An update on long COVID and its management

Long COVID is a multisystemic condition affecting five to 20% of individuals after SARS-CoV-2 infection. Although there is no cure, GPs can effectively support patients by managing symptoms, providing education and co-ordinating care. Evidence of the long-term health impacts, pathophysiology and potential treatments is rapidly evolving.
To date, over 11 million cases and 20,000 deaths from COVID-19 have been reported in Australia.1 However, the true number of cases is likely higher, as seroprevalence surveys suggest over two-thirds of people in Australia had been infected with SARS-CoV-2 by December 2022.2 Some patients continue to experience persistent symptoms of a physical, psychological or cognitive nature following SARS-CoV-2 infection. Evidence suggests this post-COVID-19 condition, commonly known as long COVID, poses a significant healthcare burden that will likely continue into the future.
This article discusses the clinical presentations of long COVID, its pathophysiology, epidemiology and prognosis. A summary of long COVID management is presented, outlining the role of the GP, red flag symptoms and when to refer.
Definition of long COVID
In 2021, the WHO proposed a definition for long COVID, or the post-COVID-19 condition, that encompassed persistent symptoms occurring in individuals with probable or confirmed SARS-CoV-2 infection, usually three months from the onset of COVID-19 and lasting for at least two months, with no alternative diagnosis.3 Common symptoms include fatigue, shortness of breath and cognitive dysfunction; however, systematic reviews have associated over 100 symptoms affecting a wide range of organ systems.4,5 Symptoms may be new-onset following initial recovery from acute SARS-CoV-2 infection, or persist from initial illness. They frequently interfere with everyday functioning (including activities of daily living and employment) and may also fluctuate or relapse over time.
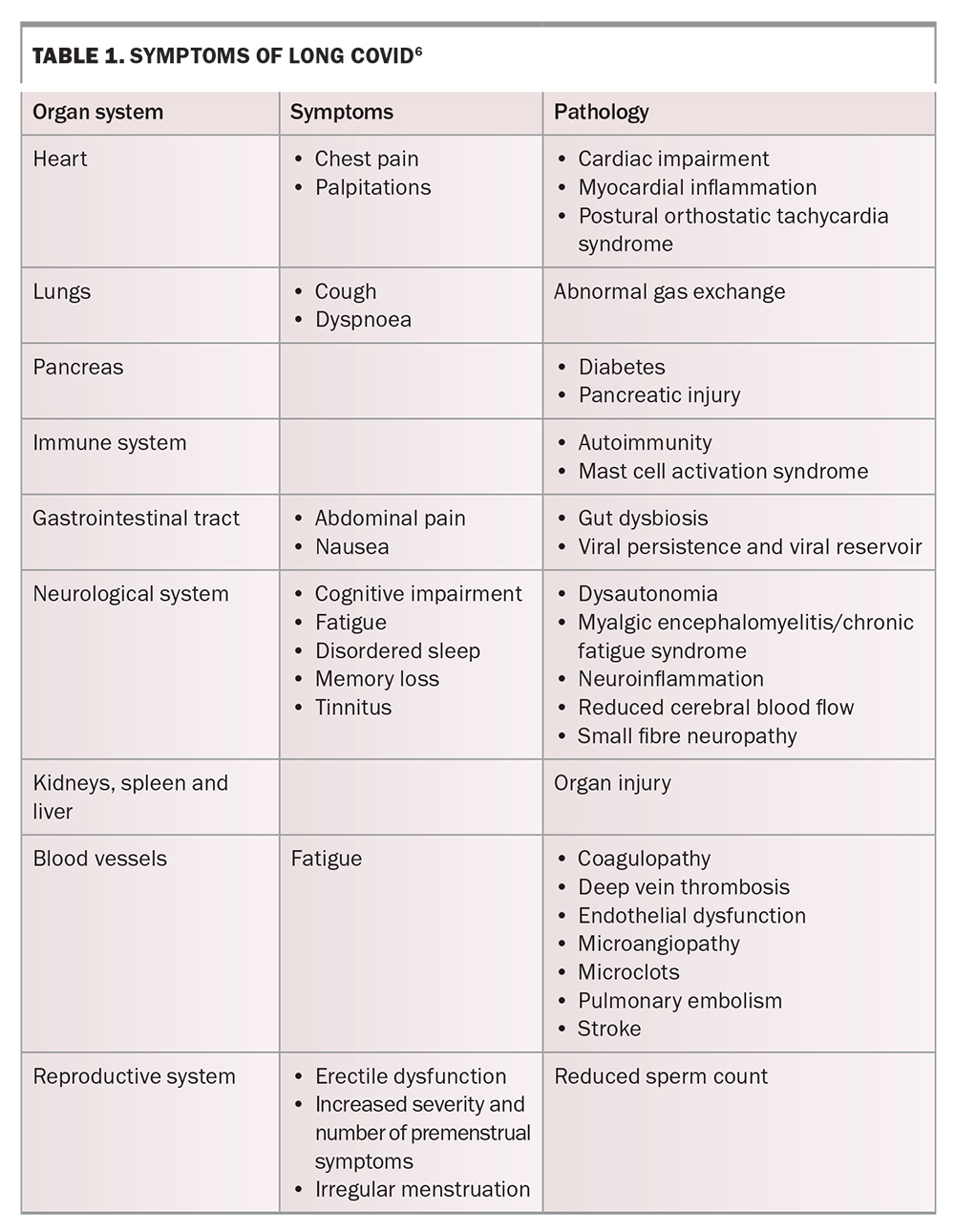
Clinical presentation
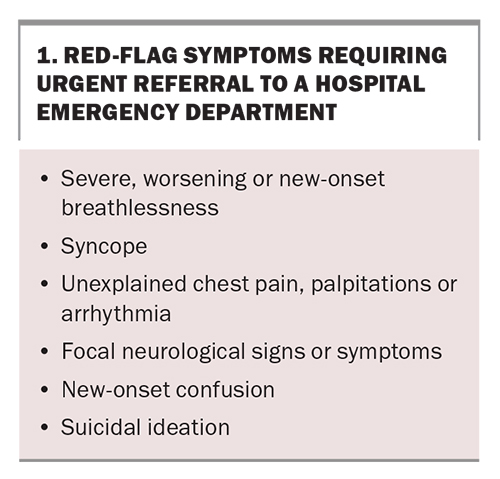
Long COVID is characterised by a wide constellation of symptoms affecting multiple organ systems (Table 1).6 Symptoms may be general, such as fatigue, post-exertional malaise and myalgia, or organ specific. Sequelae affecting the cardiorespiratory system may manifest with dyspnoea, cough, chest pain or palpitations, whereas sequelae affecting the neurological system often feature insomnia, headache, dizziness, cognitive impairment (typically reported as ‘brain fog’) and smell and taste dysfunction. Red-flag symptoms that require urgent referral to a hospital emergency department are listed in Box 1.
Patients’ symptoms tend to be characterised by at least one of three phenotypes or symptom clusters. A primary care-based study of electronic medical records from 486,149 nonhospitalised patients described three symptom clusters:7
- ‘fatigue’ cluster (80% of patients) encompassing a wide range of symptoms such as fatigue, headache, chest pain, palpitations, abdominal pain and hair loss
- ‘cognitive’ cluster (14% of patients) including symptoms of brain fog, insomnia, anxiety and depression
- ‘respiratory’ cluster (6% of patients) including symptoms of cough, breathlessness and wheeze.
It should be emphasised that these clusters are not mutually exclusive, and many patients have multiple symptoms that do not necessarily fit into one cluster type.
Cardiovascular autonomic abnormalities, such as initial orthostatic hypotension (IOH) or postural orthostatic tachycardia syndrome (POTS), are common.8 Although both forms manifest with symptoms of orthostatic intolerance, IOH is characterised by a transient drop in systolic (≥40 mmHg) or diastolic (≥20 mmHg) blood pressure within 15 seconds of standing, whereas POTS is classified by an excessive heart rate over 120 bpm, or an increase of 30 bpm or more within ten minutes of standing and in the absence of orthostatic hypotension.
Other manifestations, such as organising pneumonia, interstitial lung abnormalities and postintensive care syndrome, appear more frequently following hospitalisation for severe illness. Post-COVID pulmonary fibrosis is characterised by pulmonary function abnormalities and findings on CT such as parenchymal bands, ground-glass opacities and consolidation.9 Postintensive care syndrome encompasses multidimensional impairments in cognitive, mental, physical and social function.10
Pathophysiology
No one mechanism has been clearly associated with long COVID and it is likely that several different mechanisms are responsible for different phenotypes.11 The pathophysiology of long COVID after community-managed initial infection may also have differences compared with abnormal recovery after severe initial infection. Multiple inflammatory mechanisms have been proposed as a common pathophysiology. Two leading hypotheses include:
- viral antigen persistence causing a sustained inflammatory response
- formation of microclots causing multiorgan dysfunction.
Delayed viral antigen clearance or possibly active viral reservoirs within the body may provoke chronic
low-grade inflammation, autoimmunity, coagulation and fibrosis pathway activation and metabolic disturbances.11 One study found 65% of participants with long COVID had detectable levels of SARS-CoV-2 spike protein in their plasma up to 12 months after infection.12 Another study found combinations of proinflammatory cytokines, including interferon-beta, interferon-gamma and interleukin-6, persisted up to eight months after infection and their presence predicted long COVID with about 80% accuracy.13
The hypothesis for the microclot mechanisms, which is awaiting further experimental validation, is that proteins within SARS-CoV-2 trigger the formation of amyloid fibrin-microclots, which inhibit the transport of red blood cells to capillaries, reducing oxygen transport to tissues.
Epidemiology
Prevalence
The diversity of study populations and methodologies has introduced bias and led to challenges in accurately determining the prevalence and natural history of long COVID. A recent meta-analysis showed that unresolved symptoms occurred in 35% of community-managed patients and 53% of hospitalised patients four months after infection.14 However, many of the included studies did not include matched controls nor did they account for pre-existing symptoms. Prospective studies that included matched controls have suggested prevalence estimates of 12%, 13% and 38%.15-17
The Office for National Statistics in the UK inform our best estimates of long COVID prevalence in the postvaccine Omicron era. They found 4% of adults and 1% of children reported having long COVID 12 to 20 weeks after initial SARS-CoV-2 infection.18 Vaccination was associated with a 29% lower risk of developing long COVID in one meta-analysis.19 Similarly, the prevalence of long COVID following infection with the Omicron variant was about half that of earlier variants.20,21
Risk factors
The REACT-2 study (n = 606,434) found that the severity of initial COVID-19 illness and hospitalisation carried the highest odds ratio for developing long COVID. In addition, the study found female sex, obesity, advanced age, smoking and low socioeconomic status were also significantly associated with long COVID.17 Observational studies have consistently shown that women are more susceptible than men to developing long COVID, which may be because of differences in antiviral and autoimmune responses between the sexes.22-24 The association between obesity and long COVID is less clear, with a potential explanation being an increase in the expression of angiotensin-converting enzyme 2 in adipocytes, proinflammatory cytokines and immune dysfunction associated with insulin and leptin resistance.25 Other risk factors for developing long COVID include immunosuppression and comorbidities such as COPD, asthma and anxiety and depression.7
Treatment
Currently, no pharmacotherapies are approved for the treatment of long COVID. Numerous studies are underway to investigate potential drug therapies such as antivirals, HMG-CoA reductase inhibitors (statins), anticoagulants and immunosuppressants. Results from two large, randomised controlled trials investigating nirmatrelvir/ritonavir for the treatment of long COVID are expected by January 2024.26,27 Primary prevention with early treatment of acute infection may be beneficial. One study demonstrated that treatment with nirmatrelvir within five days of COVID-19 diagnosis was associated with a 26% less risk of long COVID sequelae and 47% less risk of post-acute death among participants with at least one risk factor for severe illness.28 The STIMULATE-ICP randomised trial is currently underway to evaluate the use of multiorgan MRI and a digitally enabled rehabilitation platform, in addition to pharmacotherapies such as colchicine, rivaroxaban and loratadine plus famotidine.29
Diagnosis
It is important to establish the timing of persistent symptoms in relation to the date of initial infection (preferably a confirmed SARS-CoV-2 diagnosis). If SARS-CoV-2 testing was not undertaken, a history consistent with COVID-19 infection may be sufficient to diagnose long COVID – even among patients with initially mild infective symptoms.
It is abnormal for almost any viral respiratory illness to cause persistent symptoms beyond one month. GPs may suspect long COVID in patients presenting with persistent, particularly disabling symptoms one month after COVID-19 infection, and are encouraged to initiate investigations early. Studies suggest only a small proportion of patients recover fully between one and three months postinfection (about 20% in the REACT-2 cohort).17
Given the lack of definitive biomarkers, long COVID remains a diagnosis of exclusion and it is important to consider alternative illnesses or coexisting pathologies that may present with similar symptoms. Initial investigations are ideally undertaken in primary care as GPs often have excellent knowledge of their patients’ comorbidities and baseline test results.
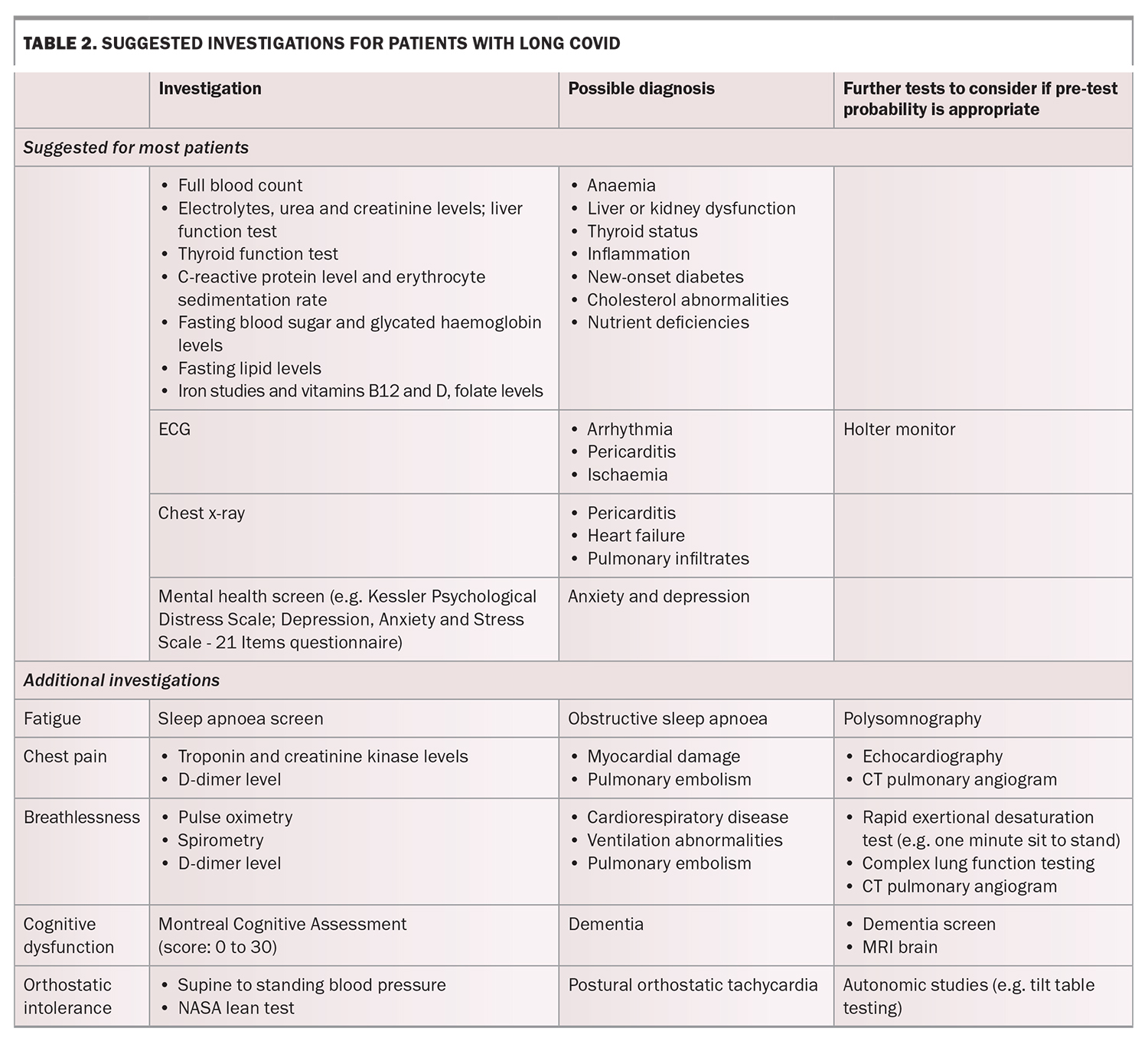
Investigations
The history and examination will guide which investigations are appropriate for each patient (Table 2). Most patients should receive blood tests to identify anaemia, electrolyte abnormalities, kidney and liver dysfunction, lipid abnormalities, thyroid dysfunction, diabetes, nutritional deficiencies and inflammatory markers. An electrocardiogram (ECG) and chest x-ray are helpful to rule out serious conditions. Further complex investigations may be considered depending on the clinical presentation (e.g. echocardiogram, lung function tests, MRI brain).
Management
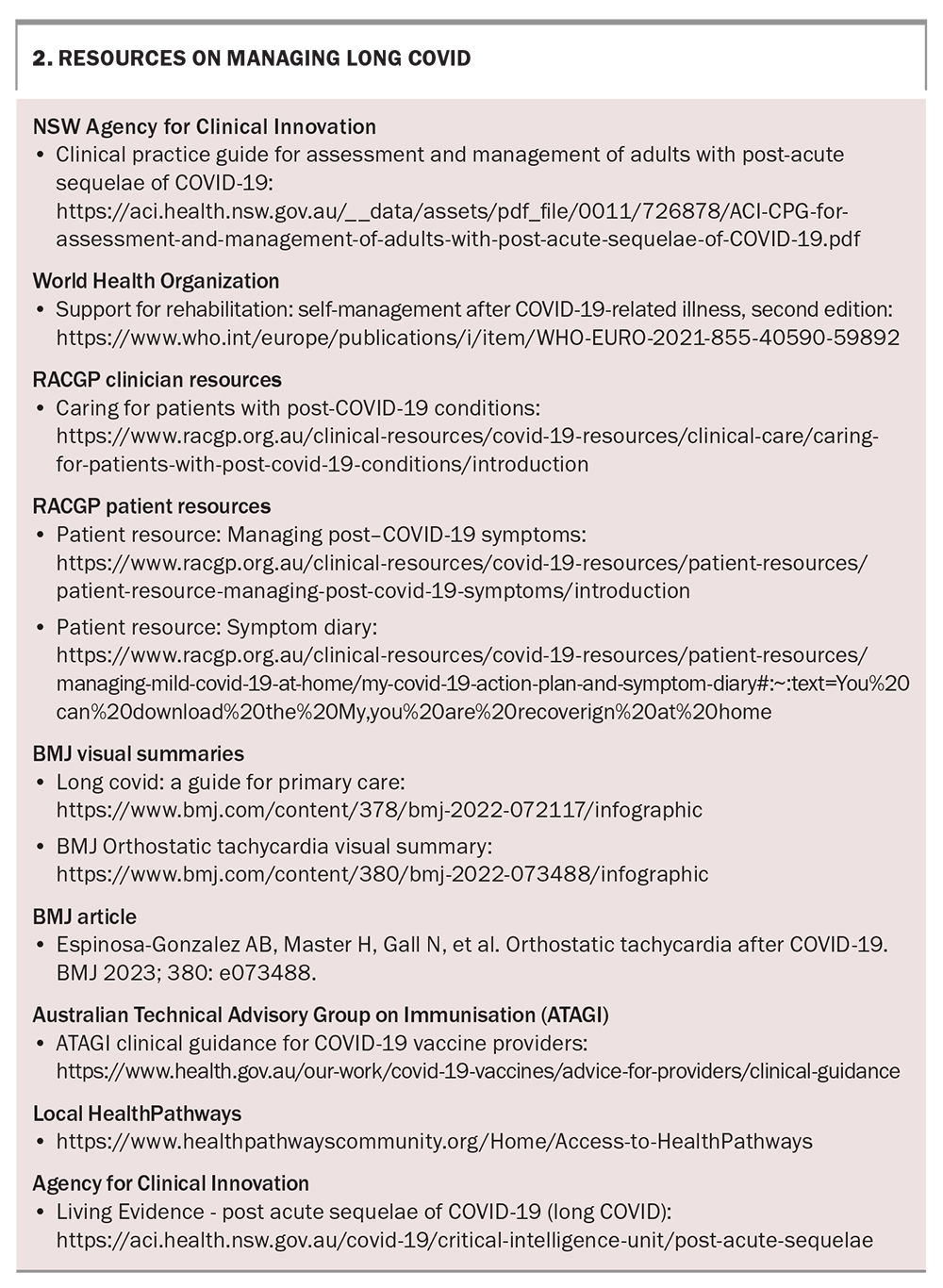
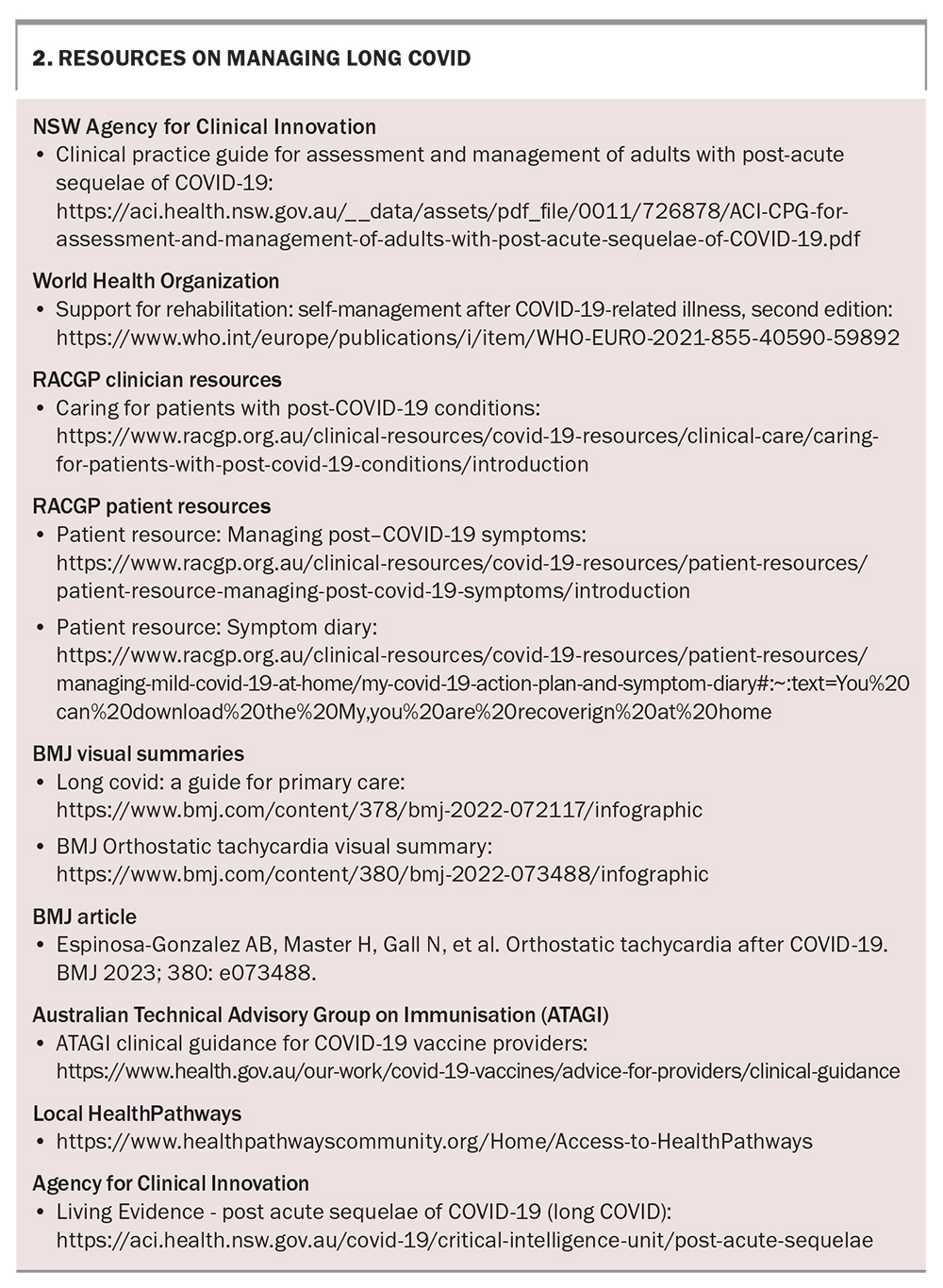
After excluding alternative pathology, management of long COVID usually involves controlling symptoms, optimising comorbidities, preventing reinfection and counselling. Box 2 provides useful information and resources on managing long COVID.
Symptom control
Patients are often required to adjust to a new baseline level of physical and mental activity to prevent relapse. The WHO’s Support for Rehabilitation: Self-Management after COVID-19 Related Illness report details multiple strategies to control symptoms, such as energy conservation or breathing techniques, and is an excellent resource for patients. Evidence also supports the use of supervised, tailored exercise programs, even among patients with initially mild COVID-19 illness.30 One small randomised controlled trial demonstrated greater improvements in quality of life, cardiovascular fitness and muscle strength among participants who underwent an eight-week exercise program compared with those assigned self-management rehabilitation recommendations alone.31
Optimising comorbidities
Sleeping difficulties, life stressors and comorbidities, such as cardiorespiratory or musculoskeletal disorders, play a large role in mediating health-related quality of life among patients with long COVID.32-34 Optimisation of comorbidities and lifestyle factors is likely to be beneficial.
Preventing reinfection
The Veterans Affairs study found that multiple COVID-19 infections were associated with cumulatively worse health outcomes and all-cause mortality.35 Although causality cannot be inferred, it is sensible to limit patients’ risk of repeat infections – consider vaccination, indications for antivirals and a COVID-19 action plan among high-risk patients. Vaccination may be delayed for three to six months after COVID-19 infection and we suggest following ATAGI recommendations for further vaccine scheduling (Box 2). Administering further doses of a COVID-19 vaccine to patients with ongoing long COVID may exacerbate symptoms, although most patients (75% in one meta-analysis) report either no change or improvement in symptoms.36
Counselling
Patients with long COVID require a nuanced and compassionate approach to care. Since many investigations will return normal results, patients may experience disbelief or stigma by their communities. Providing reassurance and education and addressing the uncertainties of prognosis can be a large focus of the consultation.
When to refer
For patients experiencing fatigue or deconditioning, consider referral for physiotherapy or occupational therapy, or to local rehabilitation services to assist with energy conservation strategies and to establish safe baseline levels of physical activity. Patients with mild breathlessness may benefit from referral to a community physiotherapist or exercise physiologist, which could be facilitated under a chronic disease management plan. However, patients with moderate to severe breathlessness limiting exercise tolerance may require pulmonary rehabilitation and assessment by a respiratory physician. For patients with suspected POTS that is not adequately controlled by conservative measures (liberal fluid and salt intake, avoidance of triggers, compression or physiotherapy), consider referral to a cardiologist for advice regarding use of off-label medications.
Mood disorders are common among patients with long COVID and may contribute to ongoing symptoms. Patients with a diagnosed mental health disorder are eligible to access Medicare rebates and should be considered for referral to a mental health clinician. Referral to a long COVID clinic should be reserved for patients with difficulty accessing a variety of specialists, patients with prolonged symptoms that are not improving, and patients who would benefit from intensive multidisciplinary rehabilitation. Local HealthPathways offer clinical guidance and referral options to support care co-ordination.
Natural history and prognosis
Recovery from long COVID is variable and nonlinear. Patients who remain unwell at three months may still improve at a slower rate, although symptoms in many appear to plateau or fluctuate, with exacerbations during times of stress. A large study from Scotland (n = 31,486) assessing participants at six, 12 and 18 months after infection found minimal change in recovery status from full, partial or non-recovery, with only 13% of participants reporting improvement and 11% reporting deterioration between study visits.37 The PHOSP-COVID (Post-hospitalisation COVID-19) study (n = 2468) also found minimal improvement across multiple robust measures of physical, mental and cognitive performance between five and 12 months.38 There is some evidence to suggest hospitalised patients may experience a longer course of illness compared with nonhospitalised patients; however, further longitudinal studies are needed to inform prognosis.39
Large retrospective studies have also associated COVID-19 infection with increased risks of incident heart disease, new-onset diabetes, neurological disease and chronic kidney disease.40-42 The effects of SARS-CoV-2 infection and long COVID on neurodegenerative disease or cancer remain to be determined.
Conclusion
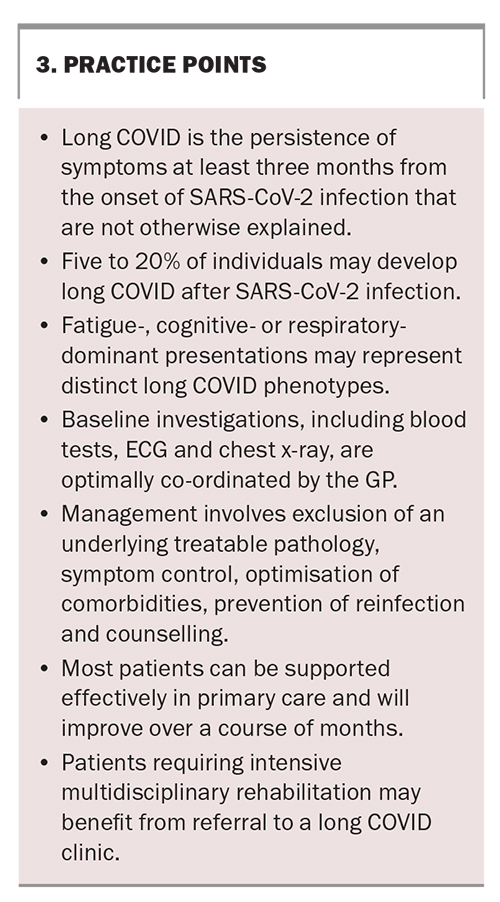
Long COVID is a chronic postviral syndrome affecting five to 20% of individuals after SARS-CoV-2 infection. Patients often present to their GPs with symptoms of fatigue, breathlessness or cognitive impairment that often limit everyday functioning. Investigations for alternative causes of illness and appropriate management should be initiated as early as one month after infection, particularly for patients with debilitating symptoms. Although there is no cure for long COVID, most patients can be effectively supported in primary care using chronic disease management principles. Further research into the immunological mechanisms of long COVID may identify novel therapeutic targets. Larger studies with robust longitudinal methodology in the postvaccine Omicron era are needed to inform prognosis. Practice points for GPs are presented in Box 3. MT
COMPETING INTERESTS: Mr Schiavone, Dr Darley: None. Professor Matthews has received institutional funding from Gilead, ViiV Healthcare and Janssen Australia; and is on Boards for Astra Zeneca, Gilead and Viiv Healthcare. Professor Dore has received clinical trial grants from Gilead Sciences and AbbVie. Associate Professor Stone has received honoraria from Astra Zeneca, Merck Sharp & Dohme and The Limbic; support for attending meetings from Astra Zeneca; is on the advisory board for Bristol Myers Squibb; and is Deputy Board Chair for the Thoracic Oncology Group of Australasia and Co-convenor of the Tobacco Control special interest group of the Thoracic Society of Australasia.
References
1. World Health Organization. WHO Coronavirus (COVID-19) Dashboard. WHO; Geneva, 2023. Available online at: https://covid19.who.int (accessed May 2023).
2. Australian COVID-19 Serosurveillance Network. Seroprevalence of SARS-CoV-2-specific antibodies among Australian blood donors: Round 4, updated February 2023. Available online at: https://kirby.unsw.edu.au/sites/default/files/COVID19-Blood-Donor-Report-Round4-Nov-Dec-2022.pdf (accessed May 2023).
3. World Health Organization. A clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021. WHO; Geneva, 2021. Available online at: https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1 (accessed May 2023).
4. Davis HE, Assaf GS, McCorkell L, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 2021; 38: 101019.
5. Hayes LD, Ingram J, Sculthorpe NF. More than 100 persistent symptoms of SARS-CoV-2 (long COVID): a scoping review. Front Med 2021; 8: 750378.
6. Davis, HE, McCorkell L, Vogel JM, et al. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol 2023; 21: 133-146.
7. Subramanian A, Nirantharakumar K, Hughes S, et al. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat Med 2022; 28: 1706-1714.
8. Hira R, Baker JR, Siddiqui T, et al. Objective hemodynamic cardiovascular autonomic abnormalities in post-acute sequelae of COVID-19. Can J Cardiol 2022; S0828-282X(22)01091-1.
9. Hama Amin BJ, Kakamad FH, Ahmed GS, et al. Post COVID-19 pulmonary fibrosis; a meta-analysis study. Ann Med Surg (Lond) 2022; 77: 103590.
10. Yuan C, Timmins F, Thompson DR. Post-intensive care syndrome: a concept analysis. Int J Nurs Stud 2021; 114: 103814.
11. Castanares-Zapatero D, Chalon P, Kohn L, et al. Pathophysiology and mechanism of long COVID: a comprehensive review. Ann Med 2022; 54: 1473-1487.
12. Swank Z, Senussi Y, Manickas-Hill Z, et al. Persistent circulating SARS-CoV-2 spike is associated with post-acute COVID-19 sequelae. Clin Infect Dis 2022; 76: e487-e490.
13. Phetsouphanh C, Darley DR, Wilson DB, et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat Immunol 2022; 23: 210-216.
14. O’Mahoney LL, Routen A, Gillies C, et al. The prevalence and long-term health effects of long Covid among hospitalised and non-hospitalised populations: a systematic review and meta-analysis. EClinicalMedicine 2023; 55: 101762.
15. Horberg MA, Watson E, Bhatia M, et al. Post-acute sequelae of SARS-CoV-2 with clinical condition definitions and comparison in a matched cohort. Nat Commun 2022; 13: 5822.
16. Ballering AV, van Zon SKR, Olde Hartman TC, Rosmalen JGM. Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study. Lancet 2022; 400: 452-461.
17. Whitaker M, Elliott J, Chadeau-Hyam M, et al. Persistent COVID-19 symptoms in a community study of 606,434 people in England. Nat Commun 2022; 13: 1957.
18. Office for National Statistics. New-onset, self-reported long COVID after coronavirus (COVID-19) reinfection in the UK: 23 February 2023. ONS; UK, 2023. Available online at: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/ (accessed May 2023).
19. Gao P, Liu J, Liu M. Effect of COVID-19 vaccines on reducing the risk of long COVID in the real world: a systematic review and meta-analysis. Int J Environ Res Public Health 2022; 19: 12422.
20. Hernández-Aceituno A, García-Hernández A, Larumbe-Zabala E. COVID-19 long-term sequelae: Omicron versus Alpha and Delta variants. Infect Dis Now 2023: 28; 104688.
21. Du M, Ma Y, Deng J, Liu M, Liu J. Comparison of long COVID-19 caused by different sars-cov-2 strains: a systematic review and meta-analysis. Int J Environ Res Public Health 2022; 19; 16010.
22. Fernández-de-Las-Peñas C, Martín-Guerrero JD, Pellicer-Valero Ó J, et al. Female sex is a risk factor associated with long-term post-COVID related-symptoms but not with COVID-19 symptoms: the LONG-COVID-EXP-CM Multicenter Study. J Clin Med 2022; 11: 413.
23. Han Q, Zheng B, Daines L, Sheikh A. Long-term sequelae of COVID-19: a systematic review and meta-analysis of one-year follow-up studies on post-COVID symptoms. Pathogens 2022; 11: 269.
24. Arnold CG, Libby A, Vest A, Hopkinson A, Monte AA. Immune mechanisms associated with sex-based differences in severe COVID-19 clinical outcomes. Biol Sex Differ 2022; 13: 7.
25. Mohammad S, Aziz R, Al Mahri S, et al. Obesity and COVID-19: what makes obese host so vulnerable? Immun Ageing. 2021; 18: 1.
26. Zimmerman KO. Efficacy of Antivirals and Other Therapeutics for Treatment of Post-Acute Sequelae of SARS-CoV-2 Infection (PASC). ClinicalTrialsgov Identifier: NCT05595369. 2023.
27. Stanford University. Selective Trial Of Paxlovid for PASC (STOP-PASC): randomized double-blind placebo-controlled pilot trial of paxlovid for the treatment of PASC. ClinicalTrialsgov Identifier: NCT05576662. 2023.
28. Xie Y, Choi T, Al-Aly Z. Association of treatment with nirmatrelvir and the risk of post–COVID-19 condition. JAMA Int Med 2023: e230743.
29. Forshaw D, Wall EC, Prescott G, et al. STIMULATE-ICP: a pragmatic, multi-centre, cluster randomised trial of an integrated care pathway with a nested, Phase III, open label, adaptive platform randomised drug trial in individuals with long COVID: a structured protocol. PLoS One 2023; 18: e0272472.
30. Jimeno-Almazán A, Buendía-Romero Á, Martínez-Cava A, et al. Effects of a concurrent training, respiratory muscle exercise, and self-management recommendations on recovery from post-COVID-19 conditions: the RECOVE trial. J Appl Physiol (1985) 2023; 134: 95-104.
31. Jimeno-Almazán A, Franco-López F, Buendía-Romero Á, et al. Rehabilitation for post-COVID-19 condition through a supervised exercise intervention: a randomized controlled trial. Scand J Med Sci Sports 2022; 32: 1791-801.
32. Pacho-Hernández JC, Fernández-de-Las-Peñas C, Fuensalida-Novo S, Jiménez-Antona C, Ortega-Santiago R, Cigarán-Mendez M. Sleep quality mediates the effect of sensitization-associated symptoms, anxiety, and depression on quality of life in individuals with post-COVID-19 pain. Brain Sci 2022; 12: 1363.
33. Frontera JA, Sabadia S, Yang D, et al. Life stressors significantly impact long-term outcomes and post-acute symptoms 12-months after COVID-19 hospitalization. J Neurol Sci 2022; 443: 120487.
34. d'Ettorre G, Vassalini P, Coppolelli V, et al. Health-related quality of life in survivors of severe COVID-19 infection. Pharmacol Rep 2022; 74: 1286-1295.
35. Bowe B, Xie Y, Al-Aly Z. Acute and postacute sequelae associated with SARS-CoV-2 reinfection. Nat Med 2022; 28: 2398-2405.
36. Watanabe A, Iwagami M, Yasuhara J, Takagi H, Kuno T. Protective effect of COVID-19 vaccination against long COVID syndrome: a systematic review and meta-analysis. Vaccine 2023; 41: 1783-1790.
37. Hastie CE, Lowe DJ, McAuley A, et al. Outcomes among confirmed cases and a matched comparison group in the long-COVID in Scotland study. Nat Commun 2022; 13: 5663.
38. Evans RA, Leavy OC, Richardson M, et al. Clinical characteristics with inflammation profiling of long COVID and association with 1-year recovery following hospitalisation in the UK: a prospective observational study. Lancet Respir Med 2022; 10: 761-775.
39. Global Burden of Disease Long COVID Collaborators. Estimated global proportions of individuals with persistent fatigue, cognitive, and respiratory symptom clusters following symptomatic COVID-19 in 2020 and 2021. JAMA 2022; 328: 1604-1615.
40. Salah HM, Fudim M, O'Neil ST, Manna A, Chute CG, Caughey MC. Post-recovery COVID-19 and incident heart failure in the National COVID Cohort Collaborative (N3C) study. Nat Commun 2022; 13: 4117.
41. Lai H, Yang M, Sun M, et al. Risk of incident diabetes after COVID-19 infection: a systematic review and meta-analysis. Metabolism 2022; 137: 155330.
42. Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature 2021; 594: 259-264.