Asthma-COPD overlap. Implications for patient management

Asthma-COPD overlap (ACO) is characterised by persistent airflow limitation with features typically associated with both asthma and chronic obstructive pulmonary disease (COPD). Because there is no universally accepted definition of ACO, reliable data on managing patients exhibiting ACO are lacking. An approach to treating chronic airways disease that targets identifiable clinical traits rather than the disease label is increasingly recommended.
- The term asthma-COPD overlap (ACO) was proposed to reflect the overlapping aetiologies and clinical features of asthma and chronic obstructive pulmonary disease (COPD) and the large population of patients who demonstrate features of both.
- Clinical features and underlying inflammatory and physiological mechanisms of asthma and COPD are highly variable and affect the utility of the ACO umbrella in clinical practice. This heterogeneity limits both high-quality research on the subject and treatment recommendations specific to ACO.
- Initiation of inhaled corticosteroids is recommended in patients who clearly demonstrate features of both asthma and COPD, as this is a critical component of asthma control.
- An individualised approach to treatment, with a focus on identifying and treating disease traits is more important than managing disease labels, and will lead to better overall care of the patient with chronic airway disease.
Asthma and chronic obstructive pulmonary disease (COPD) are the most prevalent chronic lung diseases and are responsible for considerable morbidity, mortality and the use of healthcare resources globally.1,2 In Australia, up to 11% of the population report a diagnosis of asthma.3 The prevalence of COPD is estimated at 7.5% of Australians over 40 years of age, and this increases to 30% for those over 75 years.4 Once managed as distinct diagnoses, it is now increasingly acknowledged that asthma and COPD have overlapping aetiologies and clinical features that translate to a high likelihood that patients will demonstrate features of both conditions.5 Despite this reality, guidelines for both conditions have evolved separately and differ significantly in recommendations for treatment.1,2 The term asthma-COPD overlap (ACO) was proposed to assist clinicians resolve this dilemma and provide an approach to treatment; however, there is controversy over whether ACO should be regarded as a separate entity in itself. The alternative is for clinicians to move away from the confinement of disease labels and instead take a ‘treatable traits’ approach to chronic airways disease and identify important clinical phenotypes and target treatment towards these.6 This article discusses ACO its implications for patient treatment.
What is asthma-COPD overlap (ACO)?
Although proposed definitions of ACO differ between respiratory societies, ACO is generally characterised by persistent airflow limitation with features typically associated with both asthma and COPD, such as a history of smoking, a documented history of asthma before the age of 40, a history of atopy and elevated eosinophils on full blood count (FBC; more than 0.3×109/L).7,8 This definition is based on expert opinion and does not define ACO as an independent entity based on either pathophysiology or disease outcomes.
In clinical practice, the relative contribution from features of asthma or COPD will differ substantially between patients, resulting in a cohort of patients with the label of ACO who display highly variable disease mechanisms and clinical outcomes A patient who fits the above definition of ACO may indeed have asthma and COPD concurrently, though they may instead have an atypical manifestation of one of these conditions alone, such as COPD with eosinophilic inflammation, or asthma with irreversible airflow obstruction due to airway remodelling.
Pathophysiology and clinical features
Asthma and COPD are conditions that feature airflow limitation and chronic airway inflammation,1,2 although each of these chronic airway diseases are themselves heterogenous conditions with various contributing disease mechanisms and inflammatory processes. This highlights the complexity and lack of utility of the ACO umbrella.
Asthma is defined as an inflammatory airways disease that often, but not exclusively, begins in childhood. Asthma involves the large and small airways, but not the terminal bronchioles or alveoli, and is characterised by airway hyper-responsiveness and reversible airway obstruction.2 COPD is also an inflammatory airways disorder associated with inhaled noxious agents such as tobacco smoke, which usually manifests in people over 40 years of age. COPD predominantly affects the small airways and is associated with varying amounts of alveolar tissue breakdown and mucous hypersecretion. The condition is characterised by progressive and irreversible airway obstruction, loss of lung elastic recoil and hyperinflation, and symptoms of breathlessness, productive cough and wheeze.1
The inflammatory cells and mediators that drive COPD and asthma broadly differ but there is no pathognomonic inflammatory endotype that defines ACO. COPD is typically characterised by inflammation, referred to as a type 1 (T1) immune response, featuring a predominance of neutrophils, CD8+ T cells, macrophages and inflammatory mediators such as interleukin (IL)-8 and tumour necrosis factor (TNF) alpha-1. Asthma is usually a type 2 immune process characterised by elevated eosinophils, mast cells, CD4+ T cells and cytokines IL-4, IL-5 and IL-13.2,9 Type 2 (T2) inflammation refers to a pattern of inflammation driven by T helper 2 cells and other components of the innate immune system, with increased activity of eosinophils and the allergic inflammatory cascade. Active T2 inflammation has been demonstrated to correspond with asthma symptoms, increased exacerbation frequency and lung function decline. T2 inflammation is generally responsive to inhaled corticosteroid (ICS) or oral corticosteroid (OCS) therapy. Neither of these inflammatory processes are specific for either disease. Asthma driven by neutrophilic inflammation is a recognised phenotype in 15 to 20% of people with asthma,10 and eosinophilic inflammation is recognised in up to 20% of people with COPD.2,11 The differences between and similarities in airway inflammation and airway remodelling in asthma, COPD and ACO are complex and require further investigation.12
Similarly, spirometry does not always distinguish between asthma and COPD. Bronchodilator reversibility (BDR) is a defining feature of asthma; however, patients with COPD often and variably demonstrate a significant improvement in forced expiratory volume in one second (FEV₁) with bronchodilators.13 Conversely, airflow obstruction that is not fully reversible is a defining feature of COPD, but can occur as a result of airway remodelling in cases of asthma alone, particularly in patients with longstanding disease.2 Patients with either COPD or asthma can also demonstrate hyper-responsiveness on bronchial provocation testing.14
Diagnosing patients with ACO
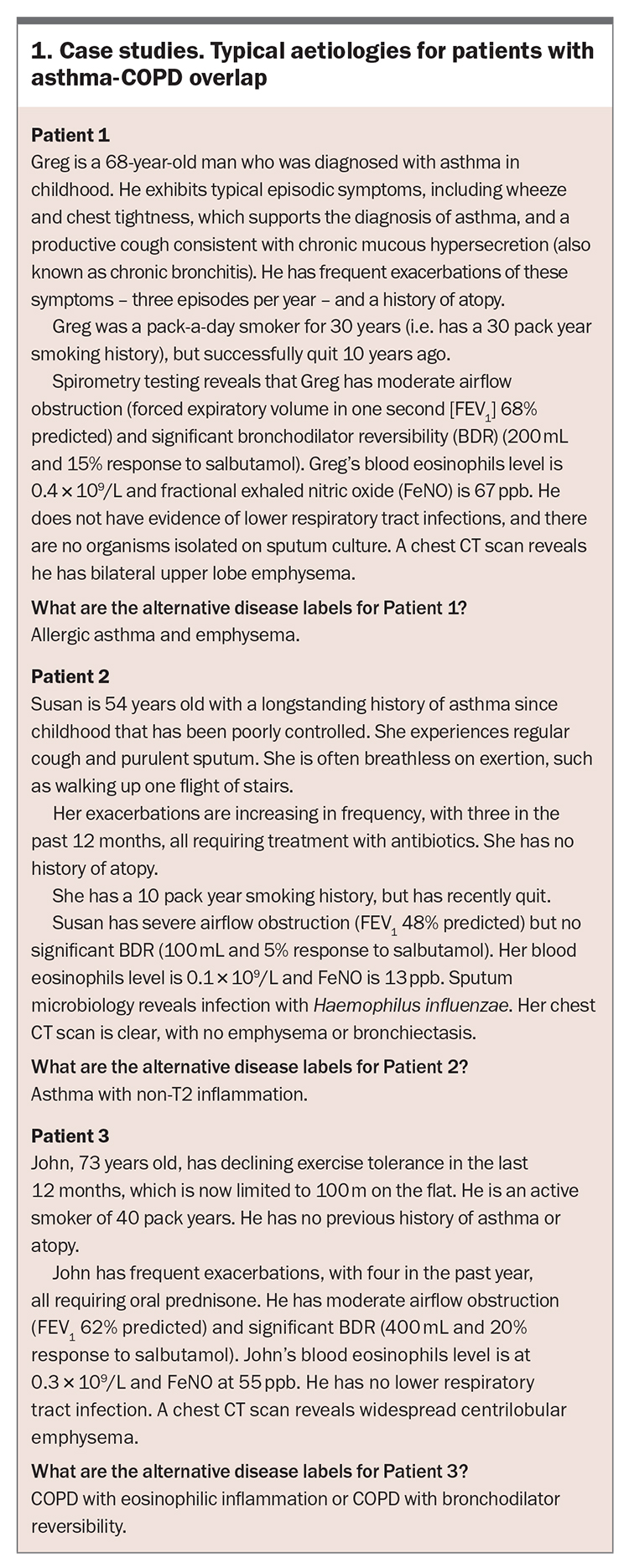
Box 1 outlines three case studies of patients with aetiologies that fit the description of ACO based on current consensus statements. However, it could be argued these patients have different diseases that will affect their prognosis and response to treatment.
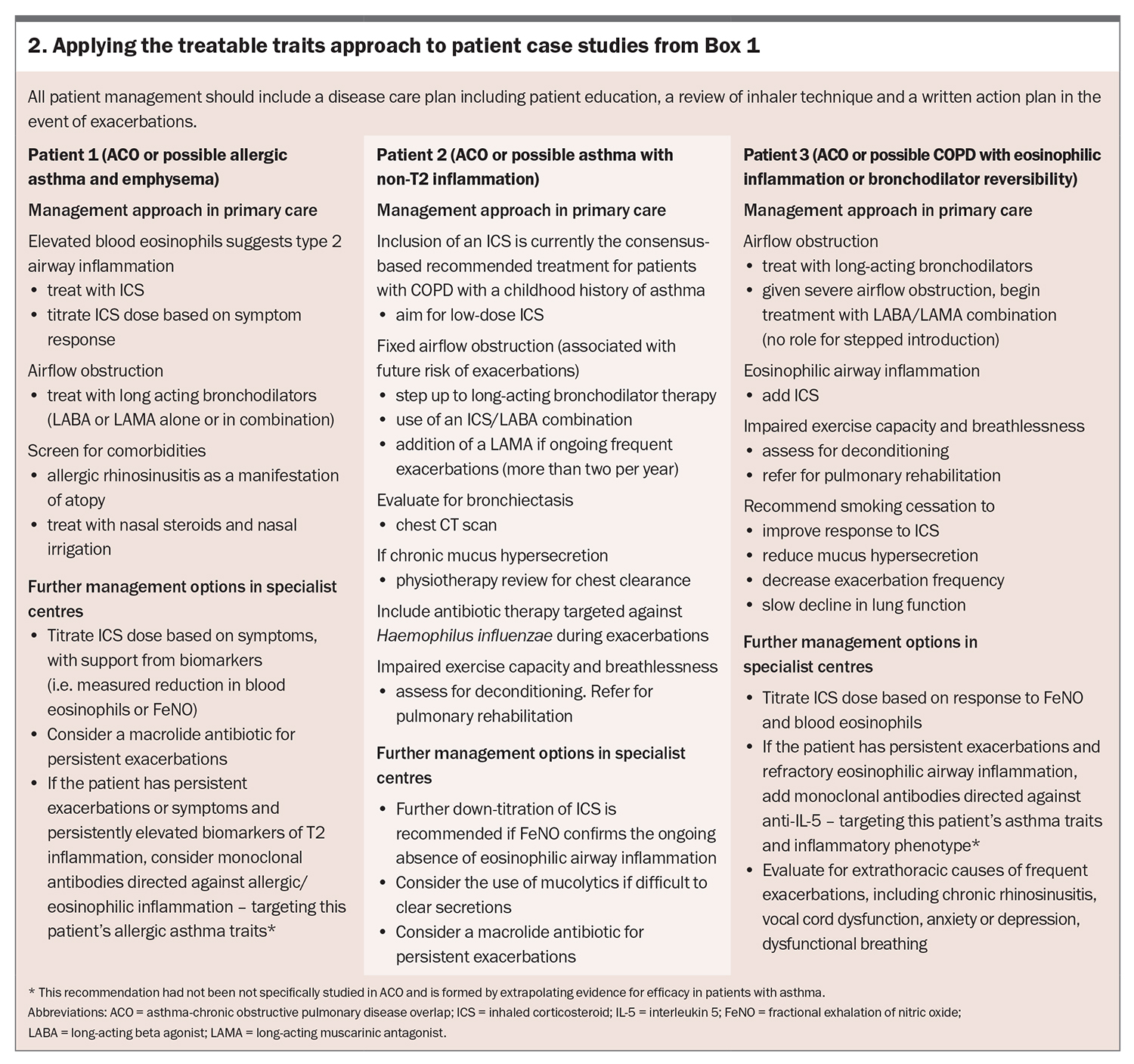
Patient 1 has a history of early-onset asthma with typical symptoms, a history of atopy and elevated biomarkers to suggest active type 2 inflammation. Elevated levels of eosinophils on FBC (particularly when higher than 0.3 × 109/L) correlate with active T2 inflammation and are a readily available way to assess this. Eosinophils can be elevated due to other causes, such as potential atopy in the case of Patient 1. Although not routinely available in general practice, fractional exhalation of nitric oxide (FeNO) is a more specific and noninvasive method of detecting eosinophilic airway inflammation, with readings over 50 ppb consistent with this. Despite the patient’s features of allergic asthma, his heavy smoking history and CT evidence of emphysema are typically associated with COPD.
Patient 2 has a diagnosis of early-onset asthma and significant airflow obstruction. The incompletely reversible airflow obstruction suggests a diagnosis of COPD, although her smoking history is relatively mild and there is no CT evidence of emphysema. It is likely that the patient’s fixed airflow obstruction is a direct result of her longstanding asthma and subsequent airway remodelling, rather than loss of elastic recoil and increased airway resistance as that occurs with COPD associated with an emphysema predominant phenotype. The absence of biomarkers of T2 inflammation suggests a poor response to typical ICS and OCS therapy. A poor response to corticosteroid therapy has been well described in people with neutrophilic asthma.
Patient 3 has a heavy smoking history and clear radiological evidence of emphysema. BDR can exist in COPD alone; however, the magnitude of BDR in this case increases the likelihood that this is true evidence of concurrent asthma. Although eosinophilic inflammation is recognised in COPD, the elevated T2 biomarkers in Patient 3 may suggest a diagnosis of asthma as described above.
The patients described in these case studies will be recognisable to all clinicians and will raise questions including: What treatment paradigm should be followed? Do you treat a disease label, such as asthma, COPD, or ACO, or do you treat the individual treatable traits?
Quality of research on ACO
Prospective intervention trials of patients who meet a definition of ACO are lacking, with most research limited to cohort and case-controlled studies.15 Data from these studies yield varying and sometimes conflicting results because of the lack of an accepted definition of ACO and inconsistent inclusion criteria.7,15 Treatment recommendations for ACO are extrapolated from trials of asthma and COPD alone; however, the inclusion criteria for these same trials would have excluded most patients with ACO.7,16-19 For example, asthma trials will often exclude patients with even a minor smoking history or with a past diagnosis of COPD,20-22 and most COPD studies will exclude never-smokers or those with a history of asthma.17,23
Epidemiology and natural history
The reported global prevalence of ACO varies between 15 and 55% but is critically dependent on the inclusion criteria in the individual studies.8 Patients who meet the definition of ACO are generally younger, have a higher body mass index, are less likely to have a smoking history, have a higher FEV₁ and more healthcare utilisation than patients with COPD alone.15 Patients with ACO are at increased risk of exacerbations, hospitalisations and a greater number of chronic respiratory symptoms; therefore, outcomes may be worse with ACO compared with asthma or COPD alone.5,15 Observations are often inconsistent between studies, which makes it difficult to draw valid conclusions.
Treatment of ACO – negotiating the contrasting inhaler therapies for asthma and COPD
The most common dilemma for the clinician treating a patient with ACO is which inhaler therapy to initiate and when.1,2 ICS therapy is the cornerstone of asthma management, and the addition of long-acting bronchodilators is indicated only if insufficient control is achieved with ICS. Bronchodilators – both short- and long-acting – represent a major part of the management of COPD, and ICS is only added in certain circumstances of advanced disease. The recommended management of asthma and COPD, with a focus on inhaler therapy, is briefly outlined below to highlight their sometimes contrasting management.
For adolescents and adults with asthma, including mild asthma, ICS therapy is recommended to decrease the risk of exacerbations and improve control of asthma symptoms.2,24,25 Long-acting beta- agonists (LABAs) reduce the frequency of severe asthma exacerbations when combined with ICS therapy and are recommended in combination with ICS therapy if inadequate control is achieved with ICS alone.2,21 LABA monotherapy has been linked with increased rates of asthma-related death and is contraindicated in the absence of ICS therapy.2,26,27 The long acting muscarinic antagonist (LAMA) tiotropium improves lung function, exacerbation rates and asthma control when added to ICS/LABA combinations, and is recommended only for those with inadequate control and persistent exacerbations despite (high-dose) ICS/LABA combinations.2,22
Treatment of COPD is similarly based on the management of symptoms and to reduce the risk of exacerbations, but in contrast to asthma, bronchodilator therapy is the preferred first-line therapy, rather than ICS.1 Long-acting bronchodilator therapy (LAMA alone or in combination with LABA) has been shown to improve lung function and COPD symptoms, and reduce the frequency of exacerbations and hospitalisations.17,18,23 The addition of ICS therapy should be considered in the setting of persistent exacerbations despite long-acting bronchodilator therapy, although this recommendation is strongest for patients with elevated blood eosinophil counts (>0.3 × 109/L), and may offer no benefit to those with persistently low blood eosinophil counts (<0.15 × 109/L).1,28,29 As described above, the inflammation in COPD is usually driven by neutrophilic (T1) inflammation, which is less responsive to corticosteroids than the eosinophilic (T2) inflammation associated with asthma. With the increased appreciation of an overlap between our traditional understanding of asthma and COPD inflammatory patterns, there will be a cohort of patients with COPD who demonstrate evidence of eosinophilic airway inflammation, with elevated blood eosinophils (above 0.3 × 109/L) and elevated FeNO (above 50 ppb) (although FeNO measurement is not necessary to diagnose eosinophilic inflammation in the primary care setting), and are more likely to respond to ICS therapy. It is therefore important to check for evidence of eosinophilic airway inflammation in patients with COPD, as this will influence treatment options, although it should be noted that the addition of ICS to COPD in the absence of frequent exacerbations or a concurrent diagnosis of asthma constitutes off-label use. The use of ICS in COPD has been linked to an increased risk of pneumonia and tempers enthusiasm for its use in COPD that can be adequately managed with bronchodilator therapy alone, particularly in the majority of patients with COPD who do not demonstrate evidence of eosinophilic inflammation.13,30
In people with COPD and moderate to severe exacerbations, mepolizumab (an anti-IL5 monoclonal antibody) reduced exacerbations, with the effect dependent on the degree of peripheral blood eosinophilia.31 The reduction in exacerbations was more pronounced in patients with persistently higher blood eosinophil counts (>0.3 × 109/L) treated with dupilumab (an anti-IL-4/IL-13 monoclonal antibody).32 These studies reinforce the importance of targeting T2 inflammatory pathways as a disease trait, specifically in the context of COPD.
Consensus treatment of ACO with inhaled therapy
Evidence to support specific treatment recommendations for ACO as a single disease is limited. Most experts support the initiation of ICS therapy early in the disease course of patients who fit the definition of ACO, as this is an important part of asthma control.2,5,8 If a patient with an established diagnosis and treatment regimen for COPD demonstrates features of asthma such as bronchodilator reversibility or eosinophilic inflammation (blood or sputum), the addition of an ICS is supported by expert consensus, although data only supports the use of ICS in those with evidence of eosinophilic inflammation.8,33 Evidence is emerging to support the use of mepolizumab and dupilumad in those with persistent exacerbations despite ICS use and persistently high blood eosinophil counts.31,32
Overall care of the patient with ACO: the treatable traits approach
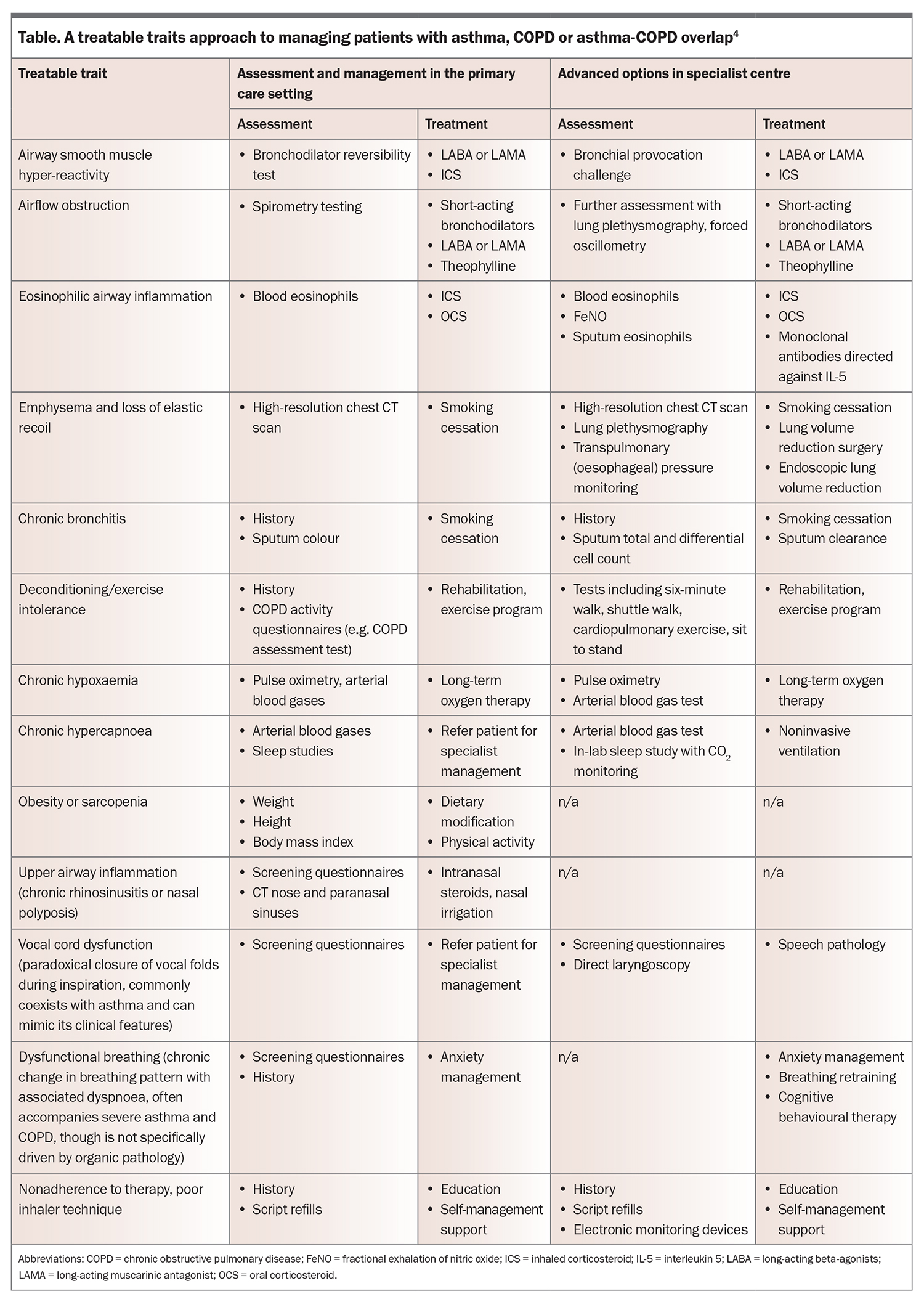
Asthma and COPD are both heterogenous conditions with multiple contributing pathophysiological processes. The classification of patients who display features of both conditions under the umbrella of ACO only risks compounding the complexity of their condition without providing any meaningful value to the individual patient. In 2016, a consortium of physicians proposed that, rather than relying on disease labels for asthma and COPD, they should be viewed as ‘a continuum of different diseases that may share biological mechanisms (i.e. endotypes), and present similar clinical, functional, imaging and/or biological features that can be observed (i.e. phenotypes) which require individualised treatment’.6 In this treatable traits approach, the focus is on identifying disease traits or clinical phenotypes with treatments that specifically target them. Such clinical phenotypes then are not limited to just asthma or COPD. The Table lists some of the traits or phenotypes that may manifest in a patient with asthma, COPD or ACO, and associated management strategies to consider for each.
Adopting a treatable traits approach to the management of the patients in the three case studies (Box 1) is outlined in Box 2. Such an approach emphasises a shift from intensifying treatment targeted towards disease labels, to targeting the treatments to the clinical phenotypes present in the individual patient.
Conclusion
Asthma-COPD overlap describes an important cohort of patients who demonstrate features typically associated with both asthma and COPD. This description is useful on a population level to highlight the complexity of chronic airways disease and the heterogeneity of the individual diagnoses of asthma and COPD. However, ACO is clearly not a disease entity in its own right and attempts to fit a label to patients who demonstrate symptoms of both asthma and COPD, and illustrates the limitations with the current approach to chronic airways disease. As we develop a greater understanding of the mechanisms underlying both asthma and COPD, a focus on treating identifiable clinical traits may offer a more targeted approach to therapies to improve symptoms and disease outcomes with fewer side effects. The management of the individual patient who fits the description of ACO should focus on the traits of chronic airways disease that the patient manifests rather than the disease label. RMT
COMPETING INTERESTS: Dr Cook reports personal fees from GSK, outside the submitted work. Professor Simpson and Professor Wark: None.
References
1. Global Initiative of Chronic Obstructive Lung Disease (GOLD). Global strategy for diagnosis, management, and prevention of chronic obstructive pulmonary disease (2018 Report), 2018. Available online at: https://goldcopd.org/wp-content/uploads/2017/11/GOLD-2018-v6.0-FINAL-revised-20-Nov_WMS.pdf (accessed August 2020).
2. Global Initiative for Asthma. Global strategy for asthma management and prevention (2020 update). Available online at: https://ginasthma.org/reports/ (accessed August 2020).
3. Australian Institute of Health and Welfare (AIHW). Asthma. Cat. no. ACM 33. Canberra: AIHW; 2019. Available online at: https://www.aihw.gov.au/reports/chronic-respiratory-conditions/asthma (accessed August 2020).
4. Toelle BG, Xuan W, Bird TE, et al. Respiratory symptoms and illness in older Australians: the Burden of Obstructive Lung Disease (BOLD) study. Med J Aust 2013; 198: 144-148.
5. National Asthma Council Australia and Lung Foundation Australia. Asthma–COPD overlap. Information paper for health professionals. National Asthma Council Australia, Melbourne: 2017. Available online at: https://www.nationalasthma.org.au/living-with-asthma/resources/health-professionals/information-paper/asthma-copd-overlap (accessed August 2020).
6. Agusti A, Bel E, Thomas M, et al. Treatable traits: towards precision medicine of chronic airways disease. Eur Respir J 2016; 47: 410-419.
7. Sin D, Miravitalles M, Mannino D, et al. What is Asthma-copd overlap syndrome? Towards a consensus definition from a round table discussion. Eur Respir J 2016; 48: 664-673.
8. Global Initiative of Chronic Obstructive Lung Disease (GOLD). Diagnosis of diseases of chronic airflow limitation: asthma, COPD, and asthma-COPD overlap syndrome (ACOS), 2015. Available online at: https://goldcopd.org/wp-content/uploads/2016/04/GOLD_ACOS_2015.pdf (accessed August 2020).
9. Woodruff P, Modrek B, Choy D. T helper type 2-driven inflammation defines major subphenotypes of asthma. Am J Respir Crit Care Med 2009; 180: 388-395.
10. Ray A, Kolls JK. Neutrophilic inflammation in asthma and association with disease severity. Trends Immunol 2017; 38: 942-954.
11. Singh D, Kolsum U, Brightling CE, Locantore N, Agusti A, Tal-Singer R. Eosinophilic inflammation in COPD: prevalence and clinical characteristics. Eur Respir J 2014; 44: 1697-1700.
12. Dey S, Eapen MS, Chia C, et al. Pathogenesis, clinical features of asthma COPD overlap, and therapeutic modalities. Am J Physiol Lung Cell Mol Physiol 2022; 322: L64-L83.
13. Calverley PM, Albert P, Walker PP. Bronchodilator reversibility in chronic obstructive pulmonary disease: use and limitations. Lancet Respir Med 2013; 1: 564-573.
14. Grootendorst DC, Rabe KF. Mechanisms of bronchial hyperreactivity in asthma and chronic obstructive pulmonary disease. Proc Am Thorac Soc 2004; 1: 77-87.
15. Alshabanat A, Zafari Z, Albanyan O, et al. Asthma and COPD overlap syndrome (ACOS): a systematic review and meta-analysis. PLoS One 2015; 10: e0136065.
16. Calverley PM, Anderson JA, Celli B, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med 2007; 356: 775-789.
17. Tashkin DP, Celli B, Senn S, et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med 2008; 359: 1543-1554.
18 Tonnel AB, Perez T, Grosbois JM, et al. Effect of tiotropium on health-related quality of life as a primary efficacy endpoint in COPD. Int J Chron Obstruct Pulmon Dis 2008; 3: 301-310.
19. Bateman E, Reddel H, van Zyl-Smit R, Agusti A. The asthma-COPD overlap syndrome: towards a revised taxononomy of chronic airways disease. Lancet Respir Med 2015; 3: 719-728.
20. Peters SP, Kunselman SJ, Icitovic N, et al. Tiotropium bromide step-up therapy for adults with uncontrolled asthma. N Engl J Med 2010; 363: 1715-1726.
21. Stempel DA, Raphiou IH, Kram KM, et al. Serious asthma events with fluticasone plus salmeterol versus fluticasone alone. N Engl J Med 2016; 374: 1833-1830.
22. Kerstjens HA, Engel M, Dahl R, et al. Tiotropium in asthma poorly controlled with standard combination therapy. N Engl J Med 2012; 367: 1198-1207.
23. Vogelmeier C, Hederer B, Glaab T, et al. Tiotropium versus salmeterol for the prevention of exacerbations of COPD. N Engl J Med 2011; 364: 1093-1103.
24. Pauwels RA, Pedersen S, Busse WW, et al. Early intervention with budesonide in mild persistent asthma: a randomised, double-blind trial. Lancet 2003; 361: 1071-1076.
25. O’Byrne PM, Pedersen S, Busse WW, et al. Effects of early intervention with inhaled budesonide on lung function in newly diagnosed asthma. Chest 2006; 129: 1478-1485.
26. Nelson HS, Weiss ST, Bleecker ER, Yancey SW, Dorinsky PM. The Salmeterol Multicenter Asthma Research Trial: a comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. Chest 2006; 129: 15-26.
27. Castle W, Fuller R, Hall J, Palmer J. Serevent nationwide surveillance study: comparison of salmeterol with salbutamol in asthmatic patients who require regular bronchodilator treatment. BMJ 1993; 306: 1034-1037.
28. Welte T, Miravitlles M, Hernandez P, et al. Efficacy and tolerability of budesonide/formoterol added to tiotropium in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2009; 180: 741-750.
29. Jung KS, Park HY, Park SY, et al. Comparison of tiotropium plus fluticasone propionate/salmeterol with tiotropium in COPD: a randomized controlled study. Respir Med 2012; 106: 382-389.
30. Kew KM, Seniukovich A. Inhaled steroids and risk of pneumonia for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014; 10(3): CD010115.
31. Pavord ID, Chanez P, Criner GJ, et al. Mepolizumab for eosinophilic chronic bbstructive pulmonary disease. N Engl J Med 2017 26; 377:1613-1629.
32. Bhatt SP, Rabe KF, Hanania NA, et al; BOREAS Investigators. Dupilumab for COPD with type 2 inflammation indicated by eosinophil counts. N Engl J Med 2023 20; 389: 205-214.
33. Lee SY, Park HY, Kim EK, et al. Combination therapy of inhaled steroids and long-acting beta2-agonists in asthma-COPD overlap syndrome. Int J Chron Obstruct Pulmon Dis 2016; 11: 2797-2803.