Inhaler therapy for COPD. An individualised approach to inhaler selection

Inhaled therapy for chronic obstructive pulmonary disease can help reduce exacerbation frequency, admission to hospital and risk of death. Appropriate inhaler choice for the patient’s capabilities and education and frequent assessment of inhaler technique can help improve adherence to therapy.
- Adherence and inhaler satisfaction copredict improved health outcomes for patients with chronic obstructive pulmonary disease (COPD).
- The best inhaler device for a patient with COPD is one they can use; patient- and device-related factors should be considered when choosing an inhaler device.
- Assessment of a patient’s co-ordination and inspiratory flow patterns should guide selection of inhaler devices.
- Adherence and device technique should be assessed regularly and before changing a patient’s therapy.
- Patients should use only one type of device for all of their inhaled therapies, where possible.
Chronic obstructive pulmonary disease (COPD) affects around one in seven adults over the age of 40 years in Australia and rises to 29% among people aged 75 years and older.1,2 This common respiratory condition is the leading cause of potentially preventable hospital admissions.3 Optimal management of COPD requires nonpharmacological and pharmacological strategies to optimise function through symptom relief and to reduce the risk of exacerbations. All patients with COPD can benefit from smoking cessation, pulmonary rehabilitation and vaccination.1 Effective management of COPD should involve a multidisciplinary team including general practitioners, pharmacists, allied health professionals and practice or respiratory nurses.4 This collaborative approach can help enhance quality of life and reduce disability for patients living with COPD.1
Although pharmacological therapy has not been shown to slow decline in lung function over time, inhaled therapy can reduce exacerbation frequency and improve symptoms and exercise tolerance.1 This article outlines the inhaler devices available in Australia and discusses their benefits and drawbacks with respect to co-ordination of actuation and the patient’s capabilities and preferences.
Medication management
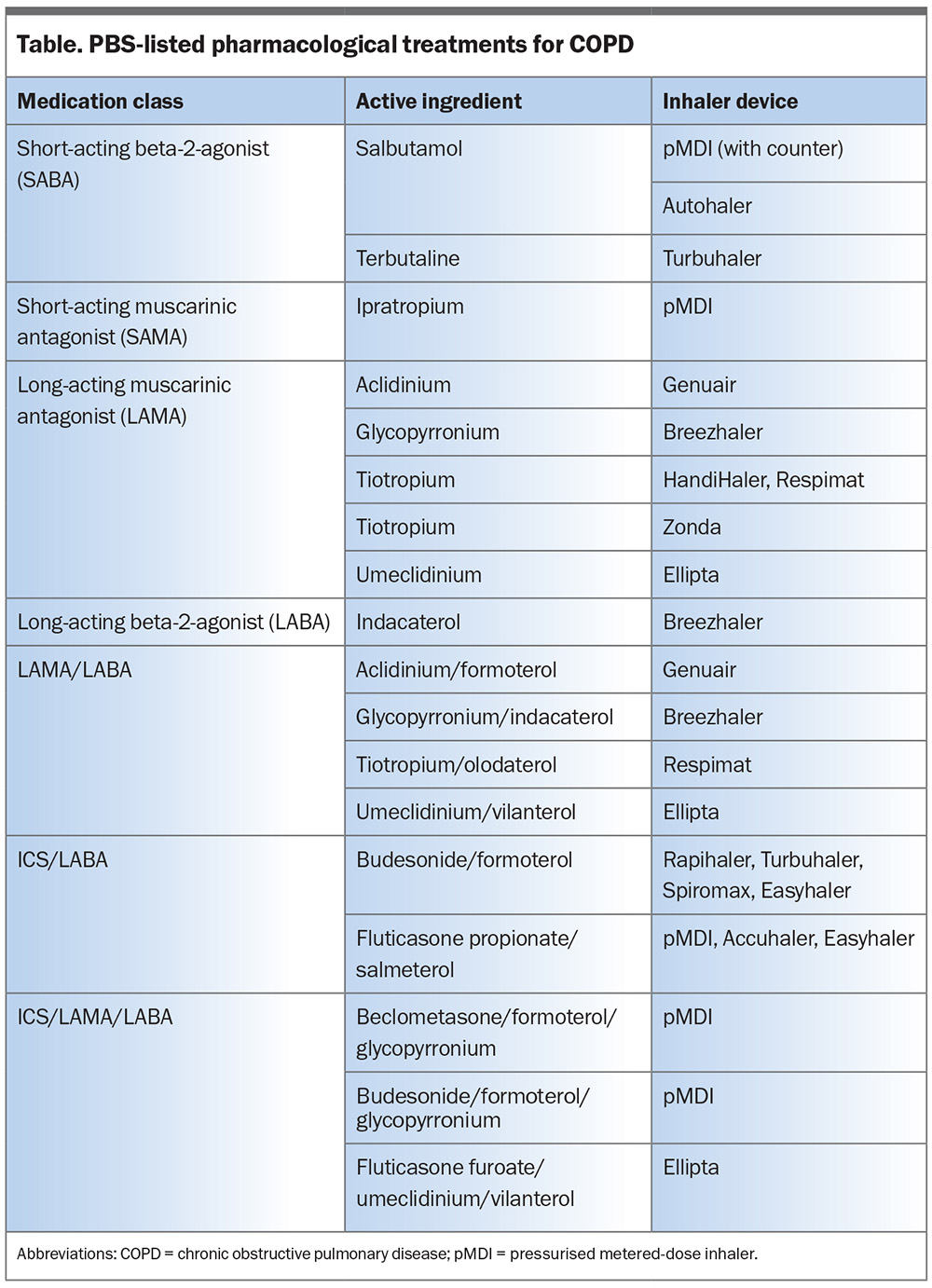
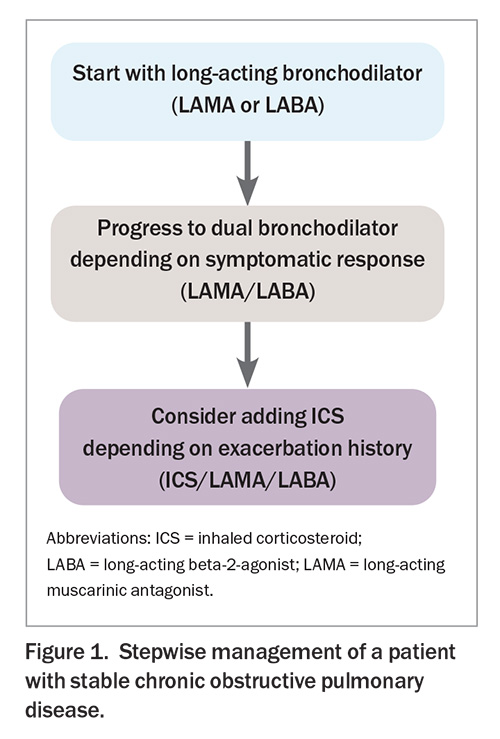
The mainstay of pharmacological treatment of COPD is inhaled bronchodilators and corticosteroids (Table). The Lung Foundation Australia recommends a stepwise approach to the pharmacological management of patients with stable COPD based on increasing severity of symptoms, lung function and history of exacerbations (Figure 1).5 Inhaler device technique should be assessed and optimised at every opportunity.1 Inhaler device polypharmacy should be minimised by using single-inhaler dual and triple therapy, where possible.
Adherence
Adherence to inhaled medication regimens is associated with reduced risk of death and admissions to hospital due to exacerbations in COPD.6 Inhaler devices vary widely with regard to technique, patient suitability and patient preference; therefore, choosing the right device for the individual patient is crucial to ensuring correct technique and improving the likelihood of good adherence to therapy.7 A large multinational survey showed that patients’ overall satisfaction with their inhaler was significantly associated with treatment adherence, resulting in fewer exacerbations and fewer hospitalisations due to exacerbations.8 Exploring a patient’s concerns and capabilities is important when initiating or switching devices.7 Pharmacists can play a pivotal role in optimising adherence and persistence, and providing education on safe and effective use of medications for COPD when dispensing and conducting collaborative medication reviews.
Inhaler selection
Inhaled therapy is the primary route of administration for the treatment of patients with COPD. It comprises bronchodilators, antimuscarinic agents and corticosteroids delivered via various inhaler devices. A growing number of inhaler devices are available in Australia and can be grouped as:
- pressurised metered-dose inhalers (pMDIs)
- breath-actuated (BA)-pMDIs
- soft mist inhalers (SMIs)
- dry powder inhalers (DPIs).
Simultaneous use of different inhaler types, particularly a mixture of pMDI and DPI devices, is predictive of increased errors in inhalation and poor adherence to therapy.9 Therefore, where possible, patients should use a single inhaler device to deliver multiple pharmacotherapies.
Aerosol science
A number of device-related factors influence aerosol deposition in the airways and include the following.
Particle size
Inhaler devices need to generate drug particles of an appropriate size to penetrate beyond the oropharyngeal area and deposit in the lungs. The aerodynamic diameter is the most important particle-related factor that affects aerosol deposition.10 Particles greater than 5 micrometre are most likely to deposit by impaction in the oropharynx and be swallowed; particles between 1 and 5 micrometre will deposit in the large and conducting airways; and particles less than 1 micrometre are likely to reach the peripheral airways and alveoli or be exhaled.10,11 Aerosols with high fine particle fraction have a high probability of penetrating beyond the upper airways and depositing in the lungs.10 In the peripheral airways, particles deposit predominantly by sedimentation, highlighting the importance of breath-hold after inhalation with some inhaler devices.11
Aerosol velocity and duration
pMDIs generate a high velocity cloud over a short period of time, creating difficulties in synchronising inhaler actuation with inspiration. High aerosol velocity from pMDIs also increases the probability of deposition by impaction in the oropharynx and large conducting airways.11 Only about 10 to 20% of the delivered dose from a pMDI is deposited in the lungs.12 Use of spacers with pMDIs reduces aerosol particle velocity, increasing lung deposition. Aerosol velocity from an SMI (such as Respimat) is three to 10 times slower than for pMDIs.13 The mean spray duration is 1.5 seconds, compared with 0.15 to 0.36 seconds for pMDIs.14
Inspiratory flow rate and volume
The patient’s inspiratory volume and flow rate are important patient-related factors influencing aerosol deposition in the airways. Each inhaler device has its own unique optimal peak inspiratory flow rate (PIFR).15 For pMDIs, BA-pMDIs and SMIs, inspiratory flow rate should be about 30 L/min to minimise deposition in the upper airways and enhance delivery to the lungs.10
Exhalation before inhalation
Exhalation to functional residual capacity or residual volume increases PIFR and inhaled volume, which may augment drug dispersion and facilitate fine particle generation from a DPI.16 This is also a commonly missed step before actuation with pMDIs.17
Internal resistance of inhaler
The internal resistance of DPIs varies by device, requiring different inspiratory effort to produce sufficient flow rate.18 Lower resistance devices require patients to produce a higher PIFR at a given pressure gradient than higher resistance devices.19
Duration of breath-hold
Breath-holding increases lung deposition through the process of sedimentation.11 Although the breath-hold capacity of patients with COPD is often limited, it is important that patients are advised to hold their breath for five seconds, or as long as possible, after inhalation.20 Breath-holding time may be more critical with fine particle pMDIs.9
Metered dose and soft mist inhalers
pMDIs are aerosol-based devices that require a slow and steady inhalation over four to five seconds to reduce oropharyngeal deposition and optimise delivery to the lungs.10 pMDIs come as either a solution or suspension system and all contain propellants. Co-ordination of actuation with inhalation is required with pMDIs.
SMIs, for example Respimat, generate an aerosol mist from an aqueous solution and do not contain propellants.13 Respimat has a significantly slower plume velocity and longer spray duration compared with pMDIs.13 Therefore, SMIs require less patient co-ordination than pMDIs.19
Spacers
Co-ordination errors are the most common error with pMDIs.10,21,22 Many patients cannot use a pMDI correctly, even with education and training. Spacers can be used to overcome the difficulty of co-ordinating inhalation and actuation while inhaling slowly and deeply.11 If a slow inhalation over four to five seconds is not achievable, tidal breathing with four breaths in and out normally through the spacer is an alternative method. In addition, spacers reduce oropharyngeal deposition, facilitate vaporisation of particles to an optimal size and increase deposition of the active ingredient in the lungs.9,23 When using a spacer, it is important for patients to shake the pMDI before use and start inhalation promptly, as aerosolised particles remain suspended in the spacer for less than 10 seconds.9 It is also important that the pMDI is shaken before a second dose via a spacer.
Dry powder inhalers
DPIs are breath-actuated devices that deliver the medication in powder form from a capsule, reservoir or sealed blister strip. DPIs require exhalation to functional residual capacity before inhalation with a forceful, deep inhalation over two to three seconds.10
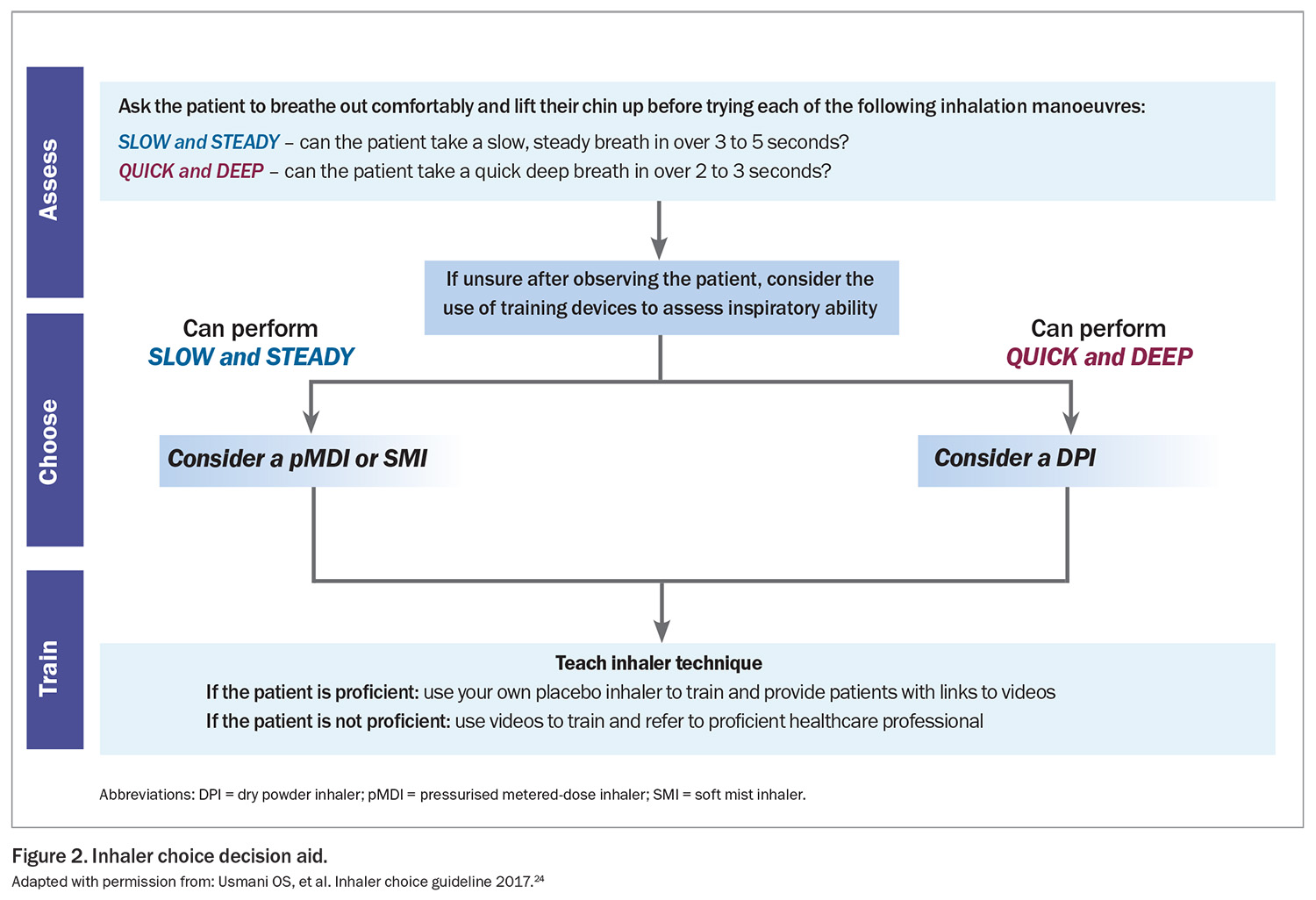
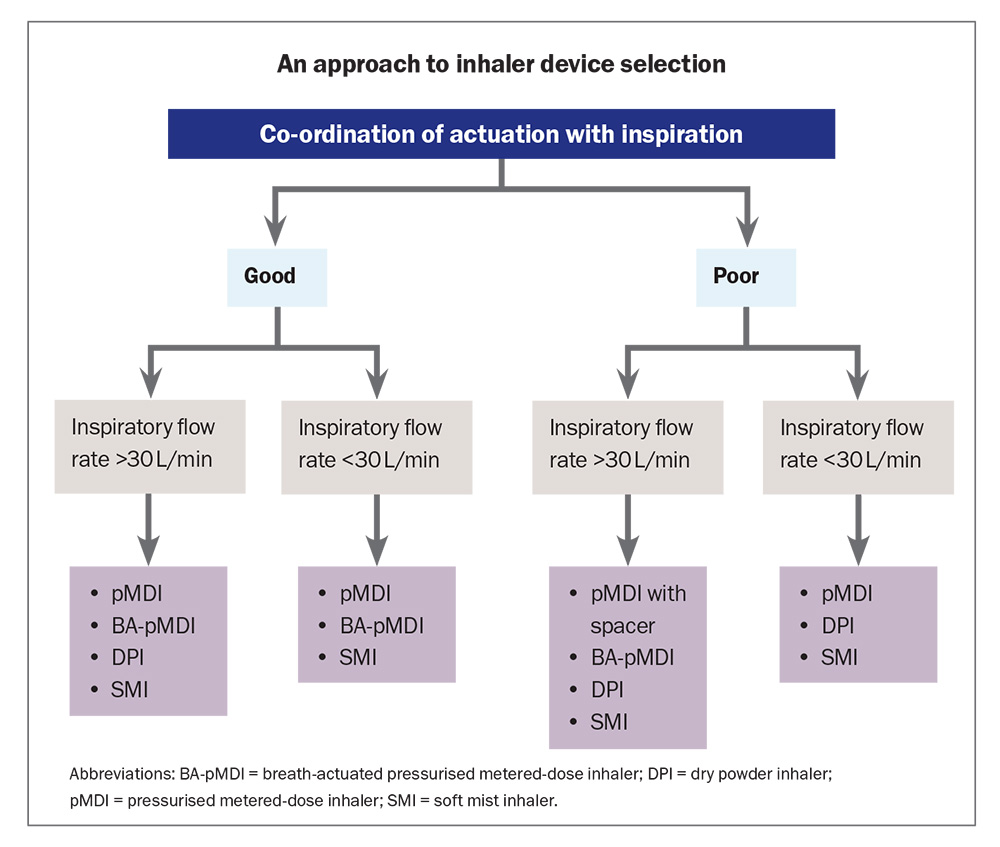
The European Respiratory Society/International Society for Aerosols in Medicine taskforce recommends choosing an inhaler based on two factors:10
- level of inspiratory flow
- co-ordination of inhalation/actuation (Figure 224).
When considering prescribing a DPI, evaluating the patients’ PIFR is important. Patients with COPD may have severe airflow limitation, accompanied by decreased inspiratory capacity, hyperinflation and compromised respiratory muscles, which may reduce inspiratory flow rates and diminish lower airway deposition from DPIs. Suboptimal PIFR in patients with COPD may limit their ability to effectively use DPIs and deliver the medication throughout the lungs, particularly during acute exacerbations.11,19,24,25 However, most patients with COPD are able to generate inspiratory flows necessary for effective DPI use.26
Insufficient inspiratory flow rate is one of the most common errors with DPIs.10,21,22,27 A PIFR value of 60 L/min is generally accepted to be optimal for most DPIs.28 PIFR values greater than 60 L/min can be associated with excessively turbulent flow and therefore poor lung deposition.15 A quick and forceful inhalation is required with DPIs to deagglomerate the active ingredient powder from carrier powder (usually lactose) and aerosolise the particles.10 Airflow achieved early in the inspiratory profile disaggregates drug from carrier powder and determines particle size distribution of the aerosol.29
The minimal inspiratory flow rate required for low resistance DPI devices (e.g. Breezhaler) is above 90 L/min, 50 to 60 L/min for medium-resistance DPI (e.g. Turbuhaler, Genuair, Spiromax) and below 50 L/min for a high-resistance DPI (e.g. Handihaler).30
Although the optimal flow rate differs between each DPI device due to differences in inhaler design and internal resistance, the principle remains the same for all – a rapid and forceful inhalation is required. It is important that the inspiratory flow rate at the start of the inhalation is forceful, rather than gradually increasing.31
A decision algorithm based on inspiratory flow rate and ability to co-ordinate inhalation actuation is shown in the Flowchart.32 An In-Check Dial is a handheld device with an adjustable dial to mimic the internal resistance of different inhalers and can be used to measure and identify suboptimal PIFR and optimise inhaler device selection.15
Inhaler technique
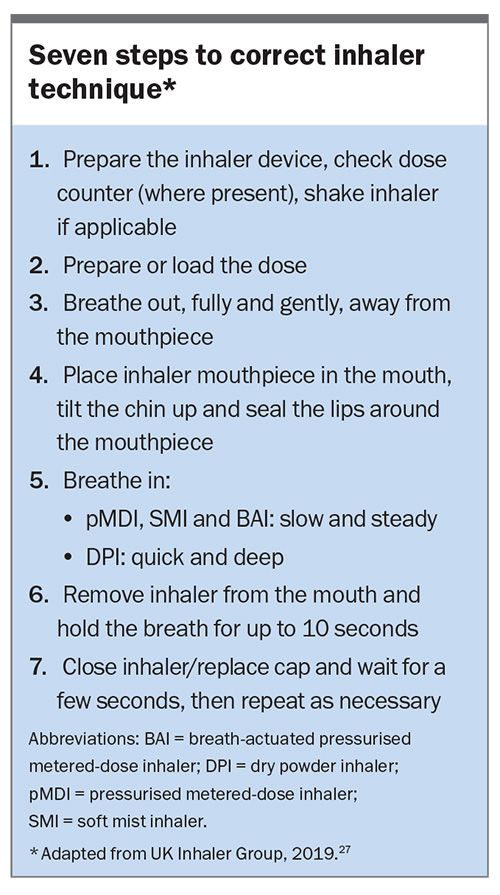
Optimal inhaler technique is critical to effective COPD management. When used correctly, all inhalers are effective and can achieve the same therapeutic effect, although different doses may be required.33 Mastering an inhaler device involves correct preparation and handling before inhalation, and optimal inhalation technique. There are seven basics steps to using an inhaler device, pertinent to all devices (Box).34 Errors in any step may lead to inadequate drug delivery to the lungs.
Up to 94% of patients do not use their inhaler device correctly, resulting in inadequate dosing, suboptimal disease control, worsening of quality of life and increased hospital admissions and mortality.35 A recent analysis of inhaler technique in 364 patients with COPD showed that two-thirds of patients made one or more crucial errors, particularly among those using several different devices.36 The most common errors with DPIs include failure to exhale before actuation, failure to breath-hold after inhalation, incorrect positioning of the inhaler, incorrect rotation sequence and failure to execute a forceful and deep inhalation.35 Common errors with pMDIs include insufficient inspiratory force (not slow and deep enough), failure to actuate before inhalation and breath-hold after inhalation and incorrect second-dose preparation, timing or inhalation.21 Older age, cognitive impairment, multiple inhaler devices and lack of previous training are all risk factors for poor inhaler use and adherence.37
As many as 25% of patients have never received verbal inhaler technique instruction.35 All health professionals involved in the care of patients with COPD should check a patient’s inhaler technique at every opportunity. Numerous studies show that inhaler technique interventions in community pharmacies can be effective.38-41 Pharmacists conducting comprehensive medication reviews (Home Medicine Review) have an opportunity to check inhaler device technique in the privacy of the patient’s home. Providing written instructions highlighting incorrect steps helps patients maintain correct technique for longer.38 Inhaler technique can decline in as little as one to two months after mastering correct technique; therefore, follow-up over time is essential to maintain correct technique.42,43 Videos on inhaler device technique are available on the Lung Foundation Australia website (https://lungfoundation.com.au/patients-carers/after-your-diagnosis-title/inhaler-devices/).
Conclusion
Choosing the right inhaler for the right patient is crucial to optimal management for patients living with COPD. Choice of an inhaler can be based on many patient and prescriber factors; two important patient-related factors are the patient’s inspiratory flow rate and their ability to co-ordinate inhalation and actuation. The patient’s inhaler preferences should also be considered. Inhaler device technique should be diligently reviewed and optimised at each formal review and at other opportune times. Multidisciplinary collaboration can improve the management of patients with COPD in primary care. RMT
References
1. Yang I, Dabscheck E, George J, et al. The COPD-X Plan: Australian and New Zealand Guidelines for the management of chronic obstructive pulmonary disease. Version 2.63, February 2021.
2. Toelle BG, Xuan W, Bird TE, et al. Respiratory symptoms and illness in older Australians: The Burden of Obstructive Lung Disease (BOLD) study. Med J Aust 2013; 198: 144-148.
3. Australian Institute of Health and Welfare (AIHW). Disparities in potentially preventable hospitalisations across Australia, 2012-13 to 2017-18. AIHW; Canberra, 2020. Available online at: https://www.aihw.gov.au/reports/primary-health-care/disparities-in-potentially-preventable-hospitalisations-exploring-the-data/contents/introduction (accessed August 2021).
4. Therapeutic Guidelines. eTG Complete. Therapeutic Guidelines: Respiratory. West Melbourne; Therapeutic Guidelines Limited, 2021.
5. Lung Foundation Australia. Stepwise management of stable COPD. Available online at: https://https://lungfoundation.com.au/resources/stepwise-management-of-stable-COPD/ (accessed August 2021).
6. Vestbo J, Annderson JA, Calverley PM, et al. Adherence to inhaled therapy, mortality and hospital admission in COPD. Thorax 2009; 64: 939-943.
7. Dekhuijzen R, Lavorini F, Usmani OS, van Boven JFM. Addressing the impact and unmet needs of nonadherence in asthma and chronic obstructive pulmonary disease: where do we go from here? J Allergy Clin Immunol Pract 2018; 6: 785-793.
8. Chrystyn H, Small M, Milligan G, Higgins V, Gil EG, Estruch J. Impact of patients’ satisfaction with their inhalers on treatment compliance and health status in COPD. Respir Med 2014; 108: 358-365.
9. Levy ML, Dekhuijzen PNR, Barnes PJ, et al. Inhaler technique: facts and fantasies. A view from the Aerosol Drug Management Improvement Team (ADMIT). NPJ Prim Care Respir Med 2016; 26: 16017.
10. Laube BL, Janssens HM, de Jongh FHC, et al. What the pulmonary specialist should know about the new inhalation therapies. Eur Respir J 2011; 37: 1308-1331.
11. Capstick TG, Clifton IJ. Inhaler technique and training in people with chronic obstructive pulmonary disease and asthma. Expert Rev Respir Med 2012; 6: 91-103.
12. Newman SP, Pavia D, Moren F, Sheahan NF, Clarke SW. Deposition of pressurised aerosols in the human respiratory tract. Thorax 1981; 36: 52-55.
13. Wachtel H, Kattenbeck S, Dunne S, Disse B. The Respimat® development story: patient-centered innovation. Pulm Ther 2017; 3: 19-30.
14. Hochrainer D, Holz H, Kreher C, Scaffidi L, Spallek M, Wachtel H. Comparison of the aerosol velocity and spray duration of Respimat Soft Mist Inhaler and pressurized metered dose inhalers. J Aerosol Med 2005; 18: 273-282.
15. Ghosh S, Pleasants RA, Ohar JA, Donohue JF, Bradley Drummond M. Prevalence and factors associated with suboptimal peak inspiratory flow rates in COPD. Int J Chron Obstruct Pulmon Dis 2019; 14: 585-595.
16. Kondo T, Hibino M, Tanigaki T, Ohe M, Kato S. Exhalation immediately before inhalation optimizes dry powder inhaler use. J Asthma 2015; 52: 935-939.
17. Bonds RS, Asawa A, Ghazi AI. Misuse of medical devices: a persistent problem in self-management of asthma and allergic disease. Ann Allergy Asthma Immunol 2015; 114: 74-76.
18. Ciciliani A, Langguth P, Wachtel H. In vitro dose comparison of Respimat® inhaler with dry powder inhalers for COPD maintenance therapy. Int J Chron Obstruct Pulmon Dis 2017; 12: 1565-1577.
19. Ghosh S, Ohar JA, Bradley Drummond M. Peak inspiratory flow rate in chronic obstructive pulmonary disease: implications for dry powder inhalers. J Aerosol Med Pulm Drug Deliv 2017; 30: 381-387.
20. Horváth A, Balásházy I, Tomisa G, Farkas A. Significance of breath-hold time in dry powder aerosol drug therapy of COPD patients. Eur J Pharm Sci 2017; 104: 145-149.
21. Price DB, Román-Rodríguez M, McQueen RB, et al. Inhaler errors in the CRITIKAL Study: type, frequency, and association with asthma outcomes. J Allergy Clin Immunol Pract 2017; 5: 1071-1081.
22. Bosnic-Anticevich S, Cvetkovski B, Azzi EA, Srour P, Tan R, Kritikos V. Identifying critical errors: addressing inhaler technique in the context of asthma management. Pulm Ther 2018; 4: 1-12.
23. Newman SP. Spacer devices for metered dose inhalers. Clin Pharmacokinet 2004; 43: 349-360.
24. Usmani OS, Capstick T, Saleem A, Scullion J. Choosing an appropriate inhaler device for the treatment of adults with asthma or COPD. Available online at: https://www.guidelines.co.uk/respiratory/inhaler-choice-guideline/252870.article (accessed August 2021).
25. Dekhuijzen PN, Lavorini F, Usmani OS. Patients’ perspectives and preferences in the choice of inhalers: the case for Respimat(®) or HandiHaler(®). Patient Prefer Adherence 2016; 10: 1561-1572.
26. Clark AR, Weers JG, Dhand R. The confusing world of dry powder inhalers: it is all about inspiratory pressures, not inspiratory flow rates. J Aerosol Med Pulm Drug Deliv 2020; 33: 1-11.
27. Sulaiman I, Cushen B, Greene G, et al. Objective assessment of adherence to inhalers by patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2017; 195: 1333-1343.
28. Mahler DA. Peak inspiratory flow rate as a criterion for dry powder inhaler use in chronic obstructive pulmonary disease. Ann Am Thorac Soc 2017; 14: 1103-1107.
29. Dalby R, Spallek M, Voshaar T. A review of the development of Respimat® Soft MistTM Inhaler. Int J Pharm 2004; 283: 1-9.
30. Lavorini F, Fontana GA, Usmani OS. New inhaler devices-the good, the bad and the ugly. Respiration 2014; 88: 3-15.
31. Chrystyn H. Is inhalation rate important for a dry powder inhaler? Using the In-Check Dial to identify these rates. Respir Med 2003; 97: 181-187.
32. Chapman KR, Voshaar TH, Virchow JC. Inhaler choice in primary practice. Eur Respir Rev 2005; 14: 117-122.
33. Dolovich MB, Ahrens RC, Hess DR, et al. Device selection and outcomes of aerosol therapy: evidence-based guidelines: American College of Chest Physicians/American College of Asthma, Allergy, and Immunology. Chest 2005; 127: 335-371.
34. Scullion J, Fletcher M. UK Inhaler Group: inhaler standards and competency document. 2018. Available online at: https://www.ukinhalergroup.co.uk/uploads/c4F3tq04/InhalerStandards2018.pdf (accessed August 2021).
35. Lavorini F, Magnan A, Dubus JC, et al. Effect of incorrect use of dry powder inhalers on management of patients with asthma and COPD. Respir Med 2008; 102: 593-604.
36. Sulku J, Bröms K, Högman M, et al. Critical inhaler technique errors in Swedish patients with COPD: a cross-sectional study analysing video-recorded demonstrations. NPJ Prim Care Respir Med 2021; 31: 5.
37. Usmani OS, Lavorini F, Marshall J, et al. Critical inhaler errors in asthma and COPD: a systematic review of impact on health outcomes. Respir Res 2018; 19: 10.
38. Basheti IA, Armour CL, Bosnic-Anticevich SZ, Reddel HK. Evaluation of a novel educational strategy including inhaler-based reminder labels, to improve asthma inhaler technique. Patient Educ Couns 2008; 72: 26-33.
39. Tommelein E, Mehuys E, Van Hees T, et al. Effectiveness of pharmaceutical care for patients with chronic obstructive pulmonary disease (PHARMACOP): a randomized controlled trial. Br J Clin Pharmacol 2014; 77: 756-766.
40. Gray NJ, Long NC, Mensah N. Report of the evaluation of the greater Manchester Community pharmacy inhaler technique service (2014). Available online at: https://psnc.org.uk/greater-manchester-lpc (accessed August 2021).
41. Mehuys E, Van Bortel L, de Bolle L, et al. Effectiveness of pharmacist intervention for asthma control improvement. Eur Respir J 2008; 31: 790-799.
42. Ovchinikikova L, Smith L, Bosnic-Anticevich S. Inhaler technique maintenance: gaining an understanding from the patient’s perspective. J Asthma 2011; 48: 616-624.
43. Bosnic-Anticevich SZ, Sinha H, So S, Reddel HK. Metered-dose inhaler technique: the effect of two educational interventions delivered in community pharmacy over time. J Asthma 2010; 47: 251-256.
COMPETING INTERESTS: Clinical Associate Professor Rigby is the Clinical Executive Lead, National Asthma Council and is on the COPD Advisory Committee and Primary Care Advisory Committee, Lung Foundation Australia; and reports honoraria for presentations, conference registration, travel and advisory groups from AstraZeneca, Boehringer Ingelheim, Care Pharmaceuticals, Chiesi, GSK, Menarini, MSD, Mundipharma, Respiri and Teva.