Depression: recognising the signs in older people and in dementia

Depression often presents differently in older people compared with younger populations, and in the setting of dementia, differences can be even greater, making diagnosis challenging. Treatment of depression in older people is similar to that of any patient, albeit with particular consideration of the effects of medications on age-specific factors, such as falls risk, balance, confusional states and orthostatic hypotension.
- Presentations of depression differ in older people, often appearing as prominent lethargy or hypochondriacal concerns, insomnia, anxiety, nervousness and irritability.
- Older people are less likely to self-identify as having a depressed or low mood.
- The presence of symptoms, including sleep and appetite changes, decreased psychomotor activity, poor concentration, indecision and fatigue, are more likely to be seen as part of a major depression in older people.
- An older person presenting with a change in mood with no obvious precipitant should be assessed for a cognitive diagnosis.
- Treatment for older people with depression is similar to that for any patient, and medication selection should be based on the patient’s symptoms and drug factors.
- Measurable and observable traits, such as changes in sleep and appetite, can help in diagnosing depression in older people with dementia.
Depression is a major source of health burden globally, with the lifetime risk of major depression exceeding 30%.1,2 The risk of depression rises with age. However, this is not because of ageing itself; rather, it is the result of risk factors associated with depression that become more prevalent with age.3 Such risk factors include chronic pain, chronic illness, polypharmacy, stigma, bereavement, social isolation and loneliness, disability, cognitive impairment, economic deprivation, loss of role and abuse of any kind. Once these factors are controlled for, the excess of depressive diagnoses in old age disappear.
Depressive disorders run the spectrum, from the classic major depressive disorder (MDD) through to persistent depressive disorder (PDD; previously known as dysthymic disorder). The presence of depressive symptoms that fall short of meeting diagnostic criteria for a disorder but still cause significant distress and impairment is also common.
The prevalence of depression in old age
The prevalence of depression in old age depends largely on the population. Community surveys using validated diagnostic instruments suggest that the prevalence of MDD in community- dwelling older people is about 3% and the prevalence of any depressive disorder is as high as 10%. In similar diagnostic surveys of older people attending general practice, the prevalence of MDD rises to 10% and that of any depressive disorder to 30%. In older general medical inpatient populations, the prevalence of MDD and any depressive disorder increases again to 30% and 50%, respectively.4 High-quality data on the prevalence in nursing homes are lacking, but more than 50% of residents may meet diagnostic criteria for MDD at any one time.5 The rates of MDD in elderly carers are similarly high.6
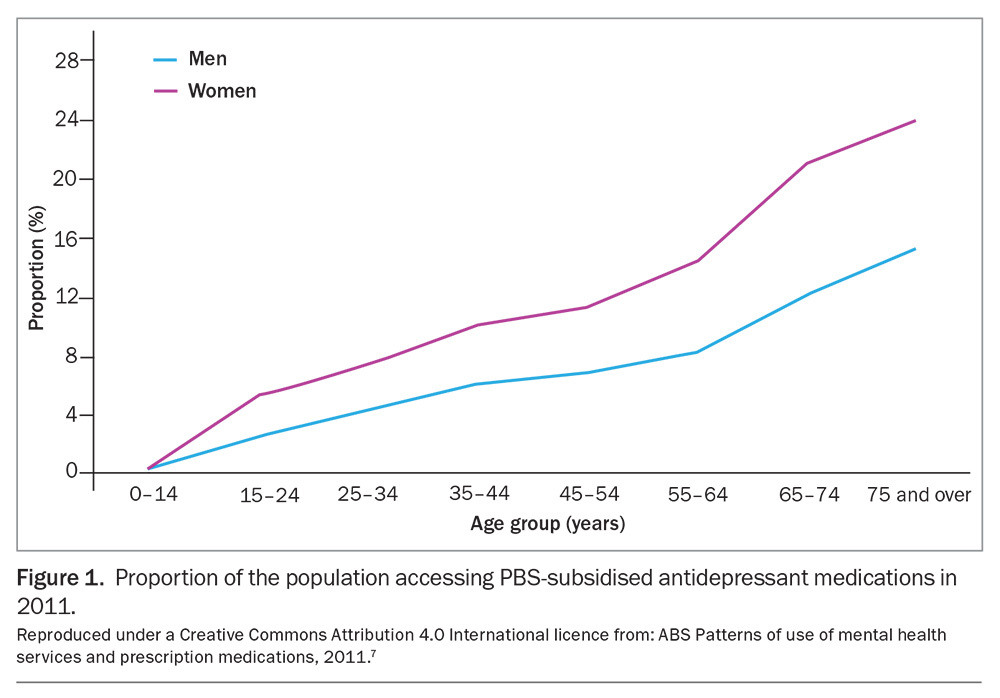
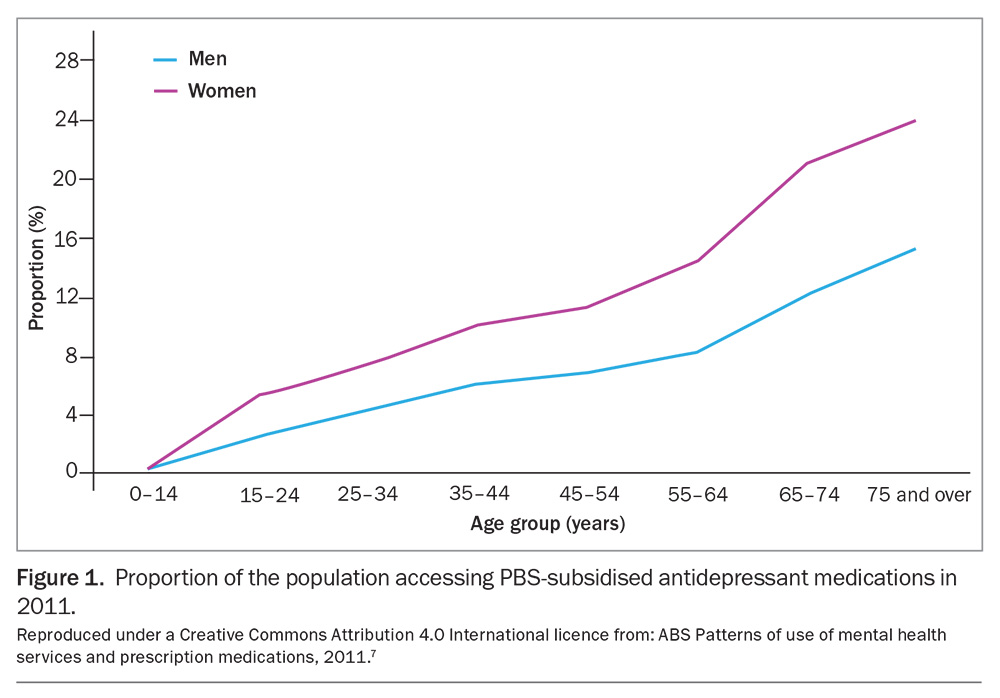
In light of these data, clinicians should reflect on the rates of diagnosed depression in the populations seen in clinical practice. In 2011, 24% of women and 15% of men over the age of 75 years received at least one prescription for an antidepressant each year (Figure 1).7 However, not all antidepressants prescribed in older people are for the treatment of depression, with data suggesting that tricyclic antidepressants comprised 35% of antidepressants prescribed in older people, often at subtherapeutic doses and for issues unrelated to mood, including nocte sedation, chronic pain and incontinence.8 Such statistics suggest that, despite the high prevalence of depression in older people, making diagnosis and initiating treatment are challenging.
Why diagnosing depression is difficult
Current society stigmatises ageing, with older people often reporting they feel invisible. Indeed, older people are less visible in advertising and entertainment, particularly in positive portrayals, perpetuating the ideology that old people are less valuable and old age is something to be feared and is, in itself, ‘depressing’. Medical practitioners are not immune to these unconscious biases,9 which can result in a tendency to normalise depressive symptoms in older patients and make the judgement that older patients either do not merit, or will not respond to, treatment.
Older people themselves are likely to have similar biases towards their own ageing, in a process of self-stigmatisation.10 They may therefore also normalise any depressive symptoms they experience and not disclose these to their GP. Current older generations have aged within a social framework of lower mental health literacy and greater stigmatisation of mental health issues, which further decreases the likelihood of them disclosing symptoms.
The time pressure of busy acute care hospital and general practice environments might provide a disincentive to enquiring about the presence of depressive symptoms in older patients, and is compounded by financial disincentives imposed by the Medicare Benefits Schedule (MBS) on longer consultations.11 Finally, ways in which the presenting symptoms of depression differ in old age compared with what clinicians are taught in medical school can make diagnosing depressive symptoms difficult and time consuming.
How does the presentation of depression differ in older people?
Compared with younger patients, older people are more likely to experience prominent lethargy or hypochondriacal concerns, insomnia, anxiety, nervousness and irritability; however, they are less likely to report having a depressed mood.12,13 This is important, given that many clinicians are taught that the best screening question for the presence of depression is ‘Do you think you are depressed?’ The over-representation of hypochondriacal concerns is often a clinical red herring in a general practice population that is frequently beset by multiple medical comorbidities, while a subjective complaint of nervousness or anxiety might lead a well-meaning clinician down the path of anxiety management rather than focusing on the possibility of depression.
Other symptoms that are common in an elderly population may also mislead the clinician, including sleep and appetite changes, psychomotor slowing, poor concentration, indecision and fatigue. These are common symptoms in older people who are not depressed and are also more likely to occur as part of MDD in older persons, but are often not recognised as such.14 Certain depressive subtypes, such as melancholic depression, agitated depression and psychotic depression, are more frequently seen in older people with MDD than in younger age groups.
Differential diagnosis
Organic illness should always be excluded in older patients. Central nervous system disorders, such as Parkinson’s disease and unrecognised stroke, should be considered, along with endocrine disorders such as thyroid disease and diabetes.
A cognitive diagnosis should be considered in all older patients presenting with their first depressive episode, particularly when the change in mood has no obvious precipitant. It is a mistake to think that the neurological changes associated with dementia will have impacts that are limited solely to cognition and, in fact, noncognitive presentations of dementia are quite common in clinical practice. Depression appears to be a significant risk factor for dementia, with evidence suggesting the existence of a depressive prodrome in certain individuals prior to the recognition of cognitive decline.15,16 A basic cognitive assessment should be performed as part of the initial assessment for depression in an older patient, ideally along with some form of neuroimaging to assess for the presence of infarcts or significant small vessel disease.
Other psychiatric disorders can present with episodes of low mood. A diagnosis of persistent depressive disorder (dysthymia) requires the presence of subthreshold depressive symptoms for at least two years. Anxiety disorders (obsessive-compulsive disorder, generalised anxiety disorder, panic disorder and post-traumatic stress disorder), along with a complicated grief reaction, should also be considered. A history of clinically significant periods of elevated mood should also be sought, in light of the possibility of bipolar depression being present. Drug-induced depressive episodes can arise with the use of certain prescription medications (e.g. beta blockers, sedatives, steroids, varenicline), as well as from alcohol and substance misuse.
Apathy merits special mention as, in addition to being a common depressive symptom, it can have a variety of other causes when it presents in the absence of depressed mood. People who are apathetic will often exhibit signs, such as psychomotor retardation, increased response latency and bradykinesia, which those close to them may interpret as depression. However, patients with discrete symptoms of apathy usually retain pleasure in, but lose the motivation and drive to initiate, activities. Those experiencing apathy in this context will usually deny the presence of low mood. Apathy is common in frontal lobe disorders and stroke, and following a head injury.
Treatment of depression in old age
The treatment for MDD in older people should follow a similar pathway as that for younger people, but with some important caveats. Although selective serotonin reuptake inhibitor (SSRI) antidepressants are recommended as first-line pharmacotherapy at any age, they are associated with an increased risk of falls in older people, a finding possibly related to their contributions to hyponatremia, poor balance, confusional states and orthostatic hypotension.17 Many clinicians may wisely choose to initiate antidepressants in their older patients at a lower dose to mitigate these problems. An awareness should remain, however, that the target antidepressant therapeutic dose remains the same as in younger groups.
The choice of antidepressant, otherwise, should be based on patient symptoms and drug factors. For instance, mirtazapine can be a useful choice for older patients, particularly those with insomnia and loss of appetite. Sedation and increased appetite are side effects of this drug, and these particular symptoms can be improved early by virtue of this fact, often well in advance of the true antidepressant effect becoming evident. However, the usual strategy of ‘start low, go slow’ may create issues when applied to mirtazapine because of its pharmacological profile, whereby serotonin receptors are engaged at low doses (and noradrenergic receptors progressively engaged as the dose increases), making it more sedating at low doses than at higher doses.18 The author’s frequent practice is, therefore, to initiate the drug at the 30 mg nightly dose.
Tricyclic antidepressants should generally be avoided in older people because of their anticholinergic side effect profile, which may result in dry eyes, dry mouth, blurred vision, constipation, urinary retention, confusion and falls. It should be noted that the minimum effective antidepressant doses of these agents are an order of magnitude greater than those used for pain management or for urinary incontinence.
Neurostimulation in the form of transcranial magnetic stimulation (TMS) or electroconvulsive therapy (ECT) also has a role in old-age depression. Patients presenting with melancholic, agitated and psychotic subtypes of depression are particularly responsive to ECT, which can be a life-saving intervention for patients in these states.
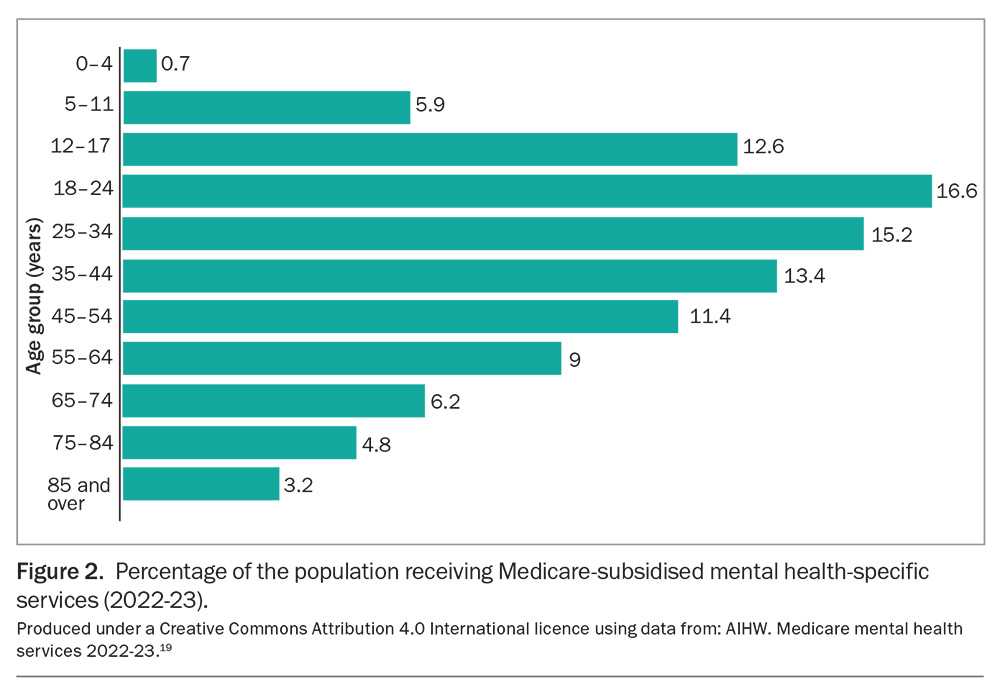
The role of psychotherapy in managing late-life depression is frequently overlooked. Although there is no evidence that psychotherapy is any less effective in older people for managing mild to moderate depression, the rates at which older people are referred for psychological interventions is very low. Data show that in any given year, people aged over 85 years are the least likely age group to receive a mental health-specific service (as delivered by a GP, psychiatrist, psychologist or other allied health professional), with the exception of children aged 0 to 4 years (Figure 2).19 It is worthwhile contrasting these data with the rates of antidepressant prescription by age in Figure 1.
Suicide in older people
The highest rates of suicide in Australia occur in those over the age of 85 years.20 The ratio of attempted to completed suicide has been reported as 4: 1 in people aged over 60 years compared with 20: 1 in those aged 20 to 40 years.21 Therefore, any suicide attempt in an older person should be taken seriously and, in the author’s view, any older person who has attempted suicide should undergo a period of psychiatric evaluation in hospital. Older men, in particular those experiencing chronic pain and who are faced with increasing dependency, are at greater risk of suicide.22 Other relevant risk factors include bereavement, increasing social isolation and chronic illness.12
Depression in dementia: the clinical dilemma
The diagnosis of MDD requires the presence of a number of specific symptoms, including complaints of depressed mood, fatigue, feelings of worthlessness or guilt, decreased concentration and thoughts of death or suicide. In other words, the diagnosis lies primarily in the ability of a person to self-report their symptoms. Reliable self-reporting is often not possible in the setting of dementia, particularly as the condition becomes more advanced.
Although reliable tools for the assessment of depression in dementia, such as the Cornell Scale for Depression in Dementia (CSDD), are widely used in nursing homes across Australia, no validation studies of these tools have been done in people living with dementia who have a Mini Mental-State Examination (MMSE) score below 10 (indicating severe dementia).23 The true prevalence of depression in this group is thus unknown, and there is no broad agreement about the diagnostic criteria for depression in those with dementia. Therefore, when considering the diagnosis of MDD in those with severe cognitive impairment, the author’s practice is to rely on those symptoms that might be at least observable to, or measurable by, others. For example, for patients living in residential care, sleep charts can capture a recent change in sleep pattern, and oral intake charts or weight charts can reflect changes in appetite. Psychomotor changes and loss of interest can also be observed by carers to the extent that these might be reliably reported. Sleep and appetite disturbances, behavioural changes and loss of interest are all invariable accompaniments of a progressive dementia. However, these symptoms progress over months to years when dementia is the underlying cause, but may develop over days to weeks in the case of depression.
The possibility of depression should be considered whenever a clinician is faced with a recent behavioural change in the setting of significant dementia. Guidelines for the management of behavioural and psychological symptoms in dementia (BPSD) recommend a range of nonpharmacological interventions as first line, followed by a trial of the SSRI citalopram as a first-line pharmacological intervention.24 The benefits of SSRI antidepressants in managing ‘behaviour’ may more likely reflect the management of unrecognised depression, rather than them having any specific effect on BPSD.
A trial of an SSRI will usually be better tolerated than alternatives such as antipsychotic medications in these circumstances. It may then be worth asking the question ‘Could this be depression?’ when faced with any new behavioural change in the setting of severe dementia.
Efficacy of antidepressant treatment in the setting of dementia
The evidence for the efficacy of antidepressant use in people with dementia is unclear. A Cochrane review identified only four studies that could be included in a meta-analysis, with a combined number of participants of only 137.25 Participants in these four studies all had mild to moderate Alzheimer’s dementia, and only two of the studies examined the efficacy of tricyclic antidepressants.
The most influential study published after the Cochrane review enrolled 326 patients from specialist old-age psychiatry services in the UK and found no difference in outcomes between those allocated to placebo, sertraline or mirtazapine after 39 weeks, using the cross-sectional standard deviation (CSSD) as the primary outcome measure.26 All three groups improved by a similar amount. Largely as a result of this Lancet study, it continues to be stated that ‘there is no evidence of therapeutic efficacy’ of antidepressants in this group.27
Although this statement is technically true, an absence of evidence of effect does not equate to evidence of an absence of effect, and the Lancet study, in which the average participant MMSE score was 18.1, has been critiqued on the basis of:
- unrepresentative sampling
- a low threshold on the CSSD for the definition of ‘caseness’
- recruitment being restricted to those with Alzheimer’s dementia
- the high rates of spontaneous remission within six months that can be expected in mildly depressed patients as part of the natural history of untreated depressive episodes
- exclusion of ‘critically depressed’ patients (e.g. those with suicide risk) from the study.28
Conclusion
Depression in older people is an important and treatable cause of morbidity in general practice. It can be difficult to diagnose in busy medical settings, particularly in the presence of severe dementia, where standardised diagnostic criteria can be difficult to apply. Data on the efficacy of antidepressants in dementia are inconclusive. MT
COMPETING INTERESTS: Associate Professor Macfarlane has received consulting fees from Eli Lilly, Eisai and George Clinical and speaker fees from Eisai; is on Advisory Boards for Eli Lilly, Eisai and Janssen-Cilag; and is a Medical Monitor for Anavex Life Sciences Corporation.
References
1. James S, Abate D, Abate K, et al. 2018. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392: 1789-1858.
2. Kruijshaar M, Barendregt J, Vos T, de Graaf R, Spijker J, Andrews G. Lifetime prevalence estimates of major depression: an indirect estimation method and a quantification of recall bias. Eur J Epidem 2005; 20: 103-111.
3. Schaakxs R, Comijs H, van der Mast R, Schoevers R, Beekman A, Penninx B. Risk factors for depression: differential across age? Am J Ger Psych 2017; 25: 966-977.
4. Katona C. Depression in old age. Rev Clin Gerontol 1991; 1: 371-384.
5. Seitz D, Purandare N, Conn D. Prevalence of psychiatric disorders among older adults in long-term care homes: a systematic review. Int Psychoger 2010; 22: 1025-1039.
6. Cuijpers S. Depressive disorders in caregivers of dementia patients: a systematic review. Ageing Mental Health 2005; 9: 325-330.
7. Australian Bureau of Statistics (ABS). Patterns of use of mental health services and prescription medications, 2011. ABS; Canberra, 2016. Available online at: https://www.abs.gov.au/statistics/health/mental-health/patterns-use-mental-health-services-and-prescription-medications/latest-release#pbs-subsidised-prescription-medications (accessed May 2024).
8. Malhl GS, Acar M, Kouhkamari MH, Chien TH, Juneja P, Siva S, Baune BT. Antidepressant prescribing patterns in Australia. BJPsych Open 2022; 8: e120.
9. Ben-Harush A, Shiovitz-Ezra S, Doron I, et al. Ageism among physicians, nurses and social workers: findings from a qualitative study. Eur J Ageing 2017; 14: 39-48.
10. Hausknecht S, Low L-F, O’Laughlin K, McNab J, Clemson L. Older adults’ self-perceptions of aging and being older: a scoping review. Gerontologist 2020; 60: e524-e534.
11. Ashcroft R, Silveira J, Rush B, McKenzie K. Incentives and disincentives for the treatment of depression and anxiety: a scoping review. Can J Psychiatry 2014; 59: 385-392.
12. Katona C. Managing depression in older people. Adv Psych Treat 1996; 2: 178-185.
13. Hegeman JM, Kok RM, van der Mast RC, Giltay EJ. Phenomenology of depression in older compared with younger adults: meta-analysis. Br J Psychiatry 2012; 200: 275-281.
14. Bergua V, Blanchard C, Amieva H. Depression in older adults: do current DSM diagnostic criteria really fit? Clin Gerontol 2023; 30: 1-38.
15. Saczynski J, Beiser A, Seshadri S, Auerbach S, Wolf P, Au R. Depressive symptoms and risk of dementia: the Framingham Heart Study. Neurology 2010; 75: 35-41.
16. Wiels W, Baeken C, Engelborghs S. Depressive symptoms in the elderly—an early symptom of dementia? A systematic review. Front Pharmacol 2020; 11: 34.
17. van Poelgeest E, Pronk A, Rhebergen D, van der Velde N. Depression, antidepressants and falls risk: therapeutic dilemmas – a clinical review. Eur Ger Med 2021; 12: 585-596.
18. Leonard S, Karlamangla A. Dose-dependent sedating and stimulating effects of mirtazapine. Proc UCLA Healthc 2015; 19: 1-2.
19. Australian Institute of Health and Welfare (AIHW). Medicare mental health services 2022-23. Canberra; AIHW, updated 2024. Available online at: https://www.aihw.gov.au/mental-health/topic-areas/medicare-subsidised-services#Who-received-MBS-services (accessed May 2024).
20. Australian Institute of Health and Welfare (AIHW). Suicide & self-harm monitoring. Canberra; AIHW, updated 2023. Available online at: https://www.aihw.gov.au/suicide-self-harm-monitoring/data/deaths-by-suicide-in-australia/suicide-deaths-over-time (accessed May 2024).
21. Parkin D, Stengel E. Incidence of suicide attempts in an urban community. BMJ 1965; 2: 133-138.
22. De Leo D. Late-life suicide in an aging world. Nature Aging 2022; 2: 7-12.
23. Goodarzi Z, Mele B, Roberts D, Holroyd-Leduc J. Depression case finding in individuals with dementia: a systematic review and meta-analysis. JAGS 2017; 65: 937-948.
24. Kales H, Lyketsos C, Miller M, Ballard C. Management of behavioral and psychological symptoms in people with Alzheimer’s disease; an international Delphi consensus. Int Psychoger 2019; 31: 83-90.
25. Bains J, Birks JS, Dening TR. Antidepressants for treating depression in dementia. Cochrane Database Syst Rev 2002; (4): CD003944.
26. Banerjee S, Hellier J, Dewey M, et al. Sertraline or mirtazapine for depression in dementia (HTA-SADD): a randomised, multicentre, double-blind, placebo-controlled trial. Lancet 2011; 378: 403-411.
27. Costello H, Rosier J, Howard R. Antidepressant medications in dementia: evidence and potential mechanisms of treatment-resistance. Psychol Med 2023; 53: 654-667.
28. Macfarlane S, McKay R, Looi J. Limited antidepressant efficacy in depression in dementia, in the context of limited evidence. Aust NZ J Psych 2012; 46: 595-597.