Cosmetic laser and light therapies
Patients often consult GPs about aesthetic concerns, but cosmetic medicine, including laser therapy, is rarely taught in medical school. Lasers can be used for treating common cosmetic problems by emitting energy of an appropriate wavelength to be absorbed by a specific target or chromophore in the skin. As laser and laser-like devices for cosmetic purposes do not require TGA approval, clinicians should critically evaluate the safety and efficacy of any intervention before recommending it to patients.
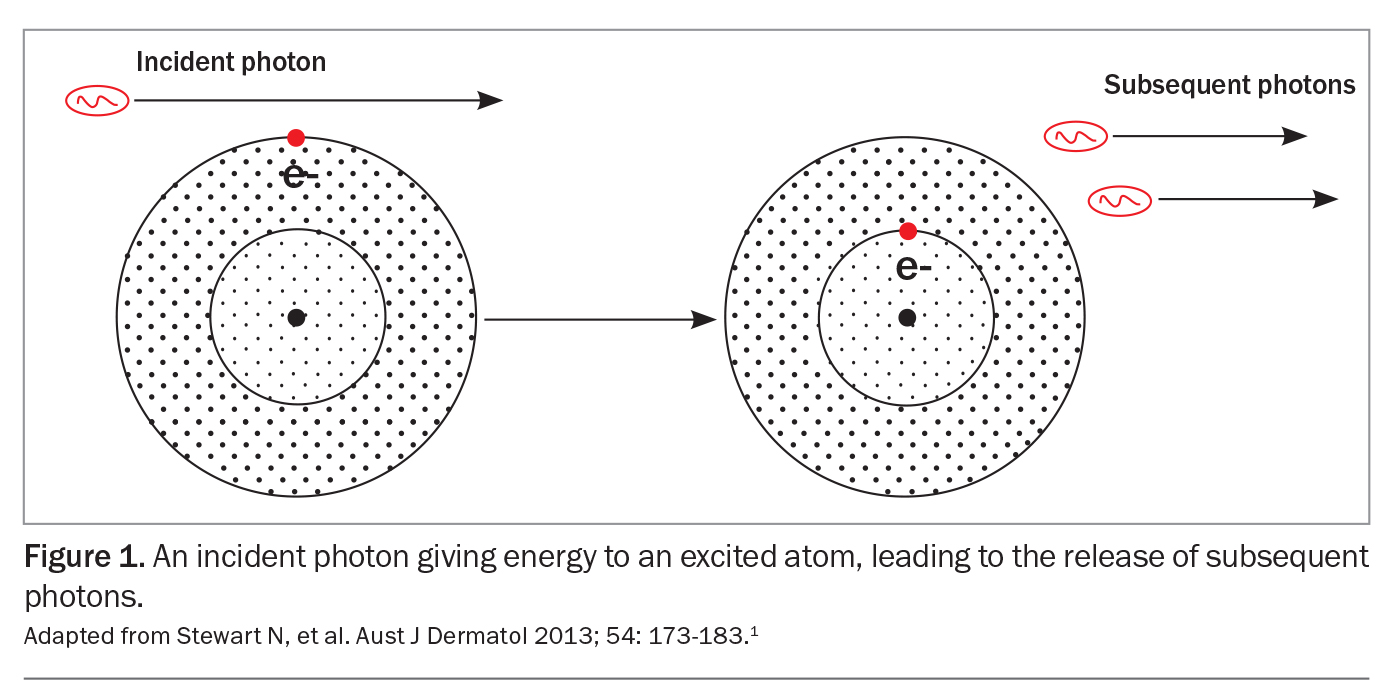
Laser (light amplification by stimulated emission of radiation) can be used in dermatology for its photothermal and photoacoustic properties. Laser energy depends on the principle of exponential light amplification through stimulated emission of photons. Each type of laser has a specific gain medium that gives it unique characteristics. An external power source excites the gain medium, leading to electron movement between the orbital shells of the affected atom and subsequent release of the energy in the form of photons (Figure 1).1 These photons will energise other atoms, triggering rapid multiplication of photons and exponential light amplification.1 The photons are amplified by mirrors within the device until they are released by the operator.
Laser beams were originally released as continuous streams of energy, but they are now pulsed (repetitive ‘on-off’ delivery) for better safety and control. Developments in technology have permitted laser pulse durations of picoseconds, which can also enact damage through photoacoustic energy.2
Chromophores, such as melanin and haemoglobin, are biochemical entities that absorb light at specific frequencies. The radiation produced by laser or light therapy can be manipulated to selectively target and destroy specific chromophores, while sparing the surrounding tissue. It is important that the irradiated area is able to dissipate heat, to reduce collateral damage to surrounding tissue and subsequent adverse outcomes.1 Both haemoglobin and melanin largely absorb light energy at wavelengths below 620 nm.3 Lasers of wavelengths above 1200 nm predominantly target water in the epidermis and superficial dermis.3
This article gives an overview of laser and light-based modalities for treating common cosmetic problems. Broad categories of laser and light devices include intense pulsed light (IPL), vascular lasers, pigment lasers and ablative and nonablative lasers. When selecting a laser for cosmetic indications, consideration must be given to the patient’s skin characteristics, treatment goals and the appropriate laser parameters.
Laser types and indications
Intense pulsed light
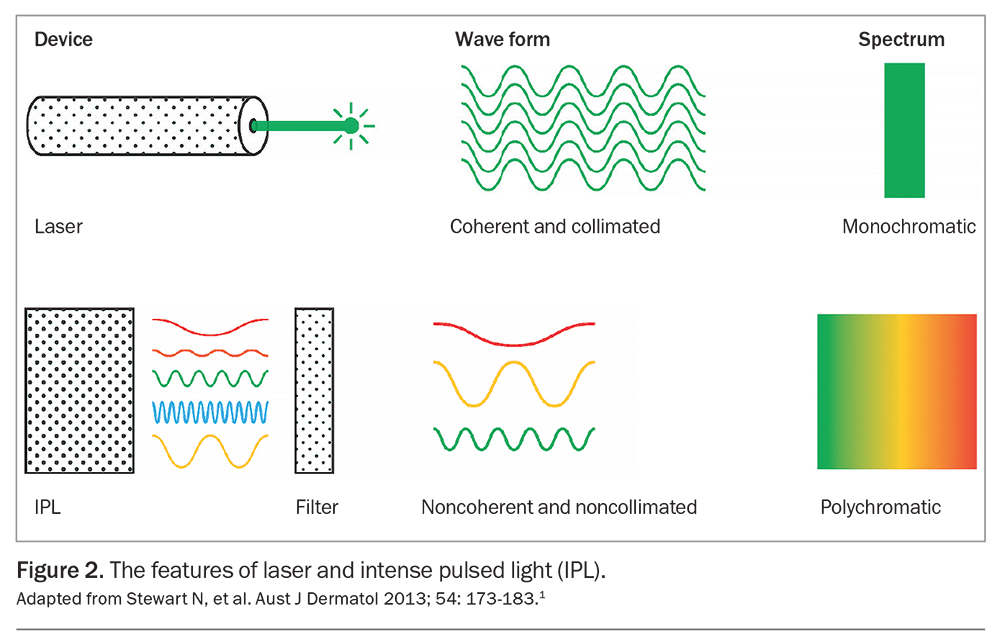
Although commonly referred to as a laser, IPL is a filtered flash lamp device that comes under the broader category of light therapies. It emits noncoherent polychromatic radiation with wavelengths between 420 and 1300 nm (Figure 2).1
IPL can be used for treating vascular lesions, dyschromia and lentigines, as well as for hair removal.1,4 Evidence suggests it may also be helpful in skin rejuvenation through alteration in gene expression, although it is not known how durable the response is over time.5
Vascular lasers
Vascular lasers target haemoglobin (oxyhaemoglobin) and can be used to treat rosacea, facial telangiectasia, angiomas, spider naevi, angiokeratomas, infantile haemangioma and other vascular anomalies (Figures 3a and b).1,4,6 Device settings should be directed by the size and depth of the target vessel.
Both pulsed dye lasers and potassium-titanyl-phosphate lasers have wavelengths (585 to 595 nm and 532 nm, respectively) that correspond well with the absorption peak of oxyhaemoglobin and are effective in treating capillary and vascular lesions.7 Neodymium-doped yttrium-aluminium-garnet (Nd:YAG) lasers have a longer wavelength of 1064 nm, which better targets larger-calibre blood vessels and venules because it has deeper penetration into the dermis.1
Pigment lasers
Lasers of various wavelengths (including 532 nm, 694 nm, 755 nm and 1064 nm), as well as nonlaser devices like IPL, can be used to treat pigmentary disorders, as melanin preferentially absorbs wavelengths below 1000 nm and does not have an absorptive peak.1 Pigment lasers can be used to treat brown freckles (lentigines and ephelides) and pigment birthmarks (café-au-lait macules, naevus of Ota and congenital dermal melanocytosis [formerly known as Mongolian spots]) and for hair and tattoo removal.1,4 Although melasma is a common pigmentary disorder, laser treatments are variably and unpredictably efficacious for this condition.8,9 Patients treated with pigment lasers for melasma can experience recurrence soon after treatment, as well as undesirable postinflammatory hyperpigmentation.8,9
Patients with darker skin are at higher risk of adverse effects, and long-wavelength lasers are recommended to reduce superficial uptake of laser energy and risk of dyspigmentation in this group.4,10 Laser therapy is not recommended for treating melanocytic naevi as it may mask the development of malignant melanoma; surgery remains the gold-standard treatment for this.4,11
Hair removal
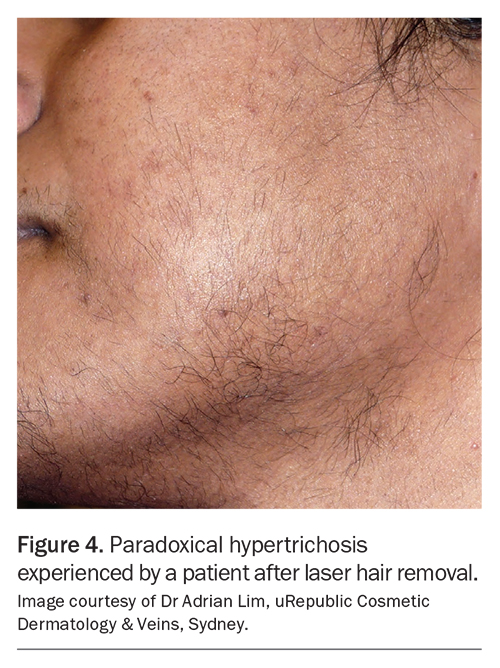
Laser therapy can be used to selectively target melanin within germinative cells in the hair follicle, leading to swelling, apoptosis and necrosis of the follicle cells from laser-induced thermal injury.12 This causes permanent stable hair reduction over several sessions.13 Various lasers can be used for this purpose, including 810 nm diode, 755 nm alexandrite and 1064 nm Nd:YAG lasers, with the latter preferred for people with pigmented skin because of its longer wavelength.4 As melanin pigment is the fundamental chromophore, pigmentary side effects are more common in people with darker skin types, and white hair without melanin pigment will not be laser-responsive. Paradoxical hypertrichosis (where the hair regrows thicker and denser) is an uncommon but often distressing reaction after laser hair removal (Figure 4). However, continued therapy may lead to eventual reduction in hair growth.12
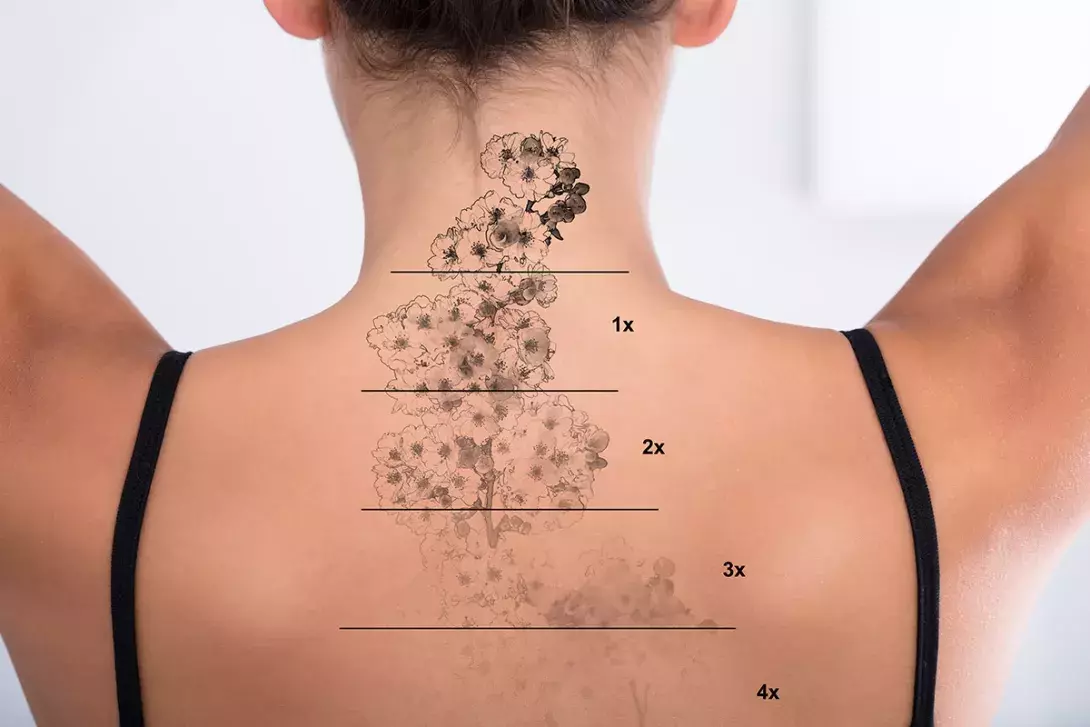
Tattoo removal
Professional tattoos are created by deposition of exogenous (nonmelanin) pigment into the dermis. To remove tattoos, rapid pulses of laser energy, generated by nanosecond or picosecond devices (with wavelengths of 694 nm, 755 nm or 1064 nm), are required to shatter the tattoo pigment with photoacoustic (rather than thermal) effects.14 These devices progressively clear tattoo ink by photoacoustic shattering of tattoo granules into increasingly smaller fragments to permit clearance via the macrophage-lymphatic system.4,14
It is recommended to familiarise the patient with the tattoo removal process by performing it on a test patch. Patients also need to be advised that multiple sessions (from five to 20) are likely to be needed, with black tattoos being far more responsive to removal than coloured tattoos.4
Ablative resurfacing lasers
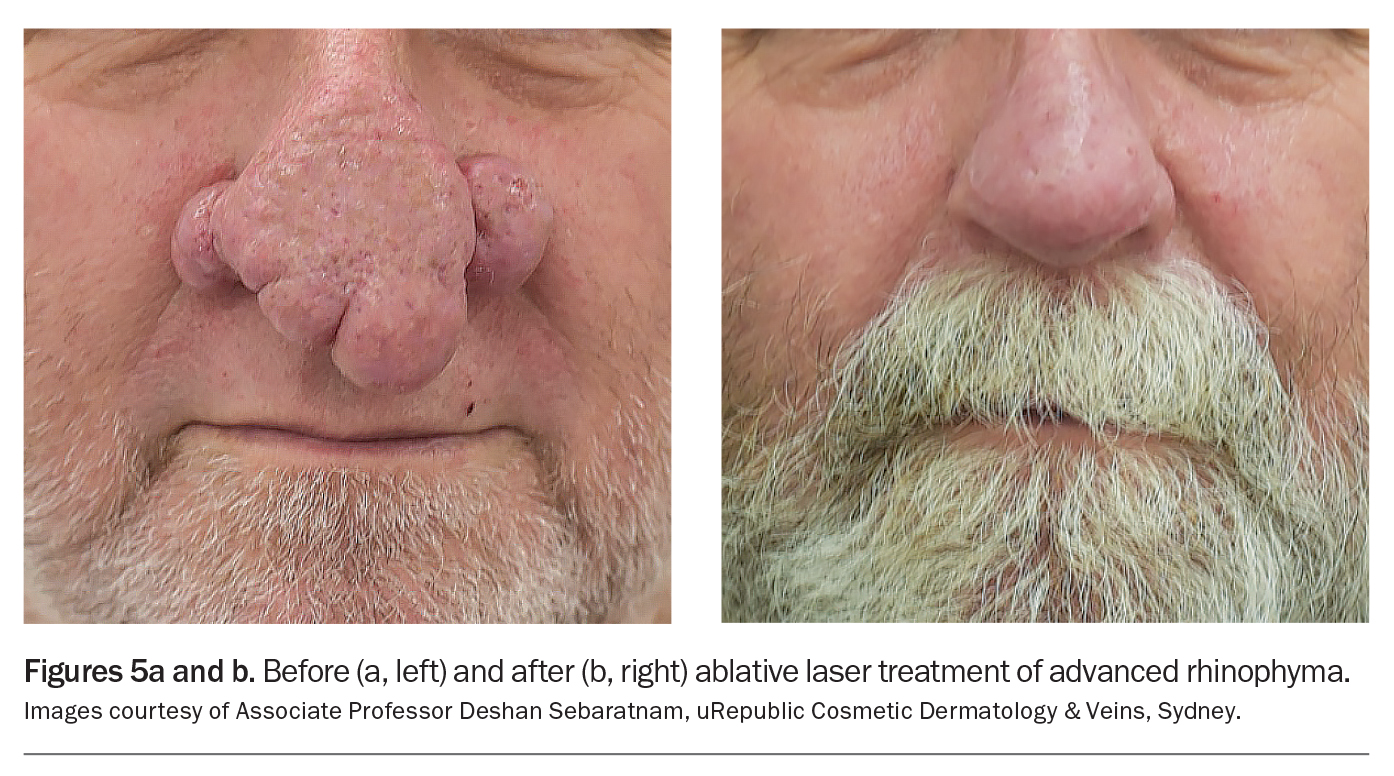
Ablative lasers produce rejuvenating effects by using thermal energy to vaporise water within skin cells, leading to healing and remodelling of denatured proteins.15 These devices include carbon dioxide (CO2) lasers, which have a wavelength of 10,600 nm, and erbium-doped yttrium-aluminium-garnet (Er:YAG) lasers, which have a wavelength of 2940 nm. Although extremely effective, CO2 lasers involve a longer healing period and have a higher risk profile, including risk of dyspigmentation, particularly in darker-skinned people.4 Er:YAG lasers, in contrast, are absorbed by water 10- to 16-fold more than CO2 lasers and produce superficial ablation with less thermal injury.1 Ablative lasers are used in treating rhytides (facial lines and wrinkles), scars, rhinophyma and exophytic lesions, such as seborrheic keratosis, epidermal naevi and dermatosis papulosa nigra (Figures 5a and b).4
Fractionated lasers
Fractionated lasers are an adapted form of ablative lasers. They deliver thermal injury in multiple discrete vertical cylinders, or microchannels, leaving spared islands of intervening tissue. As these reservoirs are spared from thermal damage, they offer nutritional support to the cells and can act as structural support for keratinocytes and fibroblast migration.1 Fractionated lasers can be ablative (tissue vaporising) or nonablative (tissue coagulating). They can be used to treat photodamaged skin, mild rhytides and acne scarring. Patients favour fractionated lasers, as they have less propensity for causing prolonged erythema and dyspigmentation. They also require less downtime (three to seven days), compared with traditional nonfractionated lasers. However, multiple treatments may be required.4
Treating scars and skin texture problems
Scarring and skin textural changes are responsive to ablative and fractionated laser resurfacing. Not all scars are the same, and treatment is determined by scar type, morphology and severity. For acne scarring, algorithms describing different therapeutic interventions depending on scar subtype have been published, but fractionated lasers are the mainstay of therapy.4 A common misconception is that patients must wait six months after isotretinoin treatment to receive laser therapy. However, the consensus is that most lasers can be safely used as soon as acne is controlled (including fractionated lasers and excepting fully ablative lasers).16 It should be emphasised that no scarring will be completely removed with any procedural therapy, and progress is typically modest and incremental in gain.
Multimodal treatment
Using one treatment modality at a time is recommended for new practitioners. With experience, clinicians can begin to combine laser therapy with other cosmetic treatments, including fractional radiofrequency, muscle relaxants or fillers.4 IPL is often combined with pulsed dye vascular laser therapy for patients with a mix of lentiginous change and erythema. Similarly, for patients with rhinophyma, CO2 laser therapy is often used in combination with Er:YAG laser therapy and electrodessication. Topical sirolimus is being increasingly used in combination with vascular laser therapy for patients with capillary malformations.17
Risks of laser therapy
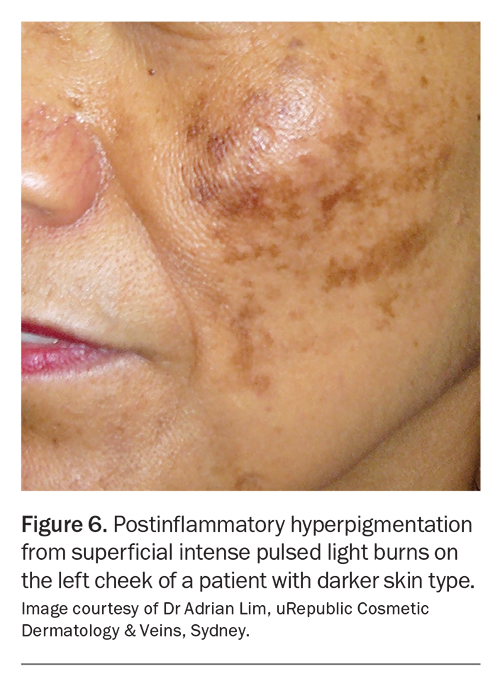
Downtime is to be expected from most laser procedures, especially with resurfacing lasers, as components of the skin are intentionally damaged and require time to regenerate. It is important to inform people with darker skin, especially those with a Fitzpatrick skin type of IV to VI, that they have much higher risks of burns, dyspigmentation (postinflammatory hyperpigmentation),
textural changes and scarring (Figure 6). The higher quantities of melanin in darker skin mean that a greater proportion of energy is absorbed by the constitutional background melanin. As a consequence, lower amounts of residual energy reach the target tissue, which increases the risk of burns and reduces therapeutic efficacy.4 There is also an increased basal melanocytic activity that predisposes darker-skinned people to postinflammatory hyperpigmentation. To reduce these risks, use of laser platforms with longer wavelengths and conservative power settings is recommended, with an emphasis on cooling devices to counteract the total accumulated heat energy.1
Adverse effects and management
Common transient side effects should be explained to the patient before the procedure. These include:4
- pain
- pruritus
- erythema
- purpura
- mild oedema
- acne
- vesiculation
- crusting
- temporary pigment changes.
They may occur with more aggressive treatment protocols but can be expected to fully resolve. More serious adverse effects include thermal burns, scarring, dyspigmentation (hypopigmentation and hyperpigmentation) and ocular damage.4,18
As with any medical consultation, a full medical history is required. For example, certain pigment lasers are contraindicated for patients who have taken gold (e.g. for arthritis), and a history of herpes simplex mandates antiviral prophylaxis for patients receiving ablative laser therapy.18 It is pertinent to establish if the patient has a history of previous skin-coloured or black-ink tattoos, as the pigments used can interact with the laser therapy and result in paradoxical darkening or burns, respectively.19,20 Any previous scar camouflage tattoo or tattoo pigment can act competitively and cause uneven distribution of light and pigmentation.4 Improper postprocedural care also increases the risk of bacterial and viral infections.
Eye protection is always needed to protect the patient from direct and reflective laser or light impact.10 Ocular complications from laser or light therapy include permanent vision impairment, iris atrophy, cataracts, anterior uveitis, glaucoma, posterior synechiae and pupillary defects.21 The most common causes of eye injury are improper eye protection or clinicians removing the patient’s eyewear to treat areas near the eye.10,21
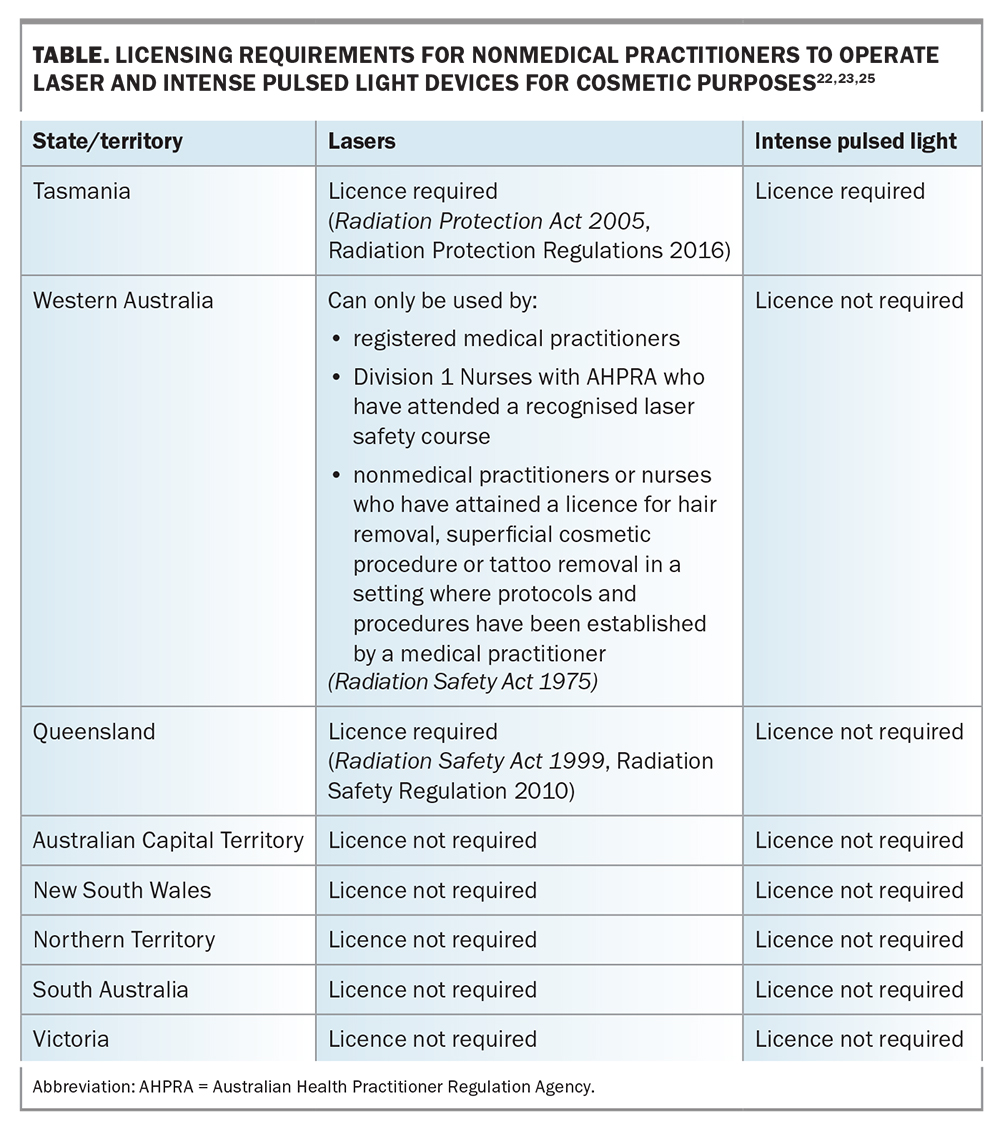
Regulations in the laser industry
Advances in technology and lower production costs have led to a proliferation of light-based therapies. There is often limited evidence-based information on new devices, as they do not need to be approved or supervised by the TGA.22 The limited regulations and safety precautions in the cosmetic industry can also result in misleading, erroneous or unsubstantiated information.23 Training on device application is usually provided by the manufacturers, with obvious conflicts of interest.
There are no national guidelines to dictate training, accreditation or certification in laser use, and the field of cosmetic medicine remains largely unregulated.23,24 Requirements are mandated by individual state or territory legislation (Table). In certain states, anyone who can acquire a laser or light device can start practising. As devices can be easily purchased through the internet, there may be operators practising without the assurance of adequate training and regulation.22 In 2021, the Australian Health Practitioner Regulation Agency and Medical Board of Australia announced a review of patient safety in the cosmetic sector, in response to serious complications caused by registered health practitioners.26
General approach
Complications are inevitable with laser therapy, even for experienced physicians. Idiosyncratic patient-specific response is difficult to predict and should be explained to the patient as part of informed consent for the proposed procedure.18 Nevertheless, risk minimisation strategies should always be adopted, and there should be a clear management pathway to deal with common and uncommon adverse events. If a lesion is suspicious for an underlying medical condition, it is important not to conduct any laser treatment, as this can aggravate or disguise the underlying condition. Further investigation or referral to a specialist should be considered.
A suggested approach to laser therapy is as follows:
- Conduct appropriate patient screening:10
– correct diagnosis of lesion (if there is uncertainty about the diagnosis, the lesion should not be treated)
– Fitzpatrick skin phototype
– medical conditions (e.g. lupus, koebnerising skin conditions such as vitiligo or psoriasis, herpes simplex, keloid scars)
– previous cosmetic or surgical procedures, including fillers, tattoos, radiotherapy and skin grafts
– allergies
– recent/regular/planned sun exposure or recent sunburn
– full medication history (including photosensitising medications or supplements)
– pregnancy and breastfeeding status for women of childbearing age
– application of fake tan within the previous two weeks
– waxing, epilation or use of hair removal creams within the previous two months. - Explain the proposed procedure and ensure the patient has realistic expectations
- Take preprocedural photographs
- For some treatments, conduct patch testing on a small area of skin at least 48 hours before the procedure to reduce the chance of adverse reactions (some clinicians may prefer to patch test as early as six weeks beforehand to ensure efficacy of the intended treatment)
- Make appropriate selection of laser or light device and settings:
– follow treatment guidelines
– ensure selection of appropriate treatment parameters, including laser wavelength and mode; do not target unnecessary tissue. - Follow treatment protocol:
– inform patients of expected side effects, recovery time, costs, likely number of treatments and duration of intervals between sessions
– ensure skin is clean and dry (patients should be advised not to apply any cosmetic products to the treatment area for 12 hours before the procedure)
– ensure adequate cooling, especially for patients with darker skin. - Take postprocedural photographs and provide postprocedural care:
– give the patient written information about aftercare, including the importance of hygiene to prevent infection and any products that should be avoided
– discuss symptoms or signs that warrant medical review and how that should be arranged
– organise follow up to assess the patient’s progress
– explain to the patient that patient-specific response is an uncontrollable variable that can lead to complications, but optimal care will be offered.
When should a GP refer?
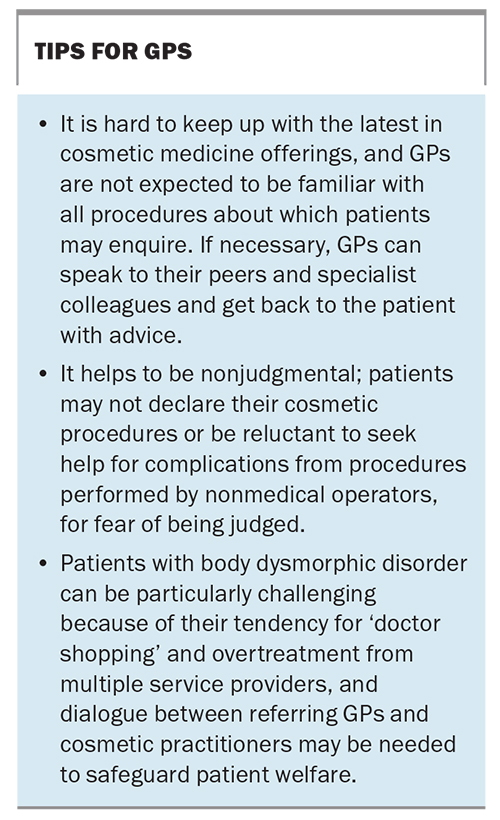
GPs should refer a patient to a dermatologist before laser therapy when there is doubt about the diagnosis of a skin lesion. There are many causes of facial erythema beyond rosacea and photodamage, and pigmented lesions must have a clinical diagnosis before treatment. Different cosmetic dermatoses may require use of different lasers, and undue harm can result if the lesion is incorrectly treated. A 2012 Radiation Health Committee survey found that 62 cases of skin cancer were missed or delayed in a 12-month period in Australia because of incorrect treatment with laser or IPL therapy, leading to unnecessary morbidity.22
GPs should also refer patients with significant complications arising from laser therapy for specialist management. Cosmetic GPs should refer patients if they do not have the right modality to treat a particular condition.23 Practice tips for GPs are provided in the Box.
Conclusion
When used appropriately, modern laser technology is a valuable therapeutic option that can target and treat a wide range of cosmetic dermatoses. Procedures are generally effective and safe when patients are suitably selected and when the appropriate laser is used for the correct indication by a properly trained operator. As laser and light devices for cosmetic purposes do not need TGA approval, clinicians should critically evaluate the safety and efficacy of these devices before recommending their use to patients. MT
COMPETING INTERESTS: Dr Sebaratnam has received consulting fees from Galderma, AbbVie, Pfizer, Novartis, Janssen, LEO Pharma, Ego Pharmaceuticals and Sun Pharmaceutical Industries; a scholarship from Eli Lilly; and material support from Candela Medical. Dr Wong, Dr Lowe: None.
References
1. Stewart N, Lim AC, Lowe PM, Goodman G. Lasers and laser‐like devices: Part one. Aust J Dermatol 2013; 54: 173-183.
2. Torbeck RL, Schilling L, Khorasani H, Dover JS, Arndt KA, Saedi N. Evolution of the picosecond laser: a review of literature. Dermatol Surg 2019; 45: 183-194.
3. Sakamoto FH, Wall T, Avram MM, Anderson RR. Lasers and flashlamps in dermatology. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, eds. Fitzpatrick’s dermatology in general medicine. Volume II. 7th ed. New York: McGraw Hill; 2008. p. 2263-2279.
4. Sebaratnam DF, Lim AC, Lowe PM, Goodman GJ, Bekhor P, Richards S. Lasers and laser‐like devices: Part two. Aust J Dermatol 2014; 55: 1-14.
5. Chang ALS, Bitter Jr PH, Qu K, Lin M, Rapicavoli NA, Chang HY. Rejuvenation of gene expression pattern of aged human skin by broadband light treatment: a pilot study. J Invest Dermatol 2013; 133: 394-402.
6. Sebaratnam DF, Wong L-CF, Wargon O. Infantile hemangioma. Part 2: management. J Am Acad Dermatol 2021; 85: 1395-1404.
7. Nelson JS, Jia W, Phung TL, Mihm Jr MC. Observations on enhanced port wine stain blanching induced by combined pulsed dye laser and rapamycin administration. Lasers Surg Med 2011; 43: 939.
8. Rendon M, Berneburg M, Arellano I, Picardo M. Treatment of melasma. J Am Acad Dermatol 2006; 54 (5 Suppl 2): S272-S281.
9. Gupta AK, Gover MD, Nouri K, Taylor S. The treatment of melasma: a review of clinical trials. J Am Acad Dermatol 2006; 55: 1048-1065.
10. Advice for providers: Lasers, IPL devices and LED phototherapy for cosmetic treatments and beauty therapy. Melbourne: Australian Radiation Protection and Nuclear Safety Agency; 2019. Available online at: https://www.arpansa.gov.au/understanding-radiation/sources-radiation/more-radiation-sources/lasers-and-intense-pulsed-light-1 (accessed April 2023).
11. Ibrahimi OA, Alikhan A, Eisen DB. Congenital melanocytic nevi: Where are we now? Part II. Treatment options and approach to treatment. J Am Acad Dermatol 2012; 67: 515.e1-e13.
12. Gan SD, Graber EM. Laser hair removal: a review. Dermatol Surg 2013; 39: 823-838.
13. Haedersdal M, Gøtzsche PC. Laser and photoepilation for unwanted hair growth. Cochrane Database Syst Rev 2006; (4): CD004684.
14. Naga LI, Alster TS. Laser tattoo removal: an update. J Am Acad Dermatol 2017; 18: 59-65.
15. Verma N, Yumeen S, Raggio BS. Ablative laser resurfacing. StatPearls; 2023. https://www.statpearls.com/point-of-care/32713 (accessed April 2023).
16. Spring LK, Krakowski AC, Alam M, et al. Isotretinoin and timing of procedural interventions: a systematic review with consensus recommendations. JAMA Dermatol 2017; 53: 802-809.
17. Marqués L, Núñez-Córdoba JM, Aguado L, et al. Topical rapamycin combined with pulsed dye laser in the treatment of capillary vascular malformations in Sturge-Weber syndrome: phase II, randomized, double-blind, intraindividual placebo-controlled clinical trial. J Am Acad Dermatol 2015; 72: 151-158.e1.
18. Kalashnikova NG, Jafferany M, Lotti T. Management and prevention of laser complications in aesthetic medicine: an analysis of the etiological factors. Dermatol Ther 2021; 34: e14373.
19. Finlayson HW, Kim WA, Dheansa B. Case report: Full thickness burns from intense pulsed light hair removal. Burns Open 2023; 7(2): 26-27.
20. Riml S, Larcher L, Grohmann M, Kompatscher P. Second‐degree burn within a tattoo after intense‐pulsed‐light epilation. Photodermatol Photoimmunol Photomed 2013; 29: 218-220.
21. Huang A, Phillips A, Adar T, Hui A. Ocular injury in cosmetic laser treatments of the face. J Clin Aesthet Dermatol 2018; 11(2): 15.
22. Australian Radiation Protection and Nuclear Safety Agency. Regulatory impact statement: intense pulsed light sources (IPLs) and lasers for cosmetic or beauty therapy. Sydney: ARPANSA; 2015.
23. Leow LJ. Navigating the disparate Australian regulatory minefield of cosmetic therapy. Aust Fam Physician 2017; 46: 697-698.
24. Lasers, IPL and LED devices for cosmetic treatments and beauty therapy. Melbourne: Victorian Department of Health; 2021. Available online at: https://www.health.vic.gov.au/radiation/lasers-ipl-and-led-devices-for-cosmetic-treatments-and-beauty-therapy (accessed April 2023).
25. Radiological Council. Fact sheet for cosmetic use of lasers. Perth: Government of Western Australia; 2021.
26. Ahpra and Medical Board announce review of cosmetic surgery checks and balances. Melbourne: Australian Health Practitioner Regulation Agency; 2021. Available online at: https://www.ahpra.gov.au/News/2021-11-24-cosmetic-review.aspx (accessed April 2023).