stein L, Furst K, Levy S. Evaluation of the efficacy and tolerability of 0.5% fluorouracil cream and 5% fluorouracil cream applied to each side of the face in patients with actinic keratosis. Clin Ther 2002; 24: 990-1000.
12. Lebwohl M, Dinehart S, Whiting D, et al. Imiquimod 5% cream for the treatment of actinic keratosis: results from two phase III, randomized, double-blind, parallel group, vehicle-controlled trials. J Am Acad Dermatol 2004; 50: 714-721.
13. Bilu D, Sauder DN. Imiquimod: modes of action. Br J Dermatol 2003; 149 Suppl 66: 5-8.
14. Mayne Pharma International Pty Ltd. Actikerall Solution. Consumer Medicine Information. March 2023. Available online at: https://www.maynepharma.com/au-products/actikerall-solution/ (accessed December 2024).