Eye floaters. Usually inconsequential but a big nuisance
Ocular floaters are shadows cast on the retina by clumps of vitreous humor that can develop as a normal consequence of ageing. They are common in people aged 50 to 75 years and are usually benign. Patients with a sudden onset of floaters should be reviewed urgently by an ophthalmologist.
Floaters are small, black, moving shapes that patients report in their vision, typically seen against a bright background. They are caused by opacities in the vitreous that cast shadows on the retina. They stand out when patients look at something bright, such as white paper, a computer screen or a blue sky, and can be quite annoying to the patient. Although floaters can be a sign of serious eye disease, most are benign. Floaters that are bad enough to disturb a patient can be vapourised by laser or removed surgically. This article covers the description, signs, symptoms, evaluation and management of floaters.
What are floaters?
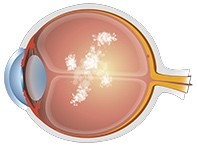
Most floaters are formed by a condensation of collagen and hyaluronic acid (essentially the components of normal vitreous humor, a gel that is transparent in young people1) in the vitreous chamber of the eye. However, floaters can also consist of red blood cells from a vitreous haemorrhage, white blood cells from inflammation, congenital opacities, an operculum from a retinal tear, lens capsular fragments following neodymium: yttrium aluminium garnet (Nd:YAG) laser capsulotomy or fragments of lens material left behind after cataract surgery. This article focuses on benign collagen floaters.
Floaters earn their name by moving around in the eye. They tend to dart away with eye movement and then slowly drift back to their resting position. Sometimes they are relatively stationary. They can appear to have many different shapes: dots, rings, insects, squiggly lines, strings of pearls, cobwebs (Figure 1) or clouds (Figure 2). Reported shapes are limited only by patients’ imaginations (Figure 3).
The Latin medical term for floaters is muscae volitantes, which translates as ‘flying flies’, and the Greek is myodesopsia (‘seeing fly-like bodies’).
As the eye ages, the collagen substance that makes up the vitreous shrinks down to leave little shreds that clump together. The patient sees the shadows these clumps cast on the retina as floaters. Floaters can occur with or without a vitreous detachment but most commonly happen after vitreous detachment, a separation of the outer part of the vitreous gel from the retina. Vitreous detachment is a common occurrence as the eye ages, and should not be confused with a retinal detachment.
A posterior vitreous detachment that takes with it the fibrous annulus of vitreous cortex around the head of the optic nerve leaves a skewed round floater in the vitreous cavity. This is known as a Weiss ring (Figure 4).
Presentation
Floaters can present at any age, but typically present between the ages of 50 and 75 years. Floaters are more common in short-sighted (myopic) eyes and eyes that have had cataract surgery. Floaters associated with a vitreous detachment can occur after ocular or head trauma.
Patients typically present with symptoms of ocular flashes as well as floaters. Patients often report seeing streaks or flashes of light at night and little black spots and grey shadows the next day.
If the onset of floaters is acute, the patient should be referred to an ophthalmologist immediately because this is a sign of retinal tear or retinal detachment. Only an examination can distinguish these from a simple posterior vitreous detachment. Most ophthalmologists would see a patient who had an acute onset of flashes and floaters within a day or so.
Examination
Visual acuity is usually unaffected. The eye appears normal on external examination. The pupil must be dilated for adequate visualisation of the floaters and, more importantly, the surrounding retina. Dilated fundus examination may reveal a posterior vitreous detachment with or without retinal problems, such as traction on the retina from an incompletely detached vitreous, retinal haemorrhage, retinal tears or a retinal detachment.
Management
If a retinal tear is detected, retinal laser photocoagulation is applied around it. A very anterior (peripheral) tear can be difficult to reach through the contact lens (fundus lens) used in retinal photocoagulation, so external scleral cryotherapy may be used.
If a retinal detachment has happened, treatment options include argon laser photocoagulation and retinal surgery.
With a healthy retina, symptoms of floaters will usually improve in the first few weeks after symptom onset. Patients should be re-examined a few weeks later by an ophthalmologist or an optometrist with the correct skills. The typical scenario is that the flashes have stopped but the floaters persist. Floaters will sometimes improve with time, especially those that have a haemorrhagic component. Symptomatic floaters often improve with gravitation away from the visual axis (they physically sink to the bottom of the vitreous chamber and can be stirred up with head movements or by being upside down) and neuroadaptation (the visual system just learns to ignore them).
Treatment for floaters that annoy the patient
Patients who present to their optometrist or ophthalmologist complaining of persistent floaters are often told simply to ignore them. They might also be told that there is nothing that can be done.
In fact, there are several therapeutic options for stubborn floaters that interfere with vision. The definitive treatment is pars plana vitrectomy.1,2 Vitrectomy can be associated with increased risk of cataractogenesis, but this risk is reduced in modern, limited vitrectomy.1 However, most retinal specialists would recommend against vitrectomy for floaters in the absence of other pathology.
Nd:YAG laser vitreolysis is a less invasive alternative, but has not been tested as rigorously as vitrectomy. This treatment is not new. First described in 1985, the procedure has been hampered by problems in aligning the laser’s illuminating light source with the path of the laser beam.3,4 The goal of treatment was to break floaters into smaller fragments rather than to vapourise them.3 The reason for this is that it is much more difficult to vapourise a floater when using a laser beam with the illumination source coming in from the side.
A new Nd:YAG laser design allows superimposition of the viewing, lighting and treating axes. This type of Nd:YAG laser breaks down vitreous opacities, converting them to gas that leaves the eye via the retinal venous vasculature.
Does laser help in all cases of floaters?
Nd:YAG laser vitreolysis is more effective for some types of floaters than others. The floaters that respond best to laser treatment are:
- easily visualised with a biomicroscopy lens (such as a 90D or a 78D) at the slit lamp, with the patient looking straight ahead (as opposed to floaters further out in the periphery, which can be seen only at the extremes of ocular gaze)
- isolated and well circumscribed (rather than diffuse, fluffy or cloudy opacities)
- not too close to the posterior lens capsule (in an eye with the natural lens in place) or to the macula.
How is the procedure performed?
Nd:YAG laser vitreolysis is performed in a clinic setting, much like Nd:YAG laser capsulotomy. No sedation is needed and the patient is treated sitting up, with their chin on a rest and forehead pressed forward against a rest, in a position similar to that used for slit lamp examination. The patient’s pupil must be maximally dilated. Topical anaesthesia is used to allow a contact lens to be placed on the eye, but the procedure itself is painless. The contact lens is a fairly bulky, hand-held instrument that is pressed against the eye during the procedure. It takes about 10 to 15 minutes.
To see the procedure being performed go to http://vitreousfloatersolutions.com.
What are the risks?
Nd:YAG laser vitreolysis can cause damage to the crystalline lens (causing an instant cataract), hit the retina (causing a retinal burn) or increase intraocular pressure.5,6
Pseudophakic eyes (eyes in which the natural lens has been replaced with an intraocular lens) appear to be most at risk of a rise in intraocular pressure following vitreolysis, particularly if they have had a posterior capsulotomy previously or if one occurs at the time of vitreolysis (author’s personal observation). The mechanism that causes the increase in intraocular pressure is unknown. One possibility is thought to be migration of micro debris into the anterior chamber during vitreolysis.7
Retinal detachment has been reported with use of Nd:YAG laser in the vitreous chamber, although not in the treatment of floaters.6 In experienced hands the most likely risk of Nd:YAG laser vitreolysis is that some persistent floaters remain, leading to suboptimal patient satisfaction.
The long-term risks of Nd:YAG laser vitreolysis are not known.
What is required after laser treatment?
Topical anti-glaucoma medications are started immediately after the procedure to reduce the risk of an increase in intraocular pressure.
Intraocular pressure should be checked and any persisting floaters reviewed a week after surgery and, if possible, a month later, because rises in intraocular pressure can be delayed.7
Nd:YAG laser vitreolysis: the good and the bad
Knowing the benign nature of floaters, optometrists and ophthalmologists often dismiss them unempathetically, particularly because visual acuity – as judged by traditional Snellen chart testing – is unaffected.
However, symptomatic floaters are now recognised to be more prevalent and have greater negative impact on patients’ quality of life than was previously understood.1 Evidence suggests that contrast sensitivity is reduced and straylight is increased in the eyes of patients who report bothersome floaters.1 Both Nd:YAG laser vitreolysis and pars plana vitrectomy targeted at floaters can be life-changing for patients.
Sadly, some patients can become obsessed by their floaters, and pursue treatment at practices that offer Nd:YAG laser vitreolysis even after large floaters in the visual axis have been vapourised. Sometimes the ophthalmologist cannot see the floater, even those reported to be in the centre of their visual field. Patients who focus on tiny little opacities are often disappointed by any treatment available to them. Clinicians should consult on several occasions with patients who are bothered by ocular floaters, to determine appropriate suitability for therapy.1 Fortunately, some objective clinical measures have become available to determine the severity of floaters, based on both structural (ultrasonography) and functional (contrast sensitivity and straylight testing) criteria.1
Conclusion
Ocular floaters are opacities in the vitreous chamber of the eye that can be greatly irritating to patients and may affect quality of vision and life. They do not require treatment unless the patient is truly bothered by them. Pars plana vitrectomy remains the definitive treatment for ocular floaters. Nd:YAG laser vitreolysis can be considered as a possible alternative to provide symptom relief from troublesome floaters in many patients. Laser success can be maximised by careful patient selection. MT