Mandatory salt targets a likely cost-effective strategy in CVD and CKD prevention
By Rebecca Jenkins
Mandating reduced sodium levels for packaged foods in Australia is a likely cost-effective strategy to prevent thousands of deaths and incident cardiovascular disease (CVD) and chronic kidney disease (CKD) events, a modelling study finds.
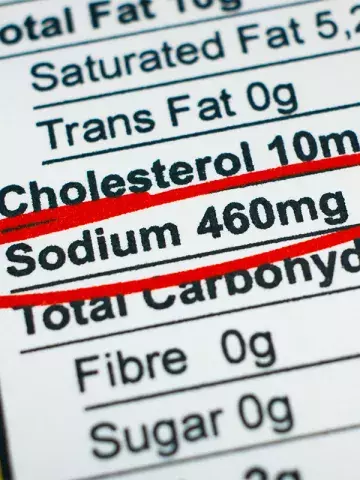
Excess sodium consumption is a leading dietary risk factor for premature deaths worldwide, an Australian-led international research team wrote in The Lancet Public Health, and in most high-income countries 70 to 90% of dietary sodium comes from processed and packaged foods.
WHO recommends consuming less than 2000 mg of sodium daily, they added, yet currently the global mean sodium intake is 4310 mg per day.
Using a multiple cohort, life table model, researchers simulated the long term economic and health outcomes of Australia mandating either the current voluntary Australian Healthy Food Partnership (HFP) sodium targets or the WHO global sodium benchmarks, which cover more products and have lower targets than the HFP.
The study found that under mandatory HFP and WHO targets, 2522 and 7756 packaged foods would be subject to reformulation, respectively.
Compared with full compliance with mandatory HFP targets, full compliance with the WHO sodium benchmarks was estimated to translate into a 3.0 to 4.2 times greater sodium intake reduction.
Mandating the WHO global sodium benchmarks could be cost-saving over the first 10 years (AUD$223 million in saving), the model found, with 2914 CVD and CKD deaths and 43,971 incident CVD events and 32,439 new CKD cases potentially averted.
The strategy would be highly cost effective over the population’s lifetime, the researchers said, noting that overall 69,117 CVD and CKD deaths and 284,236 incident CVD events and 246,725 new CKD cases could be averted.
Mandating the HFP sodium targets could also be cost effective over the population’s lifetime, the researchers reported, but the less stringent targets would result in 29% of the health benefits compared with the WHO benchmarks.
Lead author, Dr Matti Marklund, Senior Research Fellow at The George Institute for Global Health, Australia, and Assistant Professor at Johns Hopkins Bloomberg School of Public Health, Baltimore, USA, said although previous studies had estimated the potential impacts of mandating sodium levels on intake and disease burden, this was the first study to quantify both the long-term health outcomes and economic impact of mandating sodium limits in Australia.
‘Mandating these currently voluntary limits could save many lives, with healthcare cost savings from preventing heart attacks, strokes and kidney disease far outweighing the costs of implementing and enforcing mandatory sodium limits,’ he told Medicine Today.
‘However, if Australia adopted the WHO’s more comprehensive and stringent sodium benchmarks, the health benefits could be threefold.’
Dr Marklund added that Australia’s voluntary sodium targets were relatively lenient, and the targets specified only a limited number of food categories. As they were voluntary, there was also little incentive for manufacturers to meet them.
‘This weak regulatory approach means Australia is missing a valuable opportunity to shield its population from the health risks associated with excessive sodium intake,’ he said.