Allergic conjunctivitis: subtypes and management strategies

Allergic conjunctivitis is a common chronic disease, particularly in childhood, and often presents in general practice as a recurrent red eye. Allergic conjunctivitis is underdiagnosed and suboptimal treatment can result in potentially hazardous consequences to vision. Treatment of allergic eye disease involves a stepwise approach of minimisation strategies, nonpharmacological interventions and pharmacological treatments.
- Allergic diseases affect one in five people in Australia and are more common in children. People who experience allergic conjunctivitis report adverse effects of this condition on their quality of life.
- The most common type of allergic conjunctivitis is seasonal allergic conjunctivitis.
- Itching is the hallmark symptom of ocular allergy. If it is not a prominent symptom, the diagnosis of a red eye should be reconsidered.
- Rarer and more severe forms of ocular allergies that may threaten vision include atopic keratoconjunctivitis and vernal keratoconjunctivitis.
- Topical mast-cell stabilisers are the mainstay of treatment in managing ocular allergy; however, there are new management strategies to consider in refractory cases.
- There is no role for corticosteroids in treating patients with seasonal or perennial allergic conjunctivitis. The use of corticosteroids in other forms of allergic disease should always be under the supervision of an ophthalmologist, due to the potential of adverse effects.
Only a small proportion of individuals with allergic disease tend to seek help, despite it affecting one in five people in Australia.1 One of the most common allergic diseases is allergic conjunctivitis, affecting about 10% of people in Australia, with 80% of cases occurring in patients under 30 years of age.1,2 Although symptoms are often considered minor, allergic eye disease tends to have a chronic course with multiple recurrent episodes. There are well-established links between allergic conjunctivitis and other atopic conditions, such as asthma, rhinitis, eczema, food allergy and eosinophilic oesophagitis. Most patients with allergic conjunctivitis experience concomitant allergic rhinitis, with only 6% of patients experiencing isolated ocular symptoms.3
Patients with allergic conjunctivitis experience negative impacts on their quality of life, including tiredness, loss of productivity in work and school and adverse effects on mental health.4 Specific indicators of this include poor quality sleep and emotional distress due to unrelenting symptoms. There is also a significant economic cost to the healthcare system and an added financial burden of treatment to individuals.4
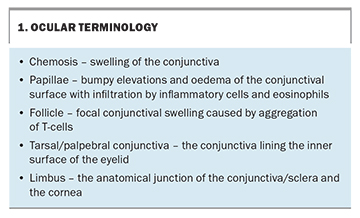
Less common but more severe forms of ocular allergy can threaten vision, such as vernal keratoconjunctivitis (VKC) and atopic keratoconjunctivitis (AKC). A good working knowledge on the spectrum of ocular allergic disease will facilitate GPs in managing routine cases and identifying complex presentations requiring referral for specialist care. Common ocular anatomy and pathology is described in Box 1.
Classification of ocular allergic disease
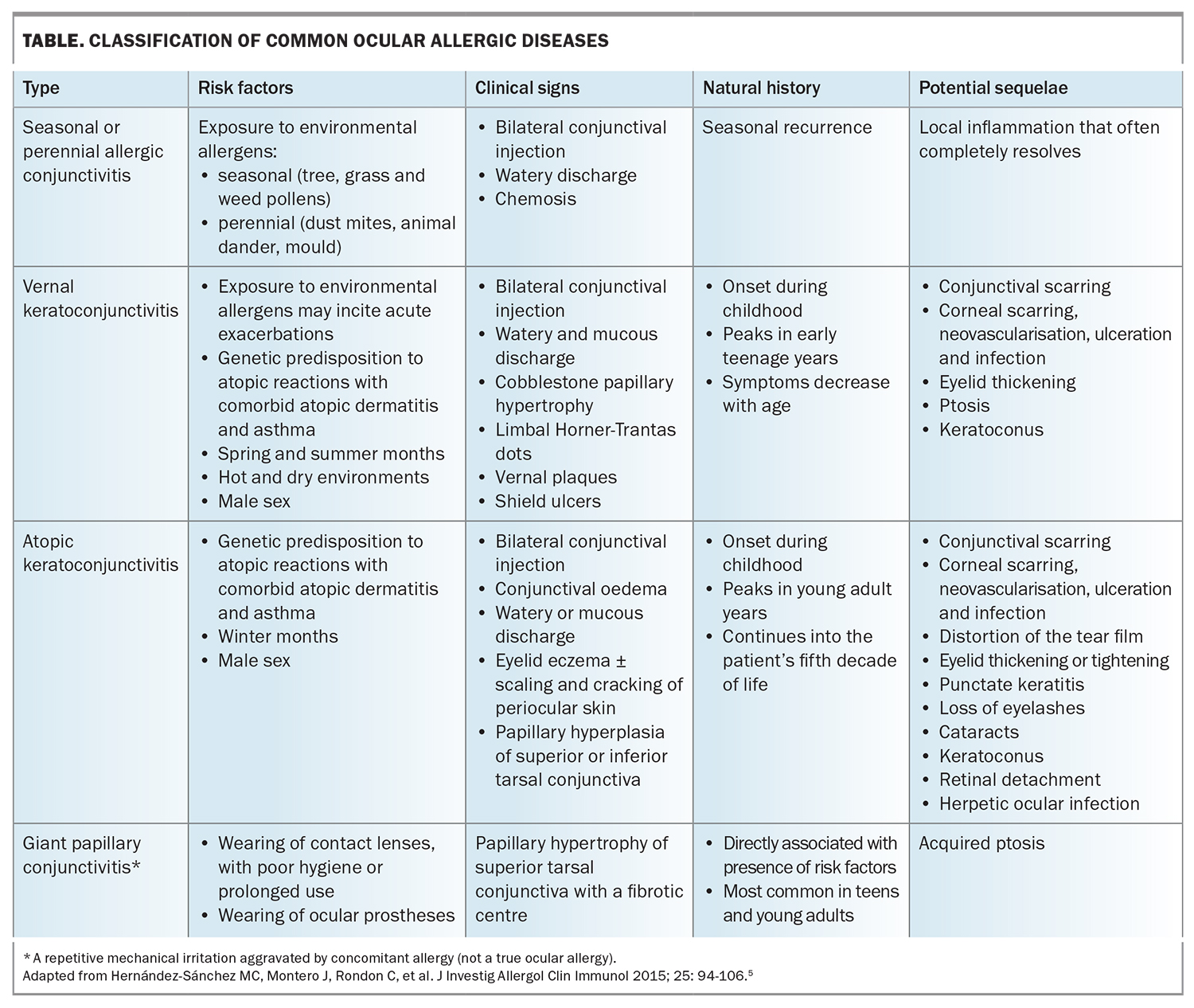
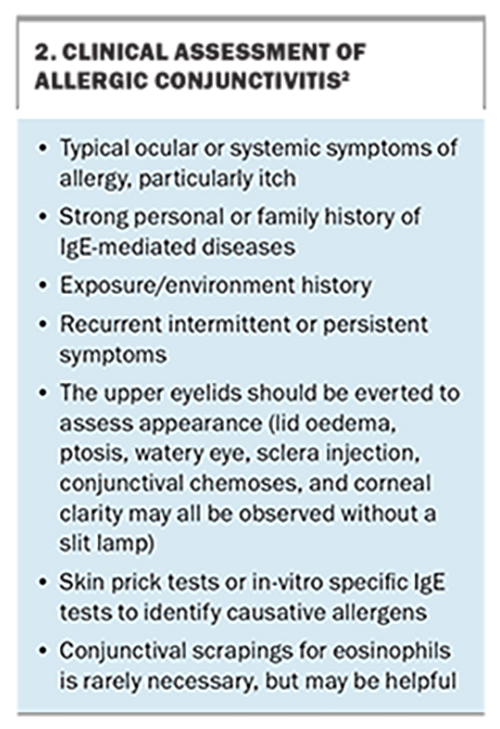
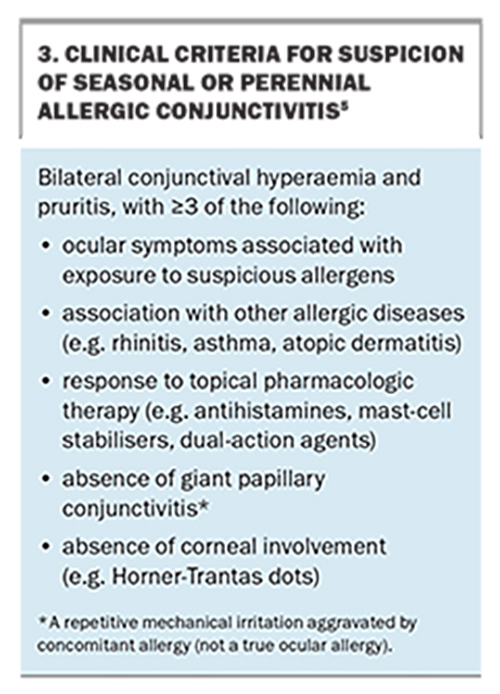
Ocular allergic disease covers a broad group of conditions, as shown in the Table. Simple acute allergic conjunctivitis is either seasonal or perennial. In regard to pathophysiology and treatment, there is considerable overlap with chronic, immune-mediated forms of conjunctivitis (VKC and AKC) and giant papillary conjunctivitis. Despite the similarity in initial treatment, the outcomes and rates of complications differ between subtypes. Assessment of allergic conjunctivitis is described in Box 2 and criteria for diagnosing allergic conjunctivitis are detailed in Box 3. All forms of ocular allergic disease have distinct clinical features and natural histories.
Acute allergic conjunctivitis
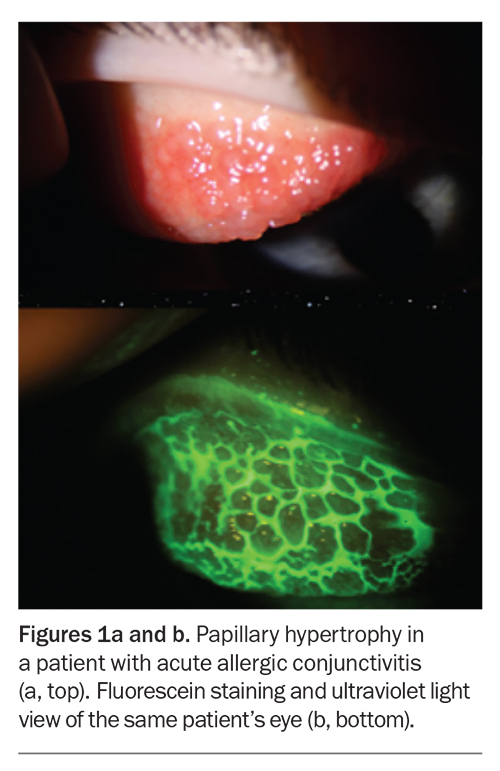
Acute allergic conjunctivitis occurs at a hyperacute rate and is self-limiting, with resolution typically occurring within 24 hours.2 Symptoms result from inoculation of the conjunctival sac by exposure to allergens (Figure 1). Acute allergic conjunctivitis can occur at any age but is most common in childhood. Symptoms include mild to debilitating pruritis, chemosis and periorbital oedema. Tearing, redness, foreign body sensation and mucous discharge may also occur. Occasionally, the eyelids may be swollen shut due to oedema. Acute conjunctivitis is further categorised as seasonal or perennial, with the former being more common. The difference between the two entities is the chronicity of symptoms, dictated by individual patient sensitivity to various allergens. It is important to note that the patient may be asymptomatic at the time of presentation; therefore, it is important to ask about the time of year when symptoms are at their worst.
Seasonal allergic conjunctivitis
Seasonal allergic conjunctivitis is the most common type of ocular allergy. 5,6 Seasonal symptoms are triggered by fluctuating levels of aerosolised allergens, such as tree or grass pollens. This contrasts with perennial symptoms, which are caused by indoor allergens. The disease is most common in spring and autumn and there is often a history of other atopic diseases, such as eczema, asthma or allergic rhinitis. History-taking and examination should assess for family history of atopic comorbidities, as well as symptoms and signs of other common allergic processes.
Itchy and watery eyes often occur with nasal or pharyngeal symptoms and are a prominent feature in seasonal exacerbations. On examination, the conjunctiva is often mildly injected and may be swollen with low-grade papillary hypertrophy (Figure 1). There can be oedema of the eyelids, which is usually mild and does not diminish the patient’s vision. Symptoms are usually bilateral.Pain is not usually a symptom of simple allergic conjunctivitis and should alert the GP to more sinister pathology.
Perennial allergic conjunctivitis
Perennial allergic conjunctivitis is similar to seasonal allergic conjunctivitis but symptoms persist throughout the year. Perennial allergic conjunctivitis is due to chronic exposure of the eyes to allergens, such as house dust mites, animal dander, mould spores, rodents and feathers. Seasonal exacerbations are common, which can make it challenging to distinguish from seasonal conjunctivitis.6
Vernal keratoconjunctivitis
VKC is a more severe form of ocular allergy and, in rare cases, can lead to vision loss. VKC is also known as ‘spring catarrh’ and is clinically distinct from perennial or seasonal allergic conjunctivitis. The aetiology is not well understood but is thought to be due to a combination of climate and allergen exposure. It is more common in males than females (3:1) and children under 10 years of age. About 50% of patients who experience VKC have a coinciding history of asthma or atopy. VKC exhibits seasonal variation, is more severe in arid dry climates and has a clinical course of two to 10 years. Many patients have complete resolution without any symptoms after adolescence; however, about 5% of patients will develop AKC.5
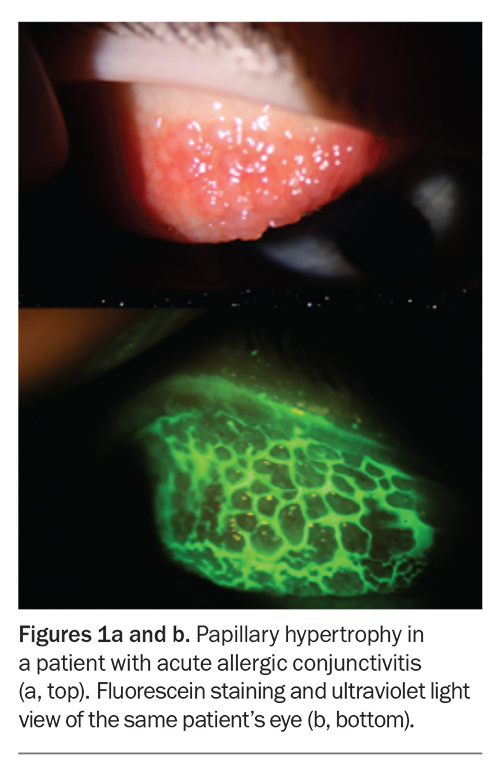
In VKC, patients experience intense itching, photophobia and tearing. Clinical signs include a ropy, mucous discharge, upper eyelid swelling with large cobblstone-like papillae of the superior palpebral conjunctiva visible on lid eversion (Figure 2) and Horner-Trantas dots (off-white deposits at the limbus that consist of eosinophils and cellular debris).
Corneal involvement may occur in severe cases, which is caused either by inflammatory mediators produced by eosinophils or by direct mechanical trauma of the inflamed papillary changes on the conjunctival surface. Corneal involvement ranges from a mild punctate keratitis to a shield ulcer (named for its shape). Shield ulcers can scar and commonly require debridement by an ophthalmologist. Patients often require specific therapy that may include topical corticosteroids, topical ciclosporin or subtarsal triamcinolone to reduce conjunctival papillary inflammation, so early referral is imperative. VKC may be associated with the development of keratoconus, particularly due to chronic eye rubbing.7 Patients should be strongly advised against rubbing their eyes.
Atopic keratoconjunctivitis
AKC is a chronic, bilateral conjunctivitis associated with atopic dermatitis of the eyelids. Of the 3% of the population with atopic dermatitis, up to 25% will develop some degree of ocular involvement. A correct diagnosis of this condition is important as it can be associated with significant ocular morbidity.8
AKC usually occurs in patients between 30 and 50 years of age. It is also more common in men and tends to be perennial, with potential exacerbations in winter. Severe itching of both the ocular surface and eyelids is the hallmark symptom and may be debilitating. Clinical signs in the skin usually precede ocular involvement and include significant hyperaemia and oedema of the conjunctiva, scaling and cracking of the periocular skin and fine papillary hyperplasia (which tends to be more marked in the inferior regions). Corneal scarring and neovascularisation can occur in severe cases due to corneal inflammation, as well as disturbance of the tear film, subconjunctival scarring and distortion of the lid margin.
About 5 to 10% of patients with AKC will develop a cataract as a result of their condition.8 These patients are also at risk of other ocular disorders, such as keratoconus, retinal detachment and herpetic ocular infection.
Giant papillary conjunctivitis
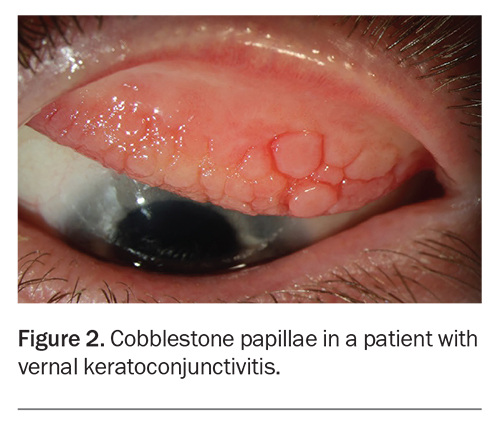
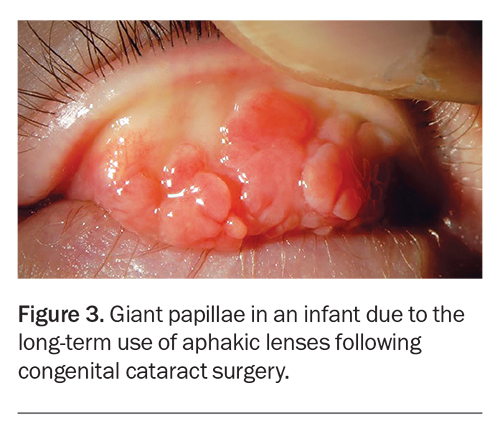
Giant papillary conjunctivitis occurs most commonly in teens and young adults, usually due to long-term contact lens use. The reaction of the superior tarsal conjunctiva to chronic exposure of contact lenses or foreign bodies results in papillary hyperplasia (Figure 3). It may also occur with ocular prostheses or following ocular surgery due to filtration blebs or loose or eroding sutures. Symptoms include itching, tearing, increased mucous production and ocular discomfort.
Differential diagnoses
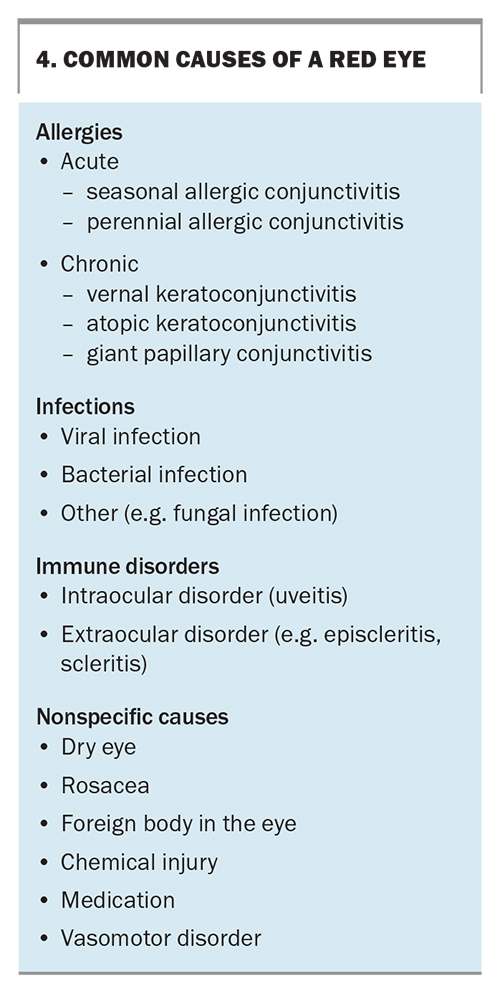
The causes of an acute red eye are varied (Box 4). Itch is the hallmark symptom of all ocular allergies. Any patient with uncontrolled ocular pain or reduced vision warrants an urgent referral to an ophthalmologist, as these symptoms may suggest raised intraocular pressure from acute glaucoma, inflammation from uveitis or an infection of the cornea (e.g. microbial keratitis). Infections are particularly common in contact lens wearers.5 The use of topical corticosteroids should be avoided in patients with an acute, red eye, unless comanaged with an ophthalmologist and especially if there is any suspicion of infection.3,5
Pathogenesis of ocular allergy
The ocular mucosa has a large surface area, mainly composed of the palpebral and bulbar conjunctiva. It is one of the most exposed and accessible sites with a dense population of mast cells and lymphocytes, allowing direct antigen deposition and leading to the initiation of the allergic cascade.
Seasonal allergic conjunctivitis and perennial allergic conjunctivitis are the only ocular conditions known to involve solely type 1 hypersensitivity reactions. In individuals who have previously been sensitised, immune cells release inflammatory cytokines that stimulate immunoglobulin E (IgE) production by B cells, resulting in the IgE binding to mast cells. Subsequent cross-linking by allergens triggers mast-cell degranulation and release of histamine and other inflammatory mediators. Airborne allergens typically contact the conjunctiva via the tear film. The early phase of the allergic cascade usually begins within seconds to minutes after allergen exposure and will clinically last 20 to 30 minutes.2,6,8 These changes result in vasodilation, oedema and the recruitment of other inflammatory cells (e.g. eosinophils). The late phase begins a few hours later. Activation of the cyclo-oxygenase pathway and lipoxygenase pathway triggers the release of prostaglandins, thromboxanes and leukotrienes, which attract additional inflammatory cells, leading to continued inflammation, persistent symptoms and increased changes associated with tissue damage. Progression results in hypersecretion of tears that increases drainage through the lacrimal ducts, carrying allergens directly into the nasal passage.
AKC and VKC involve a more complex pathogenesis of mixed type 1 and type 4 (cell-mediated) hypersensitivity.2,6-8 There are published reports of their association with IgE-mediated atopic disease but the association is not necessarily causal.2 There is a plethora of increased cytokines and chemokines in VKC and AKC compared with seasonal allergic conjunctivitis and giant papillary conjunctivitis.11 There is florid infiltration of CD4 T-cells, eosinophils and mast cells, which leads to chronic inflammation with fibrosis and tissue destruction.
Giant papillary conjunctivitis is not a true ocular allergy but is instead a repetitive mechanical irritation aggravated by concomitant allergy. Mixed populations of inflammatory cells are produced in response to a foreign body, with elements of a hypersensitivity reaction and chronic inflammation. However, the reaction usually resolves after the inciting foreign body is removed.
Treatment
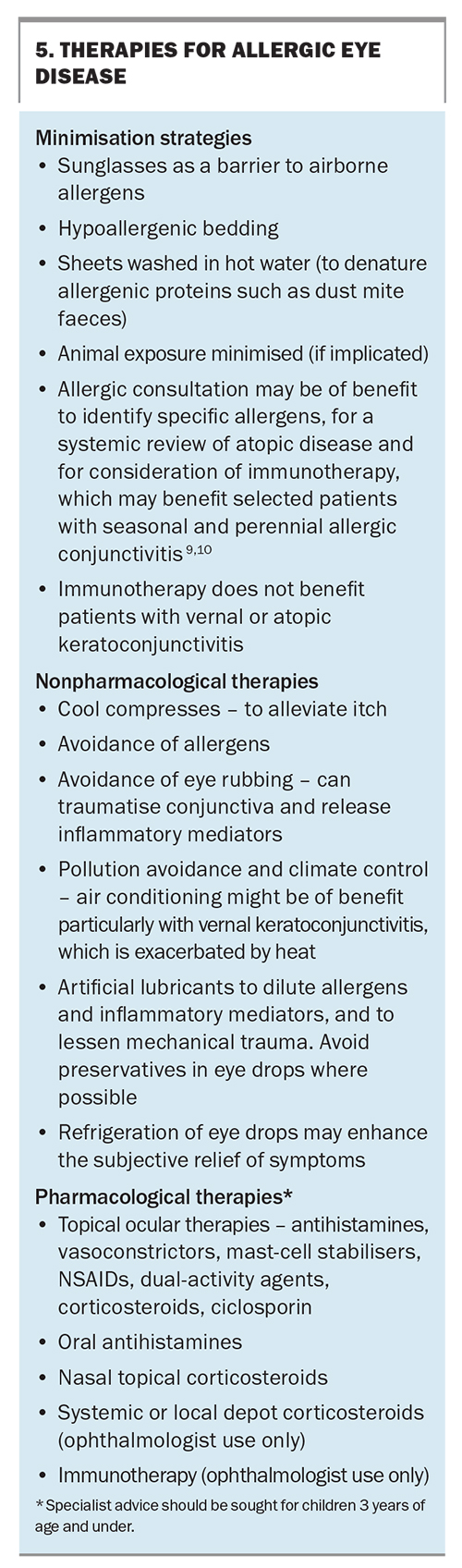
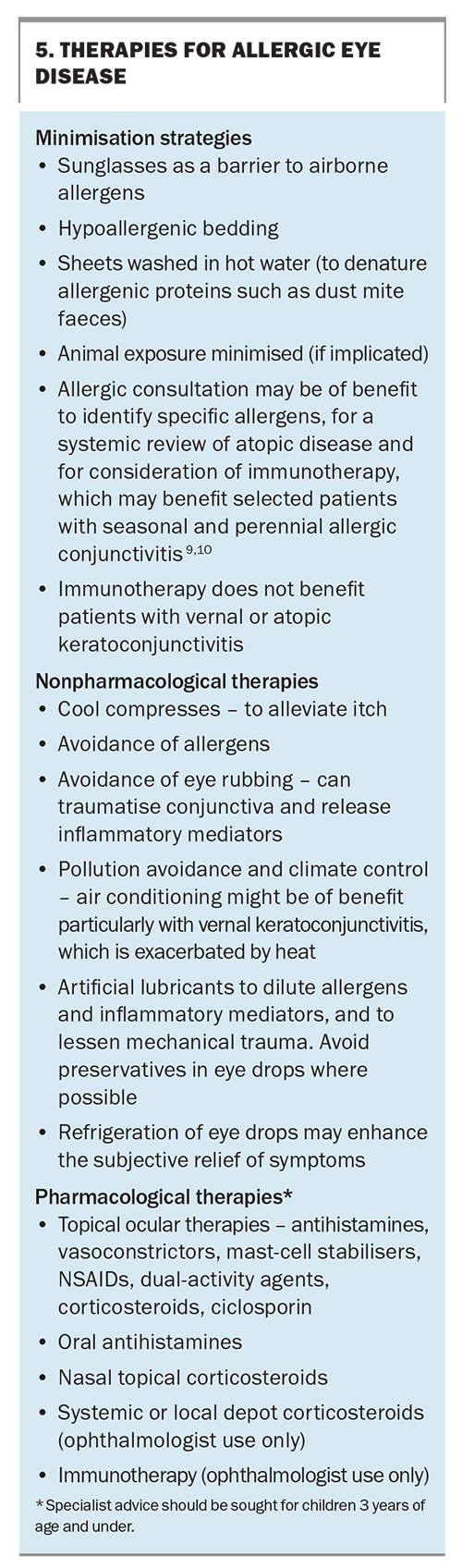
Treatment of allergic eye disease involves a stepwise approach of minimisation strategies, nonpharmacological interventions and pharmacological treatments (Box 5). Although initial treatments are often empiric, selecting therapies that are tailored to the patient’s symptoms can improve adherence and the response to treatment. Specialist advice should be sought for the treatment of children under 3 years of age as most pharmacological treatments for allergic conjunctivitis are contraindicated in this age group. All patients should be educated about good general eye care for allergic conditions and discouraged from rubbing their eyes, as it causes mast-cell degranulation and worsening of symptoms.12 Patients should also be advised to frequently apply artificial tears and cool compresses. Known allergen exposures should be avoided and contact lenses should be removed (if applicable). Patients should be asked about allergies to cosmetics and other eye medications and the use of low allergenic cosmetics can be helpful.
Patients with giant papillary conjunctivitis will respond best to the removal of the offending foreign body, in conjunction with the measures described in Box 5. If the patient’s condition is related to chronic contact lens use, changing the lens type or the cleaning solution can be beneficial. Patients should be recommended to have a break from wearing contact lenses.
Antihistamines
Both topical and oral antihistamines can be used with good effect. First-generation oral antihistamines should be avoided as they produce anticholinergic side effects, such as confusion, sedation, urinary retention, constipation, dry eyes and dry mouth.5
Topical antihistamines target the ocular tissues directly and, as such, have a faster onset of action and are better tolerated with fewer side effects. Mild symptoms of itch and erythema are relieved with regular instillations of drops (up to four times a day). Improved control can be achieved by a combination of short-term topical vasoconstrictive and antihistamine therapies, such as naphazoline plus antazoline, naphazoline plus pheniramine or naphazoline plus hamamelis extract. It is important to note that chronic use of vasoconstrictors can lead to tachyphylaxis and rebound hyperaemia or vasodilation when discontinued.5
Topical mast-cell stabilisers and dual-activity agents
Topical dual-activity agents have the combined properties of antihistamines and mast-cell stabilisers. They are clinically superior to and better tolerated than topical mast-cell stabilisers or antihistamines, alone, and should be considered first-line treatment. Immediate relief is provided by antihistamines and prophylactic effects are achieved by mast-cell stabilisers, with some inhibition of eosinophil migration and other mediators of inflammation.3,12 Dual-activity agents have largely replaced topical mast-cell stabilisers alone, such as levocabastine, sodium cromoglycate and antihistamines. They are best used on a prophylactic basis and require a loading period of several weeks prior to allergen exposure.
Olopatadine and ketotifen have multiple actions as mast-cell stabilisers, anti-inflammatory agents and selective H1-antagonists. Olopatadine 0.1% and ketotifen 0.025% are the mainstays of treatment for most ocular allergic diseases and their use is supported by extensive clinical research and experience. Ocular surface toxicity can occur in rare cases due to benzalkonium chloride (a surfactant preservative), so drops should be instilled 30 minutes prior to contact lens use or after removal and should not be applied while the patient is wearing contact lenses.3 Ketotifen is also available in a preservative-free form.
Olopatadine and ketotifen alleviate acute itch and prevent mast-cell degranulation as a delayed effect after one to two weeks of use.6 The symptoms of seasonal allergic conjunctivitis and perennial allergic conjunctivitis are often controlled with these agents alone. Olopatadine and ketotifen can be used safely throughout the year in patients with perennial allergic conjunctivitis or AKC and can be discontinued over autumn and winter in patients with seasonal allergic conjunctivitis and VKC.
There are no conclusive data in randomised controlled trials to suggest clinical superiority of olopatadine over ketotifen, or vice versa. Alcaftadine, a newer topical antihistamine that is not yet available in Australia, has shown superiority to olopatadine in reducing ocular itch.13
Topical NSAIDs
Topical NSAIDs may be useful when the patient’s symptoms are inadequately controlled despite the use of dual-activity agents or when the prescription of topical corticosteroids is not suitable. Topical NSAIDs inhibit the production of prostaglandins by blocking the cyclo-oxygenase pathway in IgE-mediated allergic responses. The main benefit is the temporary relief of severe symptoms of discomfort. Examples of topical NSAIDs used in ocular allergies include ketorolac trometamol, diclofenac sodium and nepafenac. These drugs can reduce histamine-invoked pruritus, ocular itch and hyperaemia associated with seasonal allergic conjunctivitis.6 Unlike corticosteroid agents, they do not mask ocular infection, affect wound healing or increase intraocular pressure. They may have an analgesic effect but can cause significant irritation due to toxicity and superficial keratitis, particularly in patients with a compromised ocular surface.14 Corneal melting, leading to corneal perforation and vision loss, is rare with the use of topical NSAIDs.15
Topical corticosteroids
Corticosteroids can treat allergic conjunctivitis by reducing cytokine production, mast-cell proliferation, and cell-mediated immune responses. Although effective, they are recommended for short-term treatment only due to the risk of cataract development, elevated intraocular pressure, ocular infection, corneal stromal melting and delayed healing.3 Their use should be restricted to short periods of two to three weeks and only when the diagnosis is certain. Topical corticosteroids should be prescribed under the supervision of administration by an ophthalmologist for the monitoring of potential side effects and the patient’s response to therapy.
Topical corticosteroids (e.g. fluorometholone, dexamethasone and prednisolone) are prescribed in conjunction with dual-activity agents when symptoms and signs are severe or unresponsive to conventional treatment. They are most useful for the control of VKC and AKC and are rarely indicated in the treatment of acute seasonal or perennial allergic conjunctivitis.2
Corticosteroids may also be administered systemically or as a local, subconjunctival depot injection in cases of uncontrolled VKC or AKC that require administration by ophthalmologist. Intranasal corticosteroids used for allergic rhinitis (e.g. fluticasone) have been shown to have positive effects on some ocular allergic symptoms compared with placebo.3
Other immunomodulating agents
Severe and chronic cases of allergic ocular disease that do not respond to conventional therapies may require other immunomodulating agents. The WHO recommends allergen-specific immunotherapy as an effective approach in patients with allergic diseases, such as rhinoconjunctivitis and asthma.2,5 Specialist supervision is imperative. Topical ciclosporin 0.05% or newer high-dose formulations (e.g. ciclosporin 0.09% or ciclosporin 0.1%) are potent steroid-sparing agents and may be useful for AKC and VKC as they are T-cell-driven, chronic inflammatory processes.6 Controlled trials of topical 0.05% topical ciclosporin A have demonstrated clinical safety and improvement in signs and symptoms of AKC and VKC.16,17 These medications are PBS listed for chronic severe dry eye disease with keratitis in patients aged 18 years and older and can only be prescribed by an ophthalmologist or optometrist. Dosages can be increased if the patient becomes resistant to lower doses. Systemic ciclosporin has a significant side effect profile, but can be used as a steroid-sparing agent in selected patients.
Monoclonal antibodies
Although not approved for allergic eye disease, monoclonal antibodies for other systemic allergic disorders (e.g. omalizumab) can provide significant relief of ocular symptoms in some patients with allergic conjunctivitis.3,18 Research into newer monoclonal antibodies for allergic conjunctivitis is promising, with several Phase 1b studies showing favourable outcomes. However, various adverse ocular symptoms have also been observed in clinical trials and off-label use studies.19
Ocular allergies in pregnancy
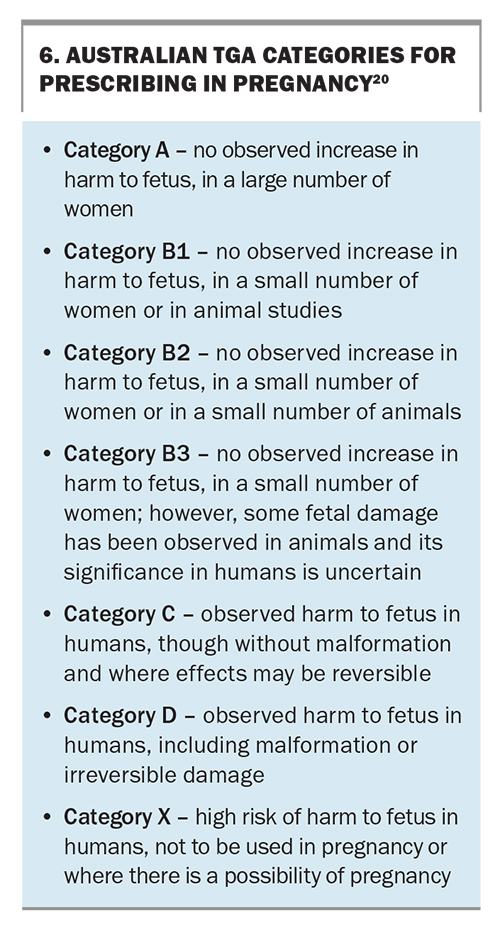
There are no adequate well-controlled studies in pregnant and breastfeeding women for the use of most ophthalmic antihistamines; however, olopatadine and ketotifen are listed under pregnancy category B1 and both can be used during breastfeeding. The topical corticosteroid fluorometholone is listed under pregnancy category B3, but stronger topical corticosteroids are pregnancy category C. TGA categories for prescribing in pregnancy are outlined in Box 6.20
When to refer
Patients should be referred urgently to an ophthalmologist in the following scenarios:
- the patient experiences any reduction in vision
- the diagnosis of a red eye is uncertain
- there is a poor response to recommended supportive measures, such as artificial tears or lubricants and antihistamines or vasoconstrictors, or mast-cell stabilisers
- the severity of allergic disease is significant enough to warrant the consideration of topical corticosteroids
- the patient has a vision-threatening diagnosis, such as AKC, VKC or giant papillary conjunctivitis.
An allergist should be involved early to assess for systemic atopic conditions, identify offending allergens (with or without patch testing) and consider immunotherapy in severe cases of perennial allergic conjunctivitis and seasonal allergic conjunctivitis that are unresponsive to conservative measures.
Conclusion
Allergic eye diseases are highly prevalent in Australia but continue to remain underdiagnosed and undertreated with patients presenting late after failing conservative measures. There are many pharmacological options available and the choice of therapy should be tailored to the individual patient. Potent topical mast-cell stabilisers have greatly improved the management of allergic conjunctivitis. GPs, ocular specialists and allergists can work collaboratively to optimise patient management and prevent vision-threatening complications from more severe forms of allergic disease and from the inappropriate use of corticosteroids. MT
COMPETING INTERESTS: Dr Klejn: None. Professor McCluskey has received honoraria and has worked as a consultant for Allergan, Alcon Laboratories, Pfizer and Bausch & Lomb.
ACKNOWLEDGEMENTS: The authors thank Dr Robin Abell and Ms Jillian Campbell for kindly providing the clinical images.
References
1. Allergy and immune diseases in Australia (AIDA) report 2013. Australasian Society of Clinical Immunology and Allergy; 2013. Available online at: https://www.allergy.org.au/images/stories/reports/ASCIA_AIDA_Report_2013.pdf (accessed November 2023).
2. Katelaris C, Smith P. Ocular allergy. Westmead: World Allergy Organization; 2020. Available online at: https://www.worldallergy.org/education-and-programs/education/allergic-disease-resource-center/professionals/ocular-allergy (accessed November 2023).
3. Dupuis P, Prokopich CL, Hynes A, Kim H. A contemporary look at allergic conjunctivitis. Allergy, Asthma & Clin Immunol 2020: 16, 5.
4. Katelaris CH, Sacks R, Theron PN. Allergic rhinoconjunctivitis in the Australian population: burden of disease and attitudes to intranasal corticosteroid treatment. Am J Rhinol Allergy 2013; 27: 506-509.
5. Hernández-Sánchez MC, Montero J, Rondon C, et al. Consensus document on allergic conjunctivitis (DECA). J Investig Allergol Clin Immunol 2015; 25: 94-106.
6. Bielory L. Allergic inflammation of the anterior surface of the eye. Allergy Asthma Proc 2020; 41: 449-453.
7. Wakefield D, McCluskey P. Vernal keratoconjunctivitis. Med J Aust 2006; 185: 523.
8. Chen JJ, Applebaum DS, Sun GS, Pflugfelder SC. Atopic keratoconjunctivitis: a review. J Am Acad Dermatol 2014; 70: 569-575.
9. Kruse K, Gerwin E, Eichel A, Shah-Hosseini K, Mösges R. Conjunctival provocation tests: a predictive factor for patients’ seasonal allergic rhinoconjunctivitis symptoms. J Allergy Clin Immunol Pract 2015; 3: 381-386.
10. Nofar K, Bielory L. The allergic eye: recommendations about pharmacotherapy and recent therapeutic agents. Curr Open Allergy Clin Immunol 2020; 20: 414-420.
11. Cook EB. Tear cytokines in acute and chronic ocular allergic inflammation. Curr Opin Allergy Clin Immunol 2004; 4: 441-445.
12. Baab S, Le PH, Kinzer EE. Allergic conjunctivitis. Treasure Island: StatPearls Publishing; 2022. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK448118/ (accessed November 2023).
13. Kam KW, Chen LJ, Wat N, Young AL. Topical olopatadine in the treatment of allergic conjunctivitis: a systematic review and meta-analysis. Ocular Immunol Inflam 2017; 25: 663-677.
14. Lee JS, Kim YH, Park YM. The toxicity of nonsteroidal anti-inflammatory eye drops against human corneal epithelial cells in vitro. J Korean Med Sci 2015; 30: 1856-1864.
15. Rigas B, Huang W, Honkanen R. NSAID-induced corneal melt: clinical importance, pathogenesis, and risk mitigation. Surv Ophthalmol 2020; 65: 1-11.
16. Akpek EK, Dart JK, Watson S, et al. A randomized trial of topical cyclosporin 0.05% in topical steroid-resistant atopic keratoconjunctivitis. Ophthalmol 2004; 111: 476-482.
17. Daniell M, Constantinou M, Vu HT, Taylor HR. Randomised controlled trial of ciclosporin A in steroid dependent allergic conjunctivitis. Br J Ophthalmol 2006; 90: 461-464.
18. Chen Y, Wang W, Yuan H, et al. Current state of monoclonal antibody therapy for allergic diseases. Research Immunol 2020; 7: 1552-1556.
19. Fukuda K, Kishimoto T, Sumi T, Yamashiro K, Ebihara N. Biologics for allergy: therapeutic potential for ocular allergic diseases and adverse effects on the eye. Allergol Int 2023; 72: 234-244.
20. Prescribing medicines in pregnancy database. Canberra: Australian Government: Therapeutic Goods Administration; 2023. Available online at: https://www.tga.gov.au/products/medicines/find-information-about-medicine/prescribing-medicines-pregnancy-database/ (accessed November 2023).