Actinic keratosis: an update on management

Actinic keratoses (AKs) are potentially premalignant cutaneous lesions that occur on chronically sun-exposed regions of the body. Left untreated, a small proportion of AKs will transform into invasive squamous cell carcinomas. It is important for GPs to be aware of the latest management practices for AKs, based on guidelines from Cancer Council Australia and the American Academy of Dermatology, so as to offer patients evidence-based treatment plans.
Note
The original version of this article was published in the May 2023 issue of Medicine Today. The version available here has been updated to more accurately reflect the use of and indications for the combination solution of 0.5% 5-FU and 10% salicylic acid.
- The presence of actinic keratoses (AKs) suggests significant ultraviolet (UV) exposure, which predisposes to development of all skin cancers. Patients should be educated about the importance of sun safety, as UV protection is associated with a reduced incidence of AKs.
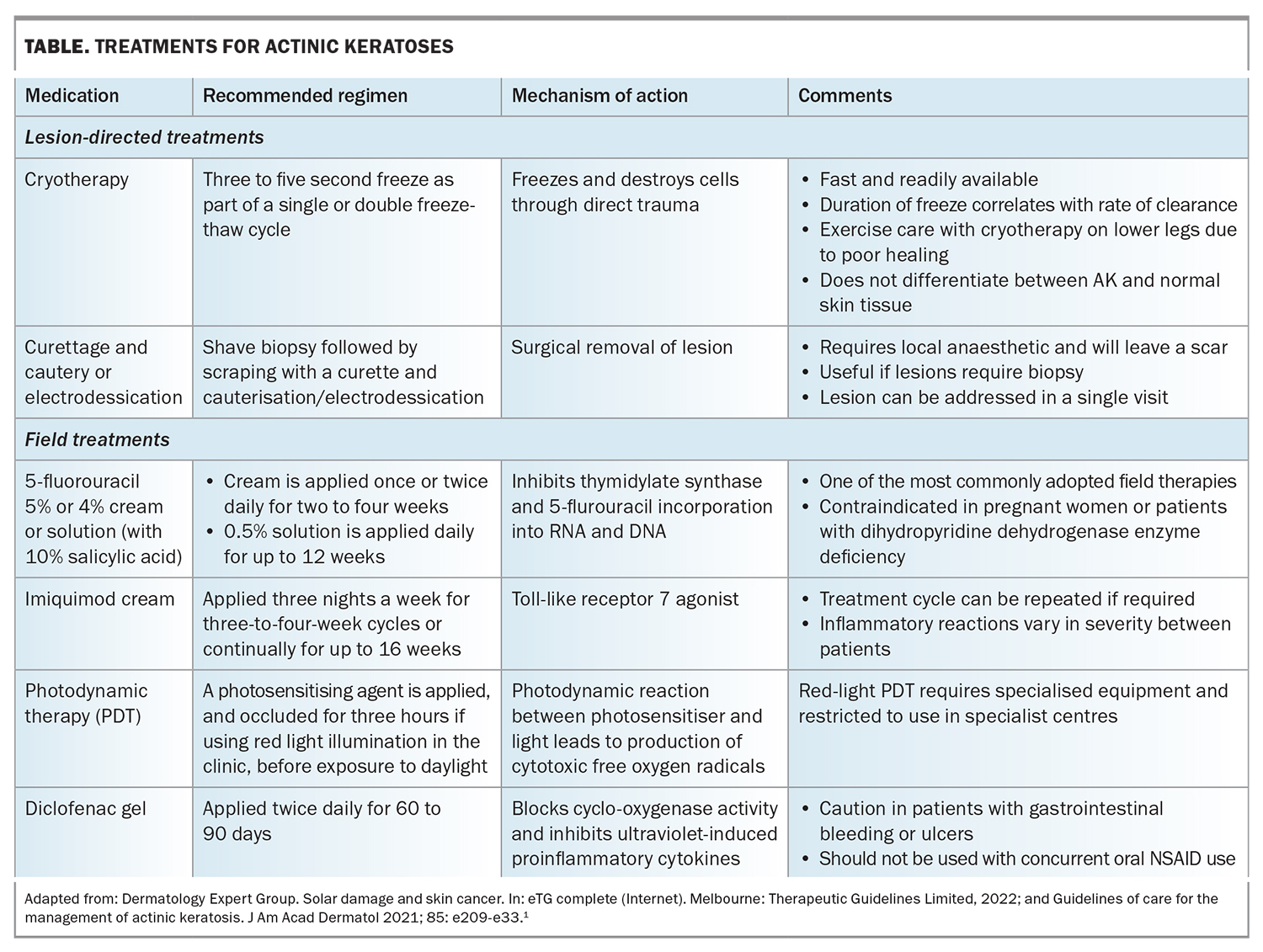
- Treatment for AKs is broadly classified as lesion-directed therapy, and includes cryotherapy or curettage and cautery, or field treatment, which includes topical and light-directed therapies.
- Cryosurgery is the recommended lesion-directed therapy, whereas 5-fluorouracil and imiquimod are the most effective field treatments.
- Photodynamic therapy involves application of either methyl aminolevulinate or 5-aminolevulinic acid, followed by light activation, either by red light for seven to nine minutes or continuous daylight for two hours.
- Ingenol mebutate is no longer considered a therapeutic option as it is associated with an increased incidence of skin cancers, and has been withdrawn from international markets.
- Tirbanibulin 1% ointment is a novel microtubule inhibitor that requires five days of treatment. It is currently under evaluation for approval by the TGA.
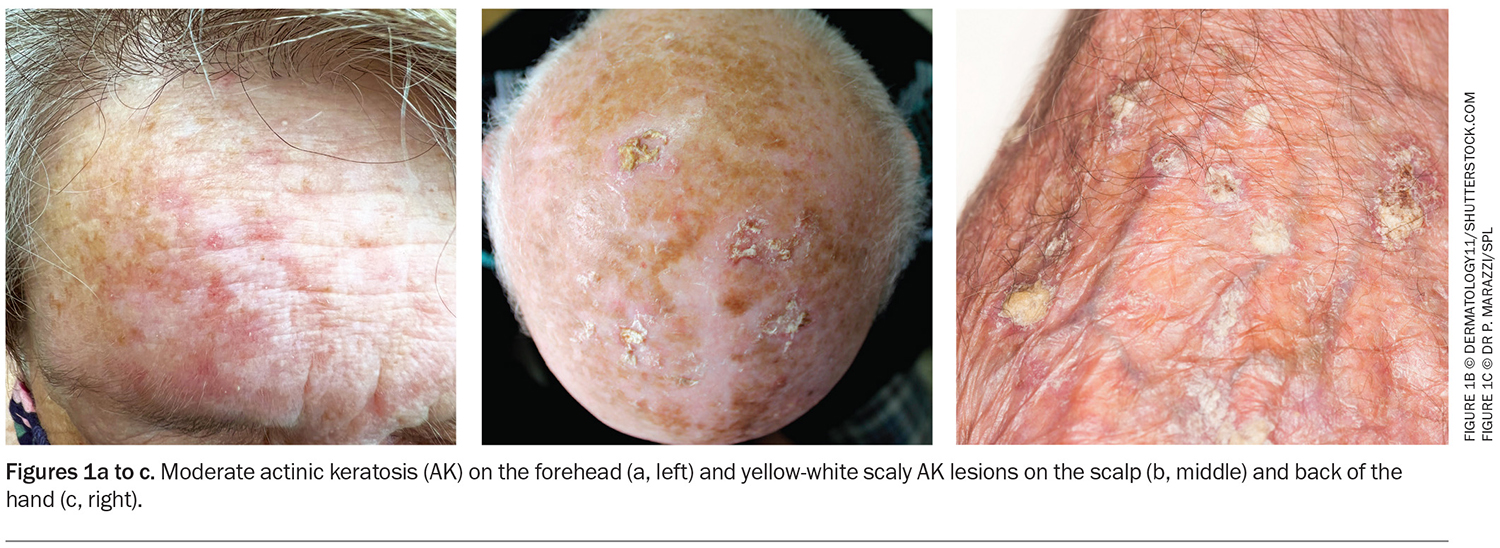
Actinic keratoses (AKs), sometimes referred to as solar keratoses, appear on sites of chronic ultraviolet (UV) radiation exposure. AKs most commonly occur on the face, scalp, dorsal aspect of the upper limbs and legs. They may occasionally produce excess keratin resulting in the formation of a keratotic horn. Lesions classically appear as yellow-white, scaly, rough, hyperkeratotic macules or papules overlying an erythematous base (Figures 1a to c). Generally, these lesions are neither tender nor indurated but have a rough texture. Palpation is thus an indispensable tool to differentiate between normal and sun-damaged skin, AK or squamous cell carcinoma (SCC). As the presence of AKs indicates considerable sun-induced damage, patients will likely have numerous lesions present, which may become confluent over a large field of sun-exposed skin.
Pathogenesis
Cumulative sun exposure causes damage to keratinocytes, which leads to changes in genetic structure. In AK, abnormal keratinocytes are confined within the epidermis; however, have the potential to progress to full-thickness epidermal dysplasia. Once this occurs, there may be progression from AK to keratinocyte carcinoma, which usually requires definitive management.
Currently, no clinically defining features determine whether an AK lesion will progress to SCC and it is therefore difficult to predict and specifically target ‘higher-risk AK lesions’. To date, estimates of progressions from AK to SCC vary between 0.1 to 20%.1 Therefore, it is pertinent to recognise and consider treatment for AKs, as they are all potential precursors of SCC. An area of skin with numerous AKs can indicate a region of field cancerisation. This concept refers to the presence of subclinical precancerous lesions near the vicinity of visible AK lesions that have been affected by the same amount of UV radiation despite a normal outward appearance.2
Patients with long-term exposure to UV radiation, fair skin, a history of severe sunburns and those taking photosensitising medications are at a higher risk for developing AKs. Clinicians should be mindful of patients who are immunosuppressed, such as patients receiving organ transplant and those with chronic lymphocytic leukaemia, as the development of AKs and the process of progression may be accelerated.
Role of the GP
Due to its geographical location and high levels of UV radiation exposure, Australia has one of the highest rates of AK development in the world.3 As highlighted above, recognition and management of AKs are important because of the risk of progression to SCC. The presence of an AK is proof of significant UV light exposure. As a result, patients with AKs are at a higher risk of developing all skin cancers, and management not only involves treating the AK lesions, but also conducting regular skin examinations.
Although diagnosis of AKs is primarily clinical in nature, a biopsy should be considered if there are concerns regarding malignancy. Caution should be exercised when approaching an AK that is bleeding, ulcerated, tender, heavily indurated, nodular in appearance or refractory to treatment, as it may suggest that the AK has already progressed into a keratinocyte carcinoma. Referral to a dermatologist is recommended for patients who are immunosuppressed, have widespread and severe actinic damage and require further management of lesions that are suspected to be keratinocyte carcinomas, or for younger patients with more AKs than expected.
Updates on management
Numerous effective treatments are currently available for AKs (Table). Careful consideration of the lesion (number, distribution, size), patient factors (pain tolerance, compliance to therapy, cosmetic considerations, cost), treatment side effects (tolerability) and rate of recurrence should be taken into account when deciding on the appropriate treatment. Shared decision making on the treatment approach is important as it will increase compliance and the ability to tolerate localised skin reactions. These reactions may cause early termination of treatment before the therapeutic outcome is achieved. Treatment for AKs is largely based on Cancer Council Australia’s Clinical practice guidelines for keratinocyte cancer (https://wiki.cancer.org.au/australia/Guidelines:Keratinocyte_carcinoma), and is also informed by the American Academy of Dermatology (ADD) Guidelines of care for the management of actinic keratosis.1
Treatment can be broadly classified as lesion-directed, which targets discrete lesions, or field treatment, which targets a larger area of skin containing multiple AKs. The prevailing consensus favours field treatment as it has the potential to concurrently treat subclinical lesions. Studies have shown that general UV protection and sunscreen is associated with a reduction in the development of new AKs and, therefore, all patients should be educated, with emphasis on the importance of ongoing sun protection, as part of their management plan.4,5
Lesion-directed treatment
Cryosurgery
Liquid nitrogen cryotherapy is a commonly performed procedure for the treatment of AKs. Dermatologists strongly recommend the use of cryotherapy for discrete AKs as it is fast, readily available and efficacious.1 The duration of the freeze time tends to parallel response rates, and general consensus suggests three to five seconds as part of a single or double freeze-thaw cycle.6 Patients should be warned that the lesion will swell due to oedema and may blister, and of the risk of hypopigmentation, especially patients with darker skin types.7 Clinicians may prefer this approach as it is low cost and does not require patient compliance or local anaesthetic. It should be noted that cryotherapy does not preferentially destroy diseased skin, and resolution rates are reported to range between 57 and 98.8%.8-12
Curettage and cautery/electrodessication
For lesions that are above average thickness or suspicious, curettage and cautery or electrodessication may be a useful modality as the initial shave biopsy can provide a specimen for histological assessment if diagnosis is uncertain. The area should then be scraped with a curette and cauterised to ensure the lesion is adequately treated. Patients should be warned that this technique will likely leave a scar and of the risk of wound infection and hypopigmentation.7 It is essential to note that only operators who have received appropriate training should conduct this therapy.
Field treatment
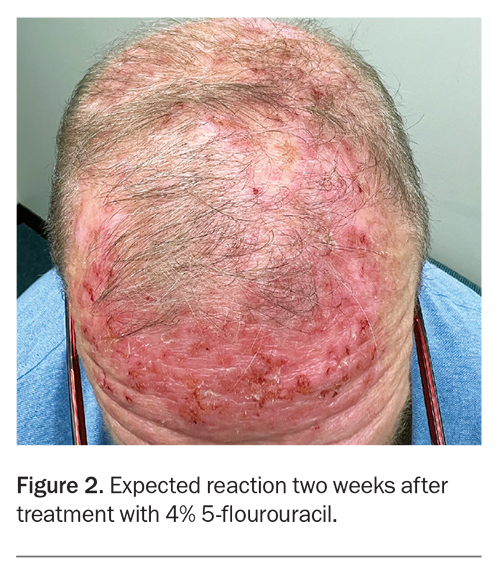
Treatment of field cancerisation is especially advantageous in patients with high density AKs or lesions without distinct borders for which localised therapy is undesirable. This management approach is favourable as seemingly healthy skin in the vicinity of AK lesions is theoretically affected by the same amount of UV radiation-induced damage and may contain precancerous keratinocytes, despite a normal outward appearance. Field therapy is usually topical in nature and relies heavily on patient compliance to achieve desirable therapeutic outcomes. Inflammatory reactions, such as erythema, soreness, erosions and crusting, are to be expected and are necessary to treat the atypical keratinocytes present (Figure 2). Patients should be educated about the importance of these reactions and their expectations managed to avoid poor adherence and subsequent poor outcomes. A range of therapies with varying treatment durations are currently available; however, those with the shortest treatment duration may be preferred by some patients.
5-fluorouracil
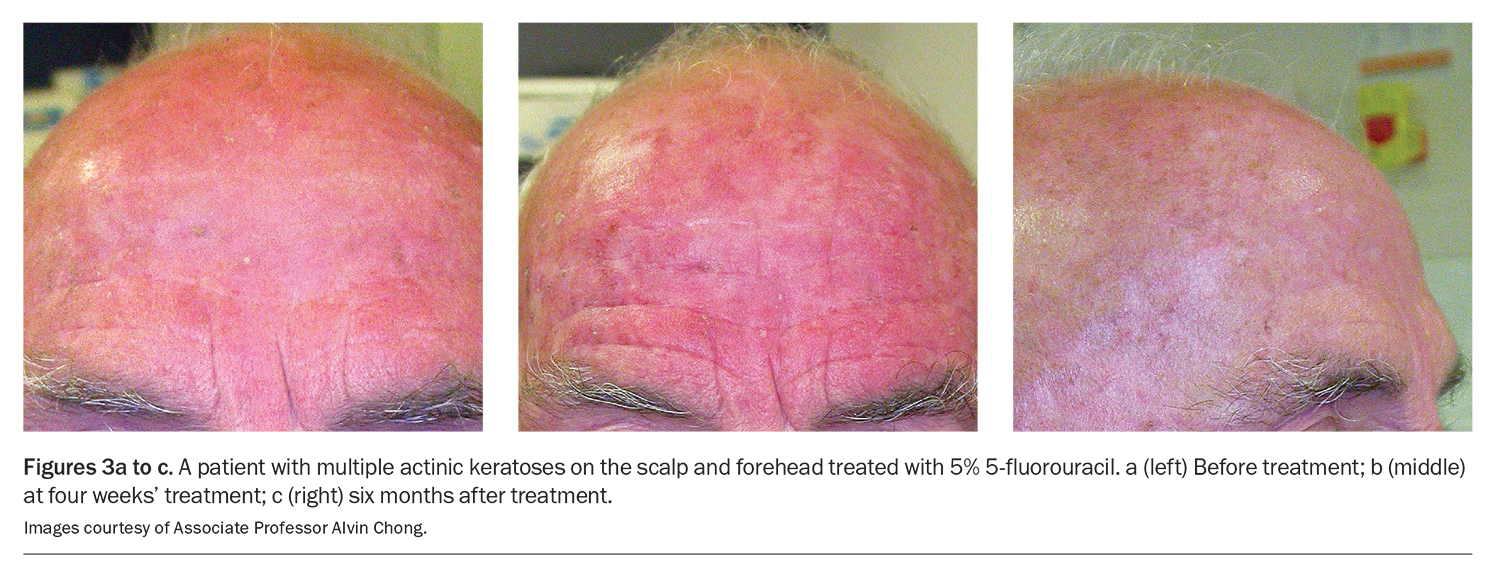
5-fluorouracil (5-FU) is a topical cytotoxic agent and is available in Australia as 5% and 4% creams and a 0.5% solution (also containing 10% salicylic acid). It inhibits both DNA and RNA synthesis in rapidly dividing cells, leading to apoptosis. There is preferential uptake in rapidly dividing cells and, therefore, it is selective for atypical cells. The AAD strongly recommends the use of 5-FU for field treatment of AKs, based on current available evidence.1 Some clinicians may even use 5-FU to identify subclinical AKs before staring cryotherapy.13 It is recommended that a thin layer of 5-FU cream is applied once or twice daily for two to four weeks, or for as long as a patient can tolerate (Figures 3a to c). A combination of 0.5% 5-FU and 10% salicylic acid solution is available; it is indicated for lesion and/or small field (<25 cm2) therapy, and is used once daily for up to 12 weeks.14 We advise this as a regular (every few years) winter time activity for high risk individuals and patients should be warned that localised irritation is to be expected.
Imiquimod
Imiquimod is an immune response modifier that activates toll-like receptor 7. The AAD strongly recommends the use of various concentrations of imiquimod for the field treatment of AKs.1 Imiquimod 5% cream is approved by the TGA for the treatment of AKs, specifically on the face and scalp. Application regimens can be three times a week in four-week cycles or consecutively for up to 16 weeks, in accordance with patient preference.
Photodynamic therapy
Photodynamic therapy (PDT) uses the application of a topical photosensitiser, either methyl aminolevulinate (MAL) or 5-aminolevulinic acid (5-ALA) and light activation to cause a photodynamic reaction, leading to the production of cytotoxic oxygen free radicals. A 1 mm layer of cream is applied onto the area under an occlusive dressing for three hours. The area is then wiped clean and illuminated by red light for seven to nine minutes in the clinician’s office.15 Alternatively, after application of MAL or 5-ALA, patients can immediately expose the treated area to daylight for two continuous hours.
A single treatment is recommended, with results assessed at three months and a second treatment needed only if residual lesions remain.15 The former method is sometimes favoured by clinicians, as it does not rely on patient compliance. Daylight PDT is less painful and can be performed all year round. It has been found to be equally as effective but less painful than red-light PDT when 5-ALA is used.1 Red-light PDT may require the use of anaesthetic and is only available at practices with the appropriate equipment and trained staff.
Diclofenac
Diclofenac sodium gel 3% is thought to induce cell death and inhibit cell proliferation in AKs. Currently, the AAD conditionally recommends the use of diclofenac based on lower quality evidence.1 It should be applied twice daily for 60 to 90 days to achieve effect. Diclofenac should be used with caution in patients with a history of gastrointestinal bleeding or ulceration. It should not be used in patients who are concurrently receiving oral NSAIDs for other health conditions.
Chemoprophylaxis for immunosuppressed patients
Patients who are immunosuppressed, especially those who have received solid organ transplants, have a higher risk of developing keratinocyte cancer. It is therefore important for these patients to use adequate sun protection and undergo regular skin checks. Systemic chemoprevention with low-dose acitretin has been found to be efficacious in this group of patients.16 Although it was previously thought that nicotinamide could be used as a form of chemoprophylaxis, the current evidence is inconclusive.17
Tirbanibulin
Tirbanibulin 1% ointment is a novel microtubule inhibitor that induces expression of p53 and causes apoptosis in rapidly dividing cells.1,18 Phase 3 clinical trials have shown a complete clearance rate ranging from 44 to 54%. The treatment regimen is short, consisting of daily application for five days and is therefore preferred by some patients. Among treated patients, rates of recurrence at one year were higher at 47% compared with 5-FU- or imiquimod-treated patients.18 Most trial patients were Caucasian with Fitzpatrick skin types I and II, which should be considered when interpreting the results.17 Further research is needed on the long-term side effects. Tirbanibulin is currently contraindicated in pregnancy and women who are breastfeeding due to lack of data. Tirbanibulin has been approved by the US Food and Drug Administration and is under evaluation for approval in Australia by the TGA.19
Discontinuation of ingenol mebutate
Ingenol mebutate gel was first introduced in 2012 as an efficacious, short duration treatment for AKs. Its mechanism of action is believed to have been neutrophil-mediated immunostimulatory effects, leading to apoptosis of dysplastic cells. Its use has since been found to increase the incidence of nonmelanocytic skin cancer in areas of treated skin and has been withdrawn from the market and will be permanently discontinued worldwide. Thus, ingenol mebutate is not recommended for the treatment of AKs.1
Conclusion
AKs are caused by chronic UV radiation damage and are precursors to keratinocyte cancer. Treatment can be lesion directed or field directed. Currently, there is strong evidence to recommend cryotherapy for lesion-directed therapy and topical 5-FU and imiquimod for field treatment. Novel medications, such as tirbanibulin, are being developed but should be used with caution until data from long-term trials are available. MT
COMPETING INTERESTS: Dr Wong: None. Associate Professor Shumack reports consultation fees and honoraria from Aspen Medical Australia.
References
1. Eisen DB, Asgari MM, Bennett DD, et al. Guidelines of care for the management of actinic keratosis. J Am Acad Dermatol 2021; 85: e209-e233.
2. Stockfleth E. The importance of treating the field in actinic keratosis. J Eur Acad Dermatol Venereol 2017; 31: 8-11.
3. See JA, Shumack S, Murrell DF, et al. Consensus recommendations on the use of daylight photodynamic therapy with methyl aminolevulinate cream for actinic keratoses in Australia. Aus J Dermatol 2016; 57: 167-174.
4. Green A, Williams G, Nèale R, et al. Daily sunscreen application and betacarotene supplementation in prevention of basal-cell and squamous-cell carcinomas of the skin: a randomised controlled trial. Lancet 1999; 354: 723-729.
5. Naylor MF, Boyd A, Smith DW, Cameron GS, Hubbard D, Neldner KH. High sun protection factor sunscreens in the suppression of actinic neoplasia. Arch Dermatol 1995; 131: 170-175.
6. Thai KE, Fergin P, Freeman M, et al. A prospective study of the use of cryosurgery for the treatment of actinic keratoses. Int J Dermatol 2004; 43: 687-692.
7. Foley P, Shumack S, Goh M, Moreno G; Cancer Council Australia Keratinocyte Cancers Guideline Working Party. Guidelines: Keratinocyte carcinoma/Cryotherapy, curettage and diathermy. In: Clinical practice guidelines for keratinocyte cancer. Cancer Council Australia: Sydney, 2019. Available online at: https://wiki.cancer.org.au/australiawiki/index.php?oldid=208353 (accessed May 2023).
8. Foley P, Merlin K, Cumming S, et al. A comparison of cryotherapy and imiquimod for treatment of actinic keratoses: lesion clearance, safety, and skin quality outcomes. J Drugs Dermatol 2011; 10: 1432-1438.
9. Freeman M, Vinciullo C, Francis D, et al. A comparison of photodynamic therapy using topical methyl aminolevulinate (Metvix®) with single cycle cryotherapy in patients with actinic keratosis: a prospective, randomized study. J Dermatolog Treat 2003; 14: 99-106.
10. Ianhez M, Miot HA, Bagatin E. Liquid nitrogen for the treatment of actinic keratosis: a longitudinal assessment. Cryobiol 2014; 69: 140-143.
11. Lubritz RR, Smolewski SA. Cryosurgery cure rate of actinic keratoses. J Am Acad Dermatol 1982; 7: 631-632.
12. Szeimiesa R, Karrera S, Radakovic-Fijanb S, et al. Photodynamic therapy using topical methyl 5-aminolevulinate compared with cryotherapy for actinic keratosis: a prospective, randomized study. J Am Acad Dermatol 2002; 47: 258-262.
13. Johnson TM, Rowe DE, Nelson BR, Swanson NA. Squamous cell carcinoma of the skin (excluding lip and oral mucosa). J Am Acad Dermatol 1992; 26: 467-484.
14. Australian product information. ACTIKERALL (fluorouracil and salicylic acid) solution. Available online at: https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2021-PI-01886-1 (accessed May 2024).
15. Foley P, Shumack S, Goh M, Moreno G; Cancer Council Australia Keratinocyte Cancers Guideline Working Party. Guidelines: Keratinocyte carcinoma/Photodynamic therapy. In: Clinical practice guidelines for keratinocyte cancer. Cancer Council Australia: Sydney, 2019. Available online at: https://wiki.cancer.org.au/australiawiki/index.php?oldid=208347 (accessed May 2023).
16. Tee LY, Sultana R, Tam SY, Oh CC. Chemoprevention of keratinocyte carcinoma and actinic keratosis in solid-organ transplant recipients: systematic review and meta-analyses. J Am Acad Dermatol 2021; 84: 528-530.
17. Allen NC, Martin AJ, Snaidr VA, et al. Nicotinamide for skin-cancer chemoprevention in transplant recipients. N Engl J Med 2023; 388: 804-812.
18. Blauvelt A, Kempers S, Lain E, et al. Phase 3 trials of tirbanibulin ointment for actinic keratosis. N Eng J Med 2021; 384: 512-520.
19. Therapeutic Goods Administration. Prescription medicines under evaluation, KX-01 Seqirus Pty Ltd. TGA; Canberra, 2022. Available online at: https://www.tga.gov.au/resources/prescription-medicines-under-evaluation/kx-01-seqirus-pty-ltd (accessed May 2023).