Nonviral hepatitis: common causes and their management
The proportion of hepatitis cases due to nonviral causes is increasing, given therapeutic advances for chronic viral hepatitis in recent years. Initial assessment can lead to a positive diagnosis and early management, and many patients can be safely and effectively managed in primary care.
- The most common causes of nonviral liver disease that may present as a hepatitis include metabolic-associated fatty liver disease (MAFLD), alcohol-related liver disease (ALD) and drug-induced liver injury (DILI).
- A thorough medication history should be taken for patients with hepatitis, including prescription and over-the-counter medications as well as herbal and dietary supplements.
- Targeted blood tests may reveal causes of nonviral hepatitis.
- Patients with features of severe liver injury, liver failure or cirrhosis should be referred for urgent hepatology assessment and, in appropriate cases, hospitalisation.
Hepatitis refers to liver inflammation, usually brought to attention by asymptomatic elevation of serum aminotransferases (aspartate aminotransferase [AST] or alanine aminotransferase [ALT]) or by symptoms, such as nausea, fatigue, abdominal discomfort or jaundice. Acute or chronic viral hepatitis can be readily excluded through serological testing, but the evaluation of nonviral causes may be more complex. Nonviral liver disorders that should be considered include, but are not limited to, alcohol-related liver disease (ALD), metabolic-associated fatty liver disease (MAFLD), drug- or toxin-induced liver injury (DILI), biliary or pancreatic disorders and, less commonly, autoimmune disorders, genetic disorders and Budd-Chiari syndrome. Hepatitis can be acute or chronic (arbitrarily defined as lasting more than six months), with prolonged inflammation resulting in fibrosis and cirrhosis in some individuals. Given the significant therapeutic advances for chronic viral hepatitis in recent years, the proportion of nonviral liver disease as a cause of hepatitis is increasing, as is the prevalence. This article presents an approach to the investigation and management of the common causes of nonviral hepatitis.
Assessing nonviral hepatitis
A diagnostic approach can be used to assess patients with nonviral hepatitis, as discussed below and presented in the Flowchart. The indications for specialist involvement and the red flags for urgent referral are listed in Box 1 and Box 2.
Symptoms and presenting features
Patients with hepatitis are frequently asymptomatic, with elevated liver enzymes levels being found on routine blood tests. Some patients present with nonspecific symptoms, such as lethargy, nausea and/or vomiting, anorexia, abdominal pain, fevers and jaundice, which prompt further investigation.
Marked elevation of serum AST and ALT levels (greater then 500 U/L) may reflect severe liver injury and can be associated with acute liver failure marked by coagulopathy and encephalopathy. This a medical emergency and patients require immediate hospitalisation. Nonviral conditions to consider are severe autoimmune hepatitis, DILI and ischaemic hepatitis.
Of note, severe alcoholic hepatitis is associated with jaundice but without marked elevations of AST and ALT levels. Acute biliary colic may present with upper abdominal pain and marked elevation of AST and ALT before changing to a more cholestatic pattern of liver test abnormality (see below).
History
Undertaking a thorough history is fundamental in assessing the cause of nonviral hepatitis. This includes a detailed history of the presenting illness, current and past alcohol intake, recreational drug use and medication history (including prescription and nonprescription medications, especially anabolic-androgenic steroids in bodybuilders and herbal or dietary supplements).
With MAFLD affecting at least 25% of adults and increasing numbers of children and adolescents, a full metabolic risk assessment is essential. This should include recent weight changes, dietary habits, physical activity levels and comorbid conditions such as obesity, type 2 diabetes, dyslipidaemia and hypertension.
A family history of liver disease or a personal history of intercurrent illnesses may be relevant. Intercurrent illnesses of concern include autoimmune conditions (such as thyroid disease, coeliac disease and inflammatory bowel disease), gallbladder disease, pancreatic disease, cardiovascular disease and malignancy.
Physical examination
Although physical examination of a patient with hepatitis may not always reveal significant abnormalities, it is important to look for clinical signs that may suggest an underlying aetiology. Increased waist circumference and hepatomegaly may be observed in patients with MAFLD. Tender hepatomegaly and fevers are often seen in patients with acute hepatitis, and jaundice can be seen with any form of severe acute hepatitis.
Upper abdominal or right upper quadrant pain is suggestive of biliary disease. Clinical features suggestive of cirrhosis and portal hypertension must be noted, including jaundice, palmar erythema, spider naevi, splenomegaly, ascites and peripheral oedema. The presence of hepatic encephalopathy warrants urgent hospital admission.
Investigations
Liver function tests can be used to determine whether the hepatitis has a hepatocellular (elevated AST and/or ALT levels) or cholestatic (elevated alkaline phosphatase [ALP] and/or gamma-glutamyl transferase [GGT] levels) pattern. The ALT to AST ratio may also provide clues regarding the underlying aetiology. Hyperbilirubinaemia may be present in severe disease. A prolonged INR can reflect synthetic dysfunction and may indicate liver failure; thrombocytopenia and a low serum albumin may suggest underlying cirrhosis and portal hypertension.
Further investigations for the diagnosis of specific conditions when there is clinical suspicion and appropriate clinical context are listed in the Table. These tests are not indicated in all circumstances. Viral hepatitis must always be excluded when assessing patients with liver disease.
Imaging studies
An abdominal ultrasound is a readily available test that should be performed in all patients with deranged liver function tests. It may provide relevant information, including:
- increased echogenicity suggestive of hepatic steatosis
- presence of gallstones or dilated biliary tree
- presence of hepatomegaly
- features of cirrhosis (nodular liver contour, coarse and heterogeneous echotexture)
- features of portal hypertension (dilated portal vein, recanalisation of umbilical vein, ascites, splenomegaly)
- presence of liver lesions
- presence of venous thrombosis.
Noninvasive tools to assess liver stiffness have an important role in fibrosis stage assessment. Vibration-controlled transient elastography (FibroScan) is readily available at most hospital liver clinics, and testing on a portable machine may be available at community-based clinics. Shear-wave elastography, which is available on the ultrasound machines used in many radiology practices, has a similar ability to determine significant fibrosis or cirrhosis but is supported by fewer validation studies.
Causes of nonviral hepatitis
Metabolic-associated fatty liver disease
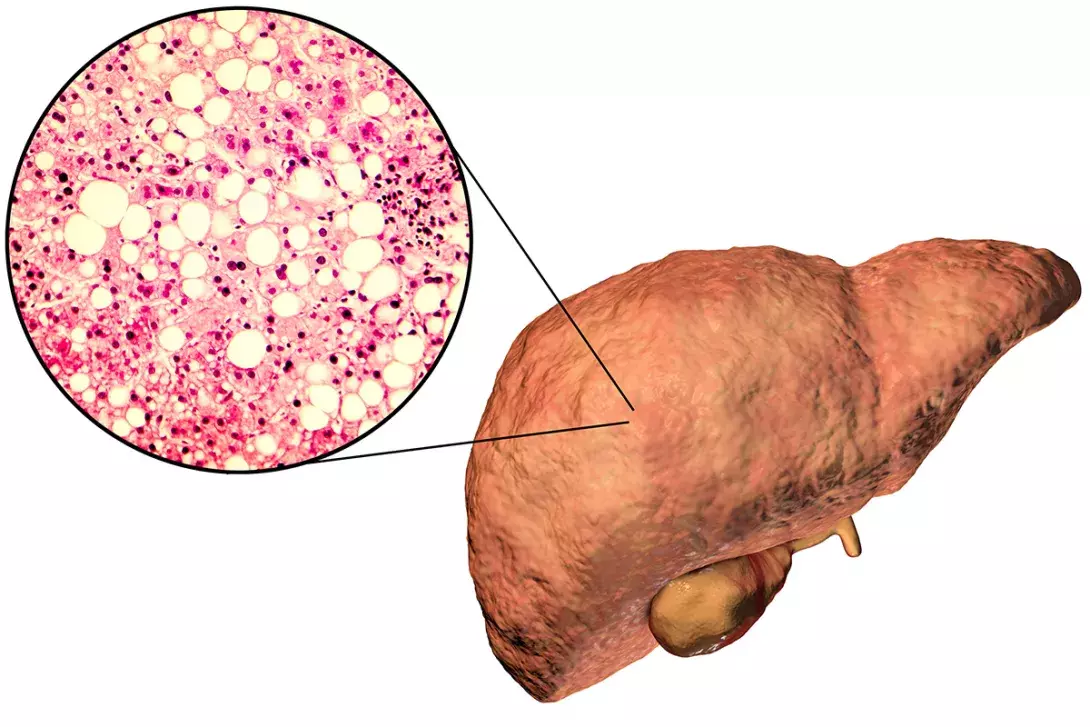
MAFLD, previously referred to as non-alcoholic fatty liver disease (NAFLD), is the most common cause of liver disease worldwide, with an estimated prevalence of 25%.1 MAFLD encompasses a disease continuum from simple fatty liver (steatosis) to steatohepatitis, with the latter projected to increase by 40% between 2019 and 2030 in Australia.2,3 MAFLD is a result of excessive lipid accumulation in the liver associated with metabolic dysregulation, and is associated with obesity, hypertension, dyslipidaemia, type 2 diabetes mellitus and insulin resistance.4 A positive diagnosis of MAFLD can be made in individuals with evidence of fatty liver in the setting of overweight/obesity, type 2 diabetes or in lean or normal weight individuals with at least two metabolic risk abnormalities.4
MAFLD is considered a standalone disease that can also occur with other concomitant liver diseases, whereas NAFLD was previously defined as the presence of steatosis in more than 5% of hepatocytes in the absence of significant alcohol consumption and other known causes of liver disease.
All patients with MAFLD should be assessed for the severity of fibrosis and the presence of extrahepatic associations, such as cardiovascular disease. Transaminase elevations are mild (usually less than five times the upper limit of normal) with an AST:ALT ratio of less than one, unless cirrhosis has supervened.5 Elevated GGT and ALP levels can also be seen. Radiographic findings most commonly include increased echogenicity on ultrasound. Noninvasive assessment with models such as the NAFLD Fibrosis Score or FIB-4, can be used to exclude significant fibrosis, along with liver stiffness measurement with elastography where available.6,7 Although liver biopsy remains the gold standard for diagnosis, it is seldom used unless the diagnosis remains unclear after noninvasive evaluation.
Once significant fibrosis is excluded, most patients with MAFLD can be managed in primary care. Currently there is no approved pharmacotherapy for MAFLD, with the cornerstone of treatment revolving around lifestyle intervention and correction of associated metabolic dysfunction. Lifestyle interventions include dietary modification aimed at reducing caloric intake and achieving a weight loss of at least 7 to 10%, and regular physical activity. Patients with advanced fibrosis or cirrhosis should be referred for specialist management. Cardiometabolic risk factors should be aggressively managed.
Alcoholic hepatitis and alcohol-related liver disease
Liver disease related to alcohol is a common but preventable cause of liver disease in Australia. It is recommended that all patients with liver disease in the context of heavy drinking undergo a fibrosis assessment and be counselled and supported to reduce alcohol consumption. Alcoholic hepatitis is an uncommon presentation of ALD and is characterised by the onset of jaundice and moderate elevations of AST levels that are greater than elevations of ALT levels, in patients with recent high-level alcohol consumption. Severe alcoholic hepatitis is associated with high short-term mortality.8 Scores, such as Maddrey’s Discriminant Function or the Model for End-Stage Liver Disease (MELD), can be used for prognostication.8
Abstinence from alcohol is the mainstay of treatment in patients with mild to moderate alcoholic hepatitis. Supportive care, including nutritional support and management of withdrawal symptoms, should be provided. Patients with severe alcoholic hepatitis or features of liver failure should be referred to hospital for specialist management including consideration of corticosteroids. Patients should be engaged in long-term abstinence support programs.
Drug- or toxin-induced liver injury
DILI is responsible for 3 to 5% of hospital admissions for jaundice and is the most frequent cause of acute liver failure in Western countries.9 It is estimated that DILI accounts for almost 10% of hospitalisations in Australia in patients with abnormal liver tests.10 Although paracetamol toxicity (either deliberate or accidental overdose) accounts for most DILI cases resulting in hospitalisation, cases related to herbal and dietary supplements are increasingly being recognised.11 Given the broad range of causative agents, a careful drug history must be taken to assess causality, including drugs that have been ceased in the last three months (typical latency period, although some exceptions occur).
DILI may present a diagnostic challenge with no diagnostic tests and a wide range of clinical presentations. Key features supporting its diagnosis include exclusion of other liver diseases, the latency period and the known likelihood of the drug to cause liver injury. Databases such as LiverTox® and tools such as the Roussel-Uclaf Causality Assessment Method (RUCAM) scale are widely used. In certain cases of acute or fulminant liver failure, a toxicology screen including paracetamol level or a urine drug screening for compounds such as ecstasy may be useful. Other than this, there is no role for the routine use of toxicology screen in DILI assessment. DILI can cause hepatocellular or cholestatic patterns of injury (Box 3).
Recovery occurs in most patients after withdrawal of the causative agent, and careful monitoring is sufficient until liver tests results normalise. Rechallenge with the causative drug is not recommended given the sometimes rapid and severe recurrence of liver injury. Acute or subacute liver failure may occur, and patients with no prior evidence of chronic liver disease who have ALT or AST levels greater than 10 times the upper limit of normal and jaundice or coagulopathy should be referred for hospital admission or urgent specialist review.
Biliary and pancreatic disorders
Biliary tract disorders, such as choledocholithiasis and cholangitis, are commonly encountered in primary care and may present with a hepatitis pattern of liver enzyme derangement. Patients present with right upper quadrant or upper abdominal pain, jaundice and/or fevers. Pancreatic disorders, such as pancreatitis or malignancy, may also cause biliary tract obstruction. Imaging, such as an abdominal ultrasound, should be performed to assess for cholelithiasis or a dilated biliary tree. Magnetic resonance cholangiopancreatography (MRCP) is another noninvasive method for assessment of the biliary tree, but costs may be prohibitive. Patients with these disorders often require referral to hospital for treatment with intravenous antibiotics and endoscopic or surgical intervention such as endoscopic retrograde cholangiopancreatography (ERCP) or cholecystectomy.
Autoimmune liver diseases
Autoimmune liver diseases represent uncommon and heterogeneous conditions that, if left untreated, may progress to cirrhosis. These diseases can be easily screened for in primary care, however specialist assessment and management is recommended.
Autoimmune hepatitis
Autoimmune hepatitis is a chronic inflammatory syndrome that can present at any age and is more common in women. It is a dynamic disease with varied clinical phenotypes, from acute hepatitis to cirrhosis or fulminant liver failure, and is a diagnosis that should always be considered when encountering elevated transaminase levels. Autoimmune markers that are commonly seen include antinuclear antibodies (ANA), smooth-muscle antibody (SMA) and liver-kidney microsomal antibodies (LKM). A liver biopsy is usually required to confirm the diagnosis and is recommended before treatment. Autoimmune hepatitis is a treatable disease, with the goals of immunosuppression to minimise inflammation and prevent progression to cirrhosis.12
Primary biliary cholangitis
Primary biliary cholangitis is an immune-mediated disease characterised by progressive destruction of small intralobular bile ducts, eventually leading to fibrosis and cirrhosis. It predominantly affects women (around 90% of cases) and is usually diagnosed between the ages of 40 and 50 years. Patients are often asymptomatic, however fatigue and pruritis may be seen. The liver enzyme pattern is usually cholestatic, with elevated serum ALP and GGT levels. Hyperbilirubinaemia may be seen late in the disease. Serum antimitochondrial antibodies (AMA) and antinuclear antibodies are positive in up to 95% and 70% of patients with the condition, respectively. Liver biopsy is not required for diagnosis; however, noninvasive fibrosis assessment is recommended. All patients diagnosed with primary biliary cholangitis are indicated for treatment with ursodeoxycholic acid, and second-line therapies are available for those with an incomplete biochemical response.13
Primary sclerosing cholangitis
Primary sclerosing cholangitis is a disorder characterised by multifocal bile duct strictures and progressive fibrosis, leading to end-stage liver disease. Patients may require liver transplantation given the lack of effective disease-modifying drugs. Primary sclerosing cholangitis is often associated with inflammatory bowel disease and patients are at increased risk of hepatobiliary and colorectal cancers. Cholestatic liver enzyme abnormalities are typically seen in patients with primary sclerosing cholangitis, and some have positive perinuclear antineutrophil cytoplasmic antibodies (p-ANCA). The diagnosis is established with cholangiography.14
Coeliac disease
Coeliac disease is a chronic multisystem immune disorder related to gluten intolerance. Occasionally patients with coeliac disease present with asymptomatic elevations of ALT and AST levels, and coeliac serology should be included in the evaluation of patients with mild to moderate transaminitis.15
Genetic disorders
Hereditary haemochromatosis
Hereditary haemochromatosis is a common autosomal recessive disorder, affecting one in 300 people in Australia. It is an iron storage disorder associated with inappropriately low levels of the hormone hepcidin. The low hormone levels lead to increased intestinal iron absorption and accumulation of the excess iron in tissues, eventually resulting in organ dysfunction (heart failure, diabetes and cirrhosis). Although hereditary haemochromatosis is usually identified on genetic testing after a finding of elevated serum ferritin with high transferrin saturation (greater than 45%), occasionally liver function tests may be abnormal (mild to moderate transaminase elevation). Management involves venesection to reduce iron levels as well as treatment of concomitant organ dysfunction if present.16
Wilson’s disease
Wilson’s disease is a rare genetic disorder characterised by excess copper accumulation due to a variety of mutations in the ATP7B gene. Patients most commonly present with liver disease, or, rarely, neuropsychiatric symptoms alone, and infrequently present over the age of 40 years. Transaminase levels are mild to moderately elevated with AST:ALT ratio greater than two, and the serum ceruloplasmin level is reduced, usually below 0.1 g/L. Other helpful tests include 24-hour urinary copper excretion, ocular examination for Kayser-Fleischer rings and liver biopsy. Management involves copper chelation agents or oral zinc, and patients should be referred for specialist management. Patients with acute liver failure usually require urgent liver transplantation.
Alpha-1 antitrypsin deficiency
Alpha-1 antitrypsin (A1AT) deficiency is due to mutations in the SERPINA1 gene, of which there are at least 150 alleles. The most common and normal allele is referred to as ‘M’; the ‘S’ allele produces moderately low levels of A1AT and the ‘Z’ allele produces very little A1AT. Heterozygous phenotypes of A1AT deficiency, such as MZ and SZ, are relatively common, and may be important cofactors in advanced liver disease of other causes, such as MAFLD or ALD.17 The homozygous (ZZ) phenotype of A1AT is associated with chronic obstructive pulmonary disease and cirrhosis.
Budd-Chiari syndrome
Budd-Chiari syndrome is a rare vascular disorder defined as hepatic venous outflow tract obstruction, independent of the mechanism, provided the obstruction is not related to cardiac disease, pericardial disease or sinusoidal obstruction syndrome.18 The clinical presentation varies widely from acute liver failure to chronic liver disease. The diagnosis may be suggested by doppler ultrasonography but usually requires invasive hepatic venography for confirmation.
Conclusion
With an increasing prevalence of nonviral liver disease, primary care physicians play an important role in the evaluation and management of these patients in the community. An accurate history, together with focused laboratory and radiological investigations, often yields the underlying aetiology. Red flags that indicate the need for urgent specialist review or hospitalisation include jaundice, prolonged INR, encephalopathy and ascites. MT
COMPETING INTERESTS: None.

