Lipid-lowering therapy for older people: the changing paradigm

The benefits of lipid-lowering therapy (LLT) for secondary prevention of cardiovascular disease and primary prevention in middle-aged people at increased risk are well established. Until recently, however, LLT trials have included few people in older age groups, and there may have been a reluctance to prescribe LLT for primary prevention in these groups. Evidence is now accumulating for the benefits of LLT in older people, suggesting chronological age alone should no longer be a barrier to LLT.
- The main objective of lipid-lowering therapy (LLT) in older people is to stabilise atherosclerotic plaques, thereby minimising the risk of plaque rupture or erosion and ischaemic clinical events.
- There is now also strong evidence for the benefits of LLT for primary prevention of cardiovascular disease in older people, indicating that LLT should not be withheld in the absence of comorbidity that limits life expectancy or factors that may reduce compliance.
- The paradigm for LLT is changing, and chronological age should no longer be a bar to initiating LLT.
Recent studies have shown that the reduction in cardiovascular disease (CVD) events with lipid-lowering therapy (LLT) in older people (age 65 years and over) is almost identical to that in younger people. The international paradigm for LLT has shifted towards no discrimination on the basis of age. Significant numbers of older people in Australia are at high absolute CVD risk and therefore eligible for LLT as recommended by current Australian guidelines.1 However, fewer than half of people aged 65 years and over in Australia are currently receiving statin therapy.2
This article discusses the most recent evidence on the benefits of LLT in people aged 65 years and over. Advances in LLT and tailoring of LLT for older patients will be discussed in a future article.
How does lipid-lowering therapy prevent CVD events?
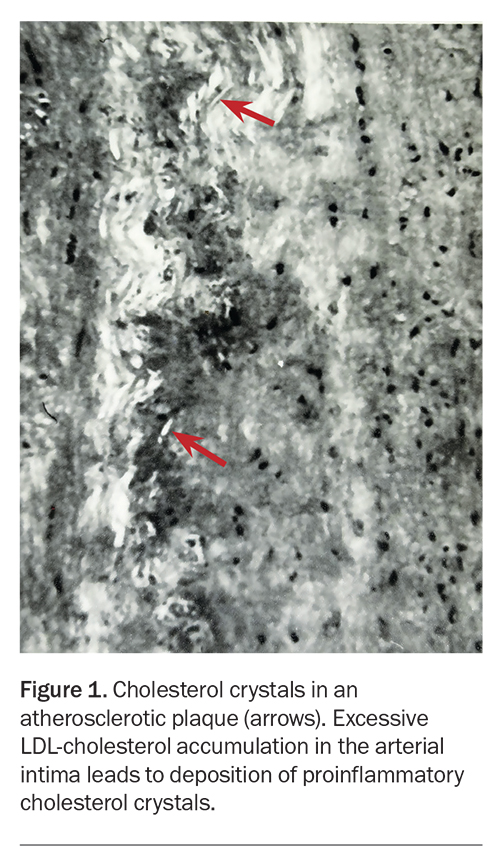
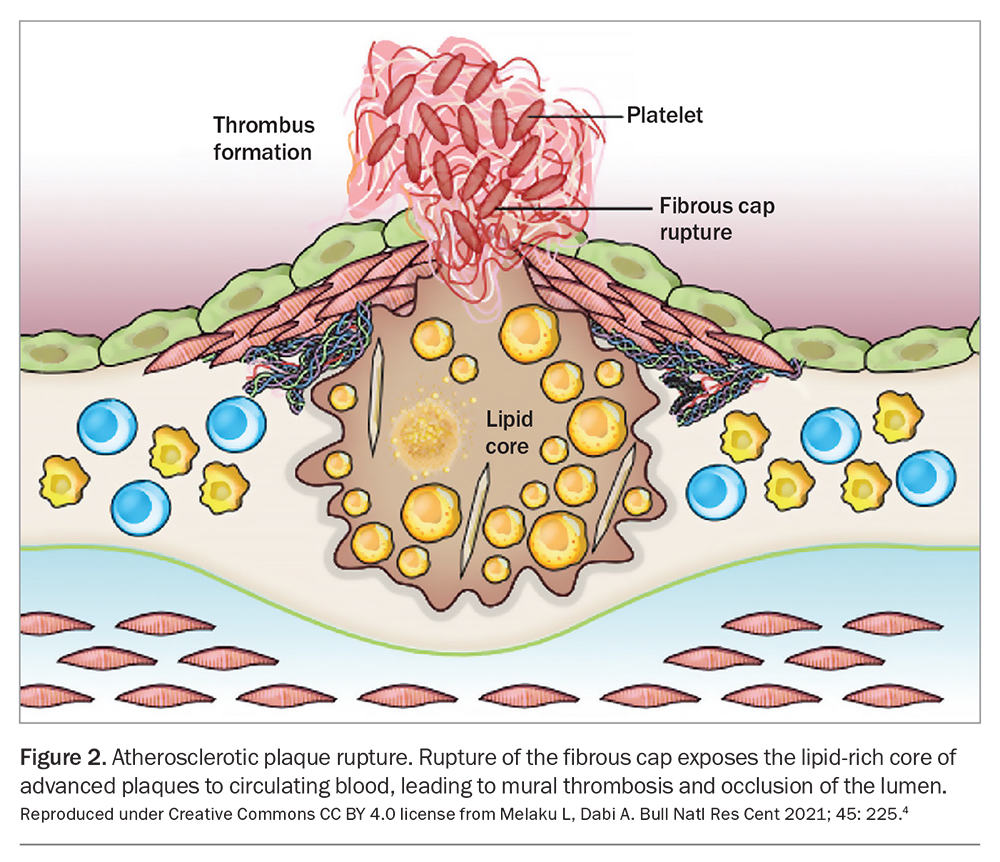
Atherosclerotic plaques result from cumulative exposure to circulating LDL particles, which accumulate in the intima of arteries and provoke an inflammatory response (Figure 1).3 Progression to fibrofatty and complicated plaques impairs blood flow, leading to distal ischaemia. Plaque rupture or erosion and mural thrombosis lead to acute events such as heart attack and stroke (Figure 2).4
The severity of atherosclerosis and risk of CVD are directly related to the duration and level of arterial exposure to LDL-cholesterol. An LDL-cholesterol exposure index can be calculated as: age × LDL-cholesterol level. CVD events occur above a certain threshold of exposure.5-7
Plaques are ‘plastic’ and capable of repair and remodelling, which can reduce lesion size and improve blood flow. In a recent six-year study of 3471 people aged 40 to 55 years, serial three-dimensional ultrasonic imaging of the carotid and femoral arteries found plaque initiation followed by progression occurred in 17.5% and progression of pre-existing plaques in 15%, whereas complete regression occurred in 8%.8
The aim of LLT is to lower long-term arterial exposure to LDL, thereby allowing plaques to change in structure and composition to prevent either rupture or erosion. Long-term reduction of the LDL-cholesterol level can significantly reduce the lifetime risk of CVD events. For example, reducing the LDL-cholesterol level by 50% from a population mean of 3.5 mmol/L reduces the lifetime risk of CVD by 52%, 46%, 37% or 27% when started at ages 30, 40, 50 or 60 years, respectively, and continued up to age 80 years.6 LLT begun early in life (so-called ‘primordial prevention’) could theoretically prevent plaque formation. The goal of LDL-cholesterol lowering for all age groups can be summarised as ‘earlier, lower, longer’.
Need for LLT in the older population
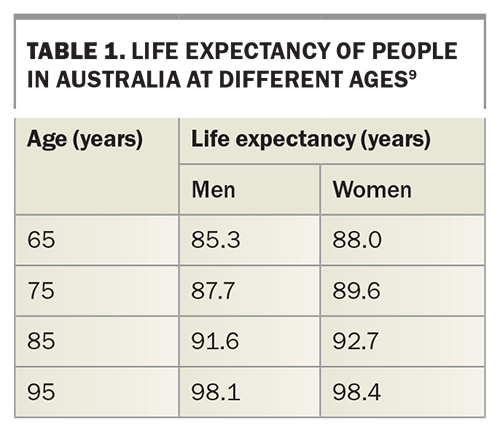
Older patients requiring LLT are now more common in Australian general practice, as the number of older people at high CVD risk increases in parallel with population ageing and longer life expectancy. In 2021, almost 17% of the Australian population were aged 65 years and over.9 By 2041, the number of people in this age group is expected to increase by 54%, and the number aged 85 years or over by 140%. Life expectancy is also increasing, and this increase is often underestimated. A woman currently aged 80 years is expected to live to 90 years (Table 1).9
CVD in the older population
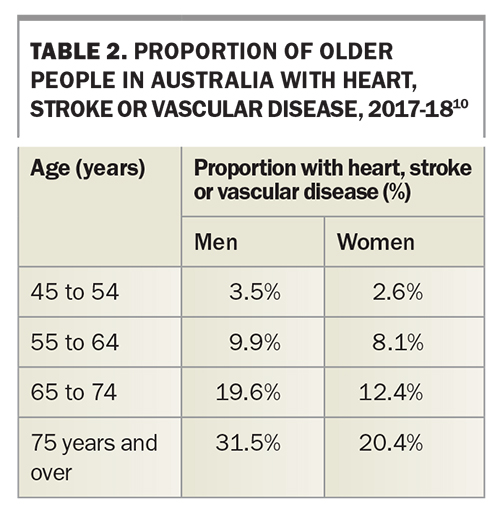
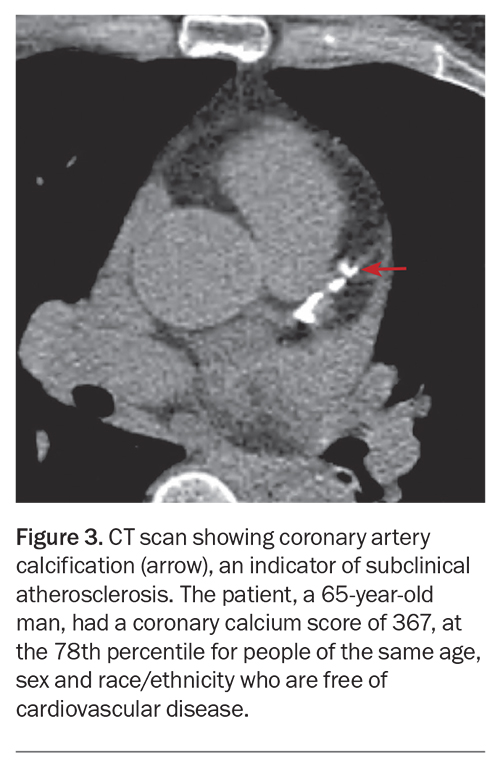
Heart disease is the most common cause of death in both men and women aged 65 years and over, and two-thirds of CVD deaths occur in people aged over 75 years.10 Around one-third of men and one-fifth of women aged 75 years and over have symptomatic CVD (Table 2).10 Most people aged 65 years or over have demonstrable subclinical atherosclerosis, manifesting as atherosclerotic plaques observed on vascular ultrasound examination or coronary calcium on CT (Figure 3).11
CVD risk factors in the older population
In 2022, almost one-third of people aged over 75 years in Australia had a high total cholesterol level, and a similar proportion had a high LDL-cholesterol level.12 Over 8% of people self-reported high cholesterol as a current health condition.13
In people aged 65 years and over in Australia:14
- 76% are overweight or have obesity
- 40 to 45% have hypertension
- 17% have diabetes
- 38% have a sedentary lifestyle
- 7% smoke cigarettes.
The prevalence of all these risk factors (other than cigarette smoking) increases progressively with age from 65 years to the 75 years plus age group. For example, in 2021, almost one in five people aged 80 to 84 years in Australia (22.1% of men and 17.2% of women) had diabetes, almost 30 times higher prevalence than in those aged under 40 years (0.7%).14
A US study found that about 40% of adults aged over 70 years have metabolic syndrome, manifesting as various combinations of high triglyceride level, low HDL-cholesterol level, increased waist circumference and central adiposity, insulin resistance, hypertension and hyperglycaemia.15 A high prevalence of metabolic syndrome has also been found in Australian studies.16 The presence of the metabolic syndrome is associated with a two- to threefold higher incidence of coronary heart disease.15
Prevalence of statin therapy in older people
A recent Australian study showed the proportion of new users of high-intensity statins in people aged 65 years and over increased year on year between 2007 and 2016, from 23.6% to 30.5%.2 Women were 18% less likely than men to begin statin therapy across all years. The incidence of statin use was also highest in those aged 65 to 74 years, who were about 15% and 45% more likely to begin statin use than those aged 75 to 84 years and 85 years and over, respectively.2
Although adverse reactions to statin therapy may be more frequent in older people, including interactions with other therapy, statins are generally well tolerated, as in younger age groups.17,18
Studies of LLT in older patients
Pre-2018 studies of LLT in older people
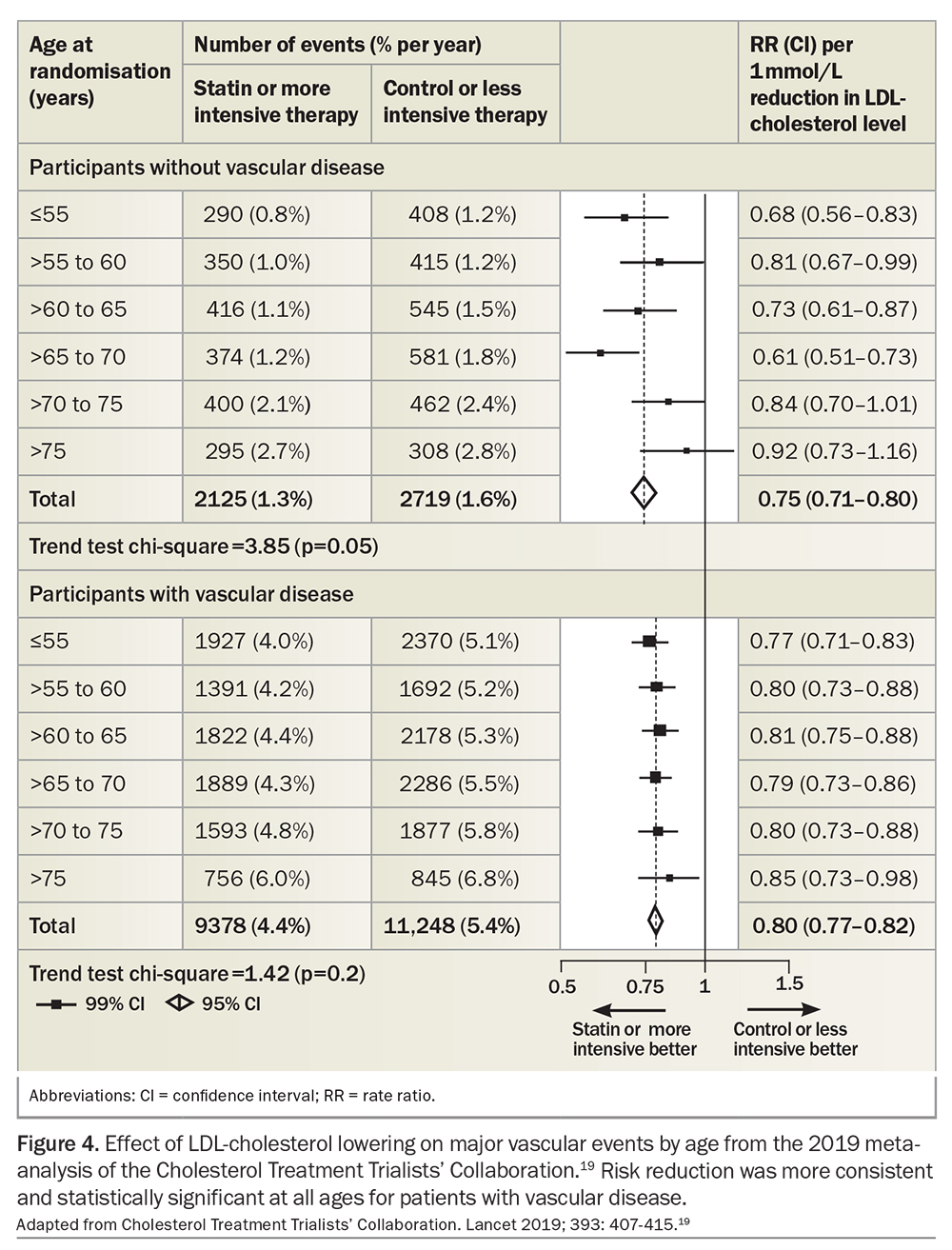
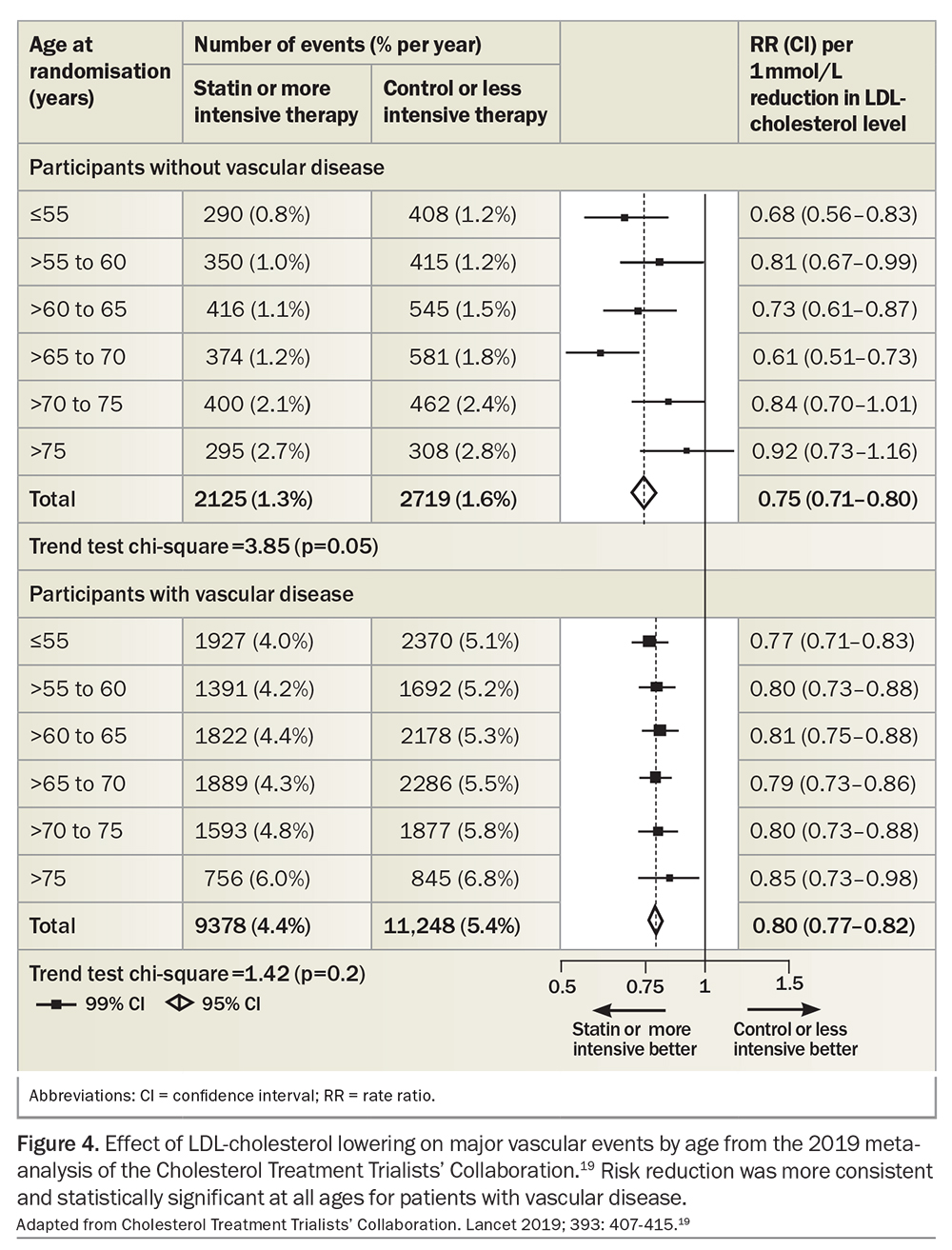
Results of studies of LLT in older patients published before 2018 were summarised in the meta-analysis of the Cholesterol Treatment Trialists’ Collaboration (Figure 4).19 For all age groups, secondary prevention of CVD with LLT resulted in highly statistically significant and unequivocal reductions in CVD events. However, for people without CVD in the oldest age groups (over 75 years), differences in CVD rates were not statistically significant between those with lower and higher LDL-cholesterol levels, most likely because of the smaller number of participants in these groups. For every 1 mmol/L reduction in LDL-cholesterol level, CVD risk was reduced by around 20% for primary prevention and 25% for secondary prevention over a five-year period (Figure 4).19 Absolute risk reduction was higher in older age groups, in whom the number needed to treat to prevent one event (NNT) was correspondingly lower. Statin therapy had no effect on nonvascular mortality, cancer death or cancer incidence at any age.
More recent meta-analyses of primary prevention
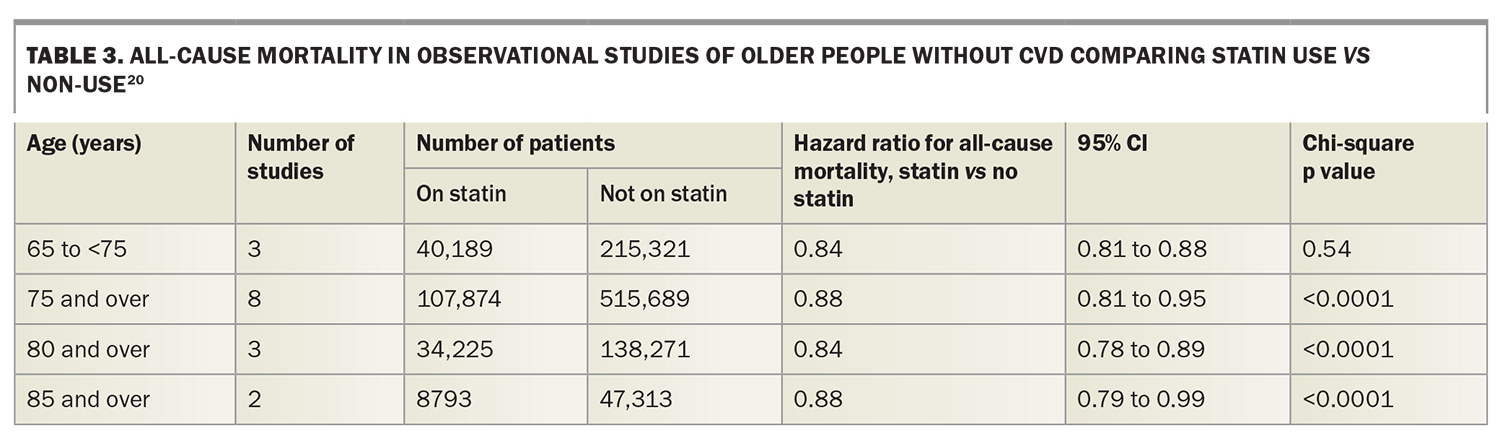
A 2021 meta-analysis of observational studies in people aged 65 years and over without CVD found that statin therapy was associated with a 12 to 16% lower risk of CVD death, stroke and all-cause mortality across all age groups (Table 3).20
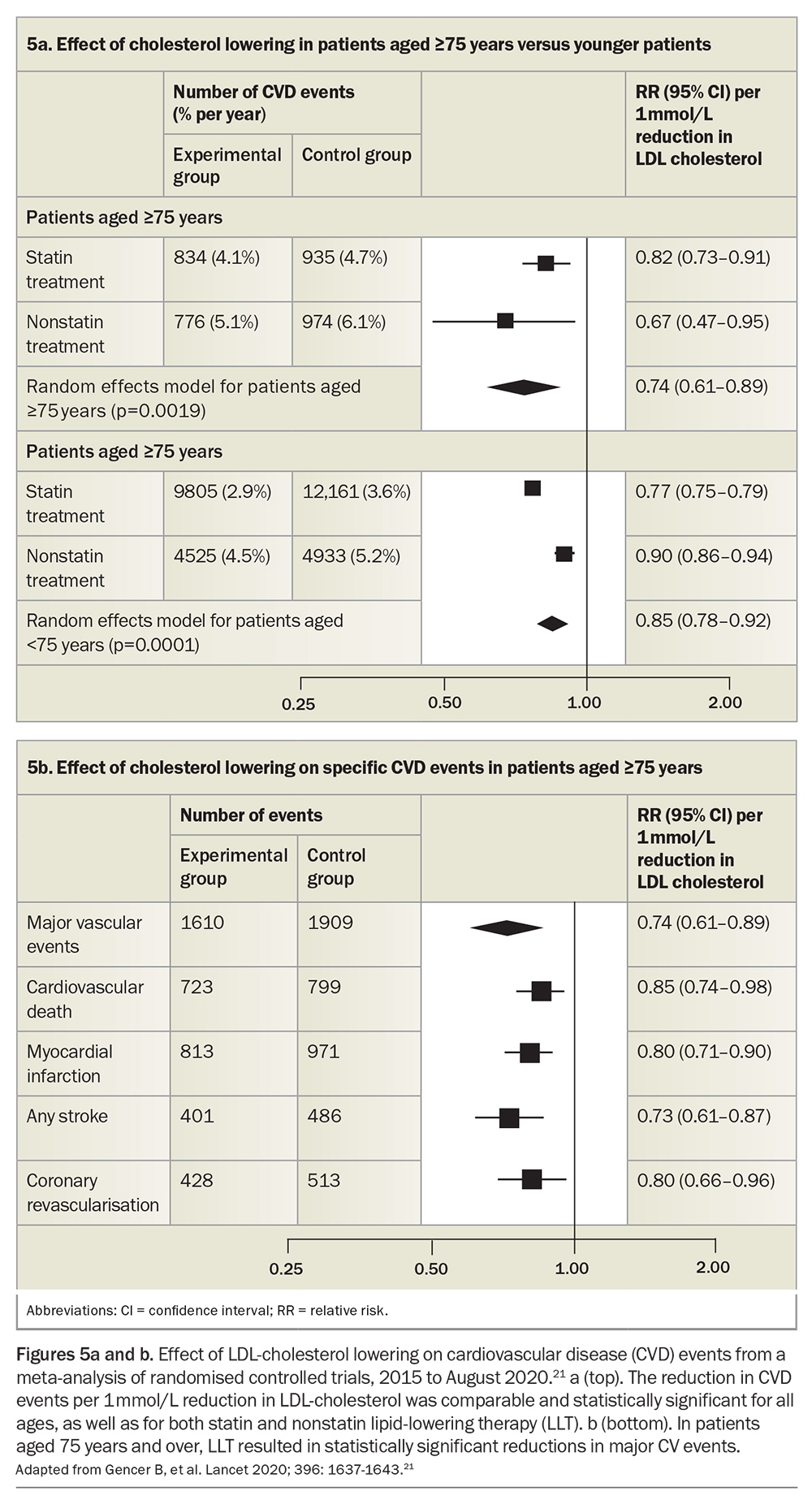
Only recently have sufficient numbers of older people without vascular disease been included in randomised controlled trials to provide robust evidence for the effectiveness of LLT in primary prevention. The latest meta-analysis of primary prevention studies published up until August 2020 included 244,090 participants, of whom 8.8% were aged 75 years and over (Figures 5a and b).21 The benefits of lowering the LDL-cholesterol level were independent of the means by which this was achieved, which included statins, bile acid sequestrants, ezetimibe or proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors (Figure 5a). Reductions in CVD events for people aged 75 years and over were: 15% for CVD death, 20% for myocardial infarction, 27% for stroke and 20% for coronary revascularisation (Figure 5b). CVD events were reduced by around 26% per 1 mmol/L LDL-cholesterol reduction in all age groups. Absolute risk reductions were greater in older age groups with higher baseline risk, as found in earlier meta-analyses.21
Population study of LLT for primary prevention
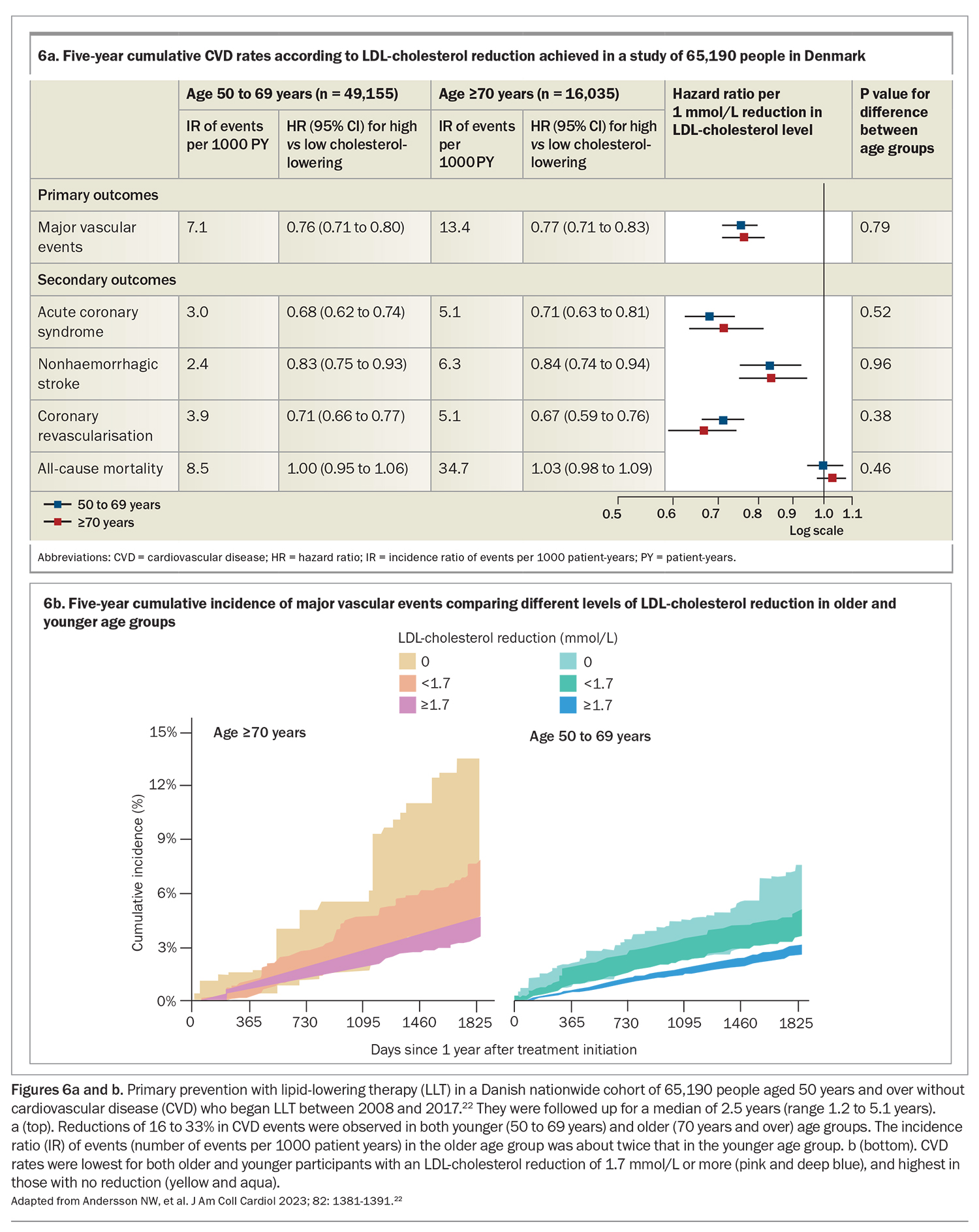
An observational study of the Danish population analysed CVD rates in people aged 50 years and over without vascular disease who had begun LLT between 2008 and 2017 (Figures 6a and b).22 CVD rates were compared between 16,035 participants aged 70 years and over and 49,155 younger participants. LLT reduced LDL-cholesterol level by a mean of 1.7 mmol/L. In both age groups, each 1 mmol/L reduction in LDL-cholesterol level was significantly associated with a 23% lower risk of CVD events.22
In participants aged 70 years and over, the cumulative incidence of CVD was about 13.5%, 7.5% and 4.5% for those with no reduction in LDL-cholesterol level, a reduction less than 1.7 mmol/L and a reduction of 1.7 mmol/L or greater, respectively. Corresponding figures in younger participants were 7.5%, 5% and 3% (Figure 6b).22
Conclusion
The evidence to date suggests that not only is LLT important for secondary prevention of CVD in older people but it is also of increasingly recognised benefit for primary prevention. In the absence of comorbidity that limits life expectancy or factors that may reduce compliance, chronological age should not be a bar to initiating LLT. A new approach to LLT for older patients will be discussed in a future article, including recommended monitoring and how to address adverse drug reactions. MT
COMPETING INTERESTS: Professor Hamilton-Craig is honorary Chairman of the SA Lipid Group, sponsored by Amgen (Australia).
References
1. Australian CVD risk calculator. CVD risk guideline. Overview. Canberra: Australian Government Department of Health and Aged Care; 2023. Available online at: https://cvdcheck.org.au/overview (accessed January 2024).
2. Ofori-Asenso R, Ilomäki J, Zomer E, Curtis AJ, Zoungas S, Liew D. A 10-year trend in statin use among older adults in Australia: an analysis using national pharmacy claims data. Cardiovasc Drugs Ther 2018; 32: 265-272.
3. Ospina-Romero M, Schultze JJ. Heart and vascular pathology. Ischemic disease. Atherosclerotic coronary artery disease. PathologyOutlines.com; 2022. Available online at: https://www.pathology outlines.com/topic/heartatheroscleroticCAD.html (accessed January 2024).
4. Melaku L, Dabi A. The cellular biology of atherosclerosis with atherosclerotic lesion classification and biomarkers. Bull Natl Res Cent 2021; 45: 225.
5. Grundy SM, Feingold KR. Guidelines for the management of high blood cholesterol. Updated 2022. In: Feingold KR, Anawalt B, Blackman MR, et al, editors. Endotext. South Dartmouth (MA): MDText.com; 2000. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK305897/ (accessed January 2024).
6. Ray KK, Ference BA, Séverin T, et al. World Heart Federation Cholesterol Roadmap 2022. Glob Heart 2022; 17: 75.
7. Domanski M, Tian X, Wu C, et al. Time course of LDL cholesterol exposure and cardiovascular disease event risk. J Am Coll Cardiol 2020; 76: 1507-1516.
8. Mendieta G, Pocock S, Mass V, et al. Determinants of progression and regression of subclinical atherosclerosis over 6 years. J Am Coll Cardiol 2023; 82: 2069-2083.
9. ARC Centre of Excellence in Population Ageing Research (CEPAR). CEPAR population ageing futures data archive. Available online at: https://cepar.edu.au/cepar-population-ageing-projections (accessed January 2024).
10. Australian Bureau of Statistics (ABS). Analysis of microdata: National Health Survey, 2014-15. Canberra: ABS; 2016.
11. Asian Heart and Vascular Centre (AHVC). Coronary calcium score. Available online at: https://www.ahvc.com.sg/service/coronary-calcium-score/ (accessed January 2024).
12. Australian Institute of Health and Welfare (AIHW). Heart, stroke and vascular disease: Australian facts. Canberra: AIHW; 2023. Available online at: https://www.aihw.gov.au/reports/heart-stroke-vascular-disease/hsvd-facts/contents/about (accessed January 2024).
13. Australian Bureau of Statistics (ABS). High cholesterol. Contains key statistics and information about high cholesterol and its prevalence in Australia. Reference period 2022. Canberra: ABS; 2023. Available online at: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/high-cholesterol/latest-release (accessed January 2024).
14. Australian Institute of Health and Welfare (AIHW). Older Australians. Canberra: AIHW; 2023. Available online at: https://www.aihw.gov.au/reports/older-people/older-australians/contents/health/behavioural-risk-factors (accessed January 2024).
15. Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA 2002; 287: 356-359.
16. Barr ELM, Magliano DL, Zimmet PZ, et al. AusDiab 2005. The Australian Diabetes, Obesity and Lifestyle Study. Melbourne: International Diabetes Institute; 2006. Available online at: https://www.baker.edu.au/-/media/documents/impact/ausdiab/reports/ausdiab-report-2005 (accessed January 2024).
17. Cholesterol Treatment Trialists’ Collaboration.Effect of statin therapy on muscle symptoms: an individual participant data meta-analysis of large-scale, randomised, double-blind trials. Lancet 2022; 400: 832-845. Erratum in: Lancet 2022; 400: 1194.
18. Newman CB, Preiss D, Tobert JA, et al; American Heart Association Clinical Lipidology, Lipoprotein, Metabolism and Thrombosis Committee, a Joint Committee of the Council on Atherosclerosis, Thrombosis and Vascular Biology and Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Clinical Cardiology; and Stroke Council. Statin safety and associated adverse events: a scientific statement from the American Heart Association. Arterioscler Thromb Vasc Biol 2019; 39: e38-e81. Erratum in: Arterioscler Thromb Vasc Biol 2019; 39: e158.
19. Cholesterol Treatment Trialists’ Collaboration. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet 2019; 393: 407-415.
20. Awad K, Mohammed M, Zaki MM, et al; Lipid and Blood Pressure Meta-analysis Collaboration (LBPMC) Group and the International Lipid Expert Panel (ILEP). Association of statin use in older people primary prevention group with risk of cardiovascular events and mortality: a systematic review and meta-analysis of observational studies. BMC Med 2021; 19: 139.
21. Gencer B, Marston NA, Im K, et al. Efficacy and safety of lowering LDL cholesterol in older patients: a systematic review and meta-analysis of randomised controlled trials. Lancet 2020; 396: 1637-1643.
22. Andersson NW, Corn G, Dohlmann TL, Melbye M, Wohlfahrt J, Lund M. LDL-C reduction with lipid-lowering therapy for primary prevention of major vascular events among older individuals. J Am Coll Cardiol 2023; 82: 1381-1391.