Preventing and managing UTIs: many gaps remain in evidence base
By Rebecca Jenkins
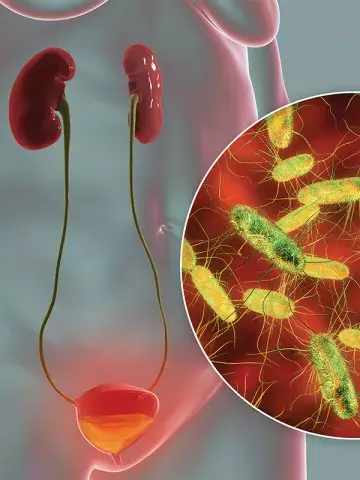
An international expert group has made a series of recommendations for preventing, diagnosing and managing urinary tract infections (UTIs) in children and adults, but its research has also revealed many pressing gaps in the evidence base.
In the WikiGuidelines Group consensus statement, published in JAMA Network Open, 54 experts from 12 countries wrote that UTIs were among the most common infections globally, notably impacting patient quality of life and posing substantial clinical and economic challenges.
The group reviewed 914 articles and submitted evidence relevant to 37 clinical questions covering five areas: prophylaxis and prevention, diagnosis and diagnostic stewardship, empirical treatment, definitive treatment and antimicrobial stewardship, and special populations and genitourinary syndromes.
However, they could only provide a clear recommendation for six of the questions and for certain aspects of a further three questions and instead provided clinical reviews in areas where strong evidence was lacking.
‘Pressing research gaps remain, including the need for high quality studies to validate novel diagnostic methods, optimize treatment durations, establish standard definitions, and refine antimicrobial stewardship strategies for asymptomatic bacteriuria and [multidrug resistant organisms],’ they wrote.
Coauthor Professor Steven Tong, Infectious Diseases Physician with the Victorian Infectious Diseases Service and lead of Clinical and Health Systems Research at the Doherty Institute, University of Melbourne, said UTI prevention had been reasonably well studied.
There was sufficient evidence to make clear recommendations that cranberry products, vaginal oestrogen and methenamine hippurate were effective for certain population groups, he said.
‘In particular, topical oestrogen has consistently been found to be effective at reducing recurrent UTIs in postmenopausal women,’ he told Medicine Today.
Professor Tong said the group also provided clear recommendations for which antibiotics could be used for UTIs and their suggested duration of treatment, adding that the exact choice depended on local antibiotic resistance patterns and individual patient factors.
For patients with uncomplicated cystitis, nitrofurantoin was found to be a reasonable drug of choice, while for patients with pyelonephritis, trimethoprim/sulfamethoxazole or a first generation cephalosporin represented reasonable first-line agents.
‘In general, for uncomplicated UTIs short durations of treatment are sufficient,’ he said.
Given the evidence gaps for managing and treating UTIs, Professor Tong said there was a lot to be said for using common sense and having open discussions with patients.
‘Where there is a lack of strong evidence, we should be honest about this but still provide practical guidance,’ he said.
‘We don’t need to be dogmatic about a certain management course, but instead try to find something that works and limits costs and impositions on our patients and healthcare system.’
However, he said more pragmatic clinical trials should be conducted, addressing everyday clinical questions around managing UTIs.
‘New drugs do need to be developed and trialled, but we also need to work out simple questions such as whether drinking more water helps to prevent UTIs,’ he said.