An update on lipid therapy with PCSK9 inhibitors
The PCSK9 inhibitors alirocumab and evolocumab appear to be generally safe and well-tolerated therapies, which are able to reduce elevated LDL-C by at least 50%. This is associated with a significant reduction in cardiovascular disease events in patients with prior cardiovascular disease who are already receiving standard therapy. Cost pressures may prevent more widespread use of these drugs.
In the October 2016 issue of Medicine Today,1 an unfolding era in cholesterol control through the availability of inhibitors of the enzyme proprotein convertase subtilisin-kexin type 9 (PCSK9), namely alirocumab and evolocumab, was described. New findings from landmark studies with these products have appeared over the intervening period and it is timely to revisit this subject.
Despite ‘scare-mongering’ in lay and medical media, the good efficacy and good general safety of statin therapy in reducing (but not eliminating) future cardiovascular disease (CVD) events in high-risk patients is widely accepted in Australia and internationally. But there is an important unmet need here for even more effective LDL-cholesterol (LDL-C) reduction in some patients.
PCSK9 inhibitors will not be required in those patients using a potent statin, with or without supplementary ezetimibe, where they are adequately managed in regard to current or even lower future LDL-C targets. But many high-risk patients will not reach target LDL-C and they will benefit from supplementary therapy with a PCSK9 inhibitor. This will also be applicable where there is intolerance to conventional therapy.
Who are the patients at high risk of future CVD?
Patients at high risk of future CVD are those with any of the following:
- a prior history of atherosclerotic CVD
- familial hypercholesterolaemia (generally in the more common heterozygous form, homozygosity is extremely uncommon)
- a more modest excess of LDL-C in combination with other major coronary risk factors such as diabetes, hypertension, smoking, low HDL-C or a family history of premature coronary disease.
Calculation of absolute CVD risk using widely available calculators is recommended in cases of intermediate risk, or even coronary imaging in relevant cases.
How does PCSK9 regulate LDL-C?
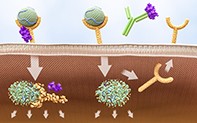
PCSK9 secreted by the liver has been shown to regulate LDL-C levels through its binding to LDL receptors, ultimately limiting their re-cycling to the cell surface, and hence reducing tissue uptake of LDL-C from the extracellular fluid. Loss-of-function mutations in the gene coding for PCSK9 have been found to be associated with low LDL-C and reduced coronary risk,2 hence the present focus on PCSK9 inhibition.
Alirocumab and evolocumab are fully humanised monoclonal antibodies to PCSK9 developed through recombinant DNA technology. These products are self-injected subcutaneously using a prefilled, fixed-dose pen usually every two weeks. A third PCSK9 inhibitor known as bococizumab has been withdrawn from use, essentially because this antibody was not fully homologous with human antibody.
Clinical trials with PCSK9 inhibitors
Early clinical trials with alirocumab and evolocumab demonstrated reductions in LDL-C of at least 50% compared with placebo injection.3 Studies were conducted in the presence or absence of statin drugs and proportionate reductions in LDL-C have been quite similar. Side effects with PCSK9 inhibitors were little different from those observed with placebo.
Yet the ultimate issue here is not just change in LDL-C but the resultant change in CVD event rates and all-cause mortality. Landmark clinical outcome trials have now been completed with these drugs.4,5 In each study all patients received standard lipid therapy (mostly statin) and other cardiovascular drugs, but half were randomised, double-blind, to receive a PCSK9 inhibitor and half to receive a placebo injection. All patients in these studies had prior CVD. In the FOURIER study with evolocumab4 this was stable CVD and in the ODYSSEY Outcomes study with alirocumab5 this was post-acute coronary syndrome. A simple comparison summarising the design features and major outcomes of the two studies is shown in the Table.
Both inhibitors reduced the composite CVD outcome by 15% (Table, Figure 1 and Figure 2). All-cause mortality was reduced significantly by 15% in the alirocumab study but was not significantly impacted in the evolocumab study. There will be continued speculation as to this apparent difference in all-cause mortality, but there are difficulties in making simple cross-study comparisons. Adverse event rates in both studies were similar between PCSK9 inhibitor and placebo, except for a small excess of injection site reactions with active treatment.
Subsequent reports from the FOURIER study show no excess of cognitive impairment in those on evolocumab;6 reductions in CVD events in the presence or absence of diabetes, with no increase in risk of new-onset diabetes nor worsening in glycaemia;7 reduction in risk of major adverse limb events in the presence or absence of prior peripheral artery disease;8 and reduction in CVD events across all strata of the inflammatory marker hs-CRP, with greatest risk reductions in patients with highest baseline hs-CRP.9 We await peer-reviewed publication of the ODYSSEY Outcomes results with similar analyses.
Given the much lower LDL-C levels achieved with PCSK9 inhibitors, many experts are suggesting that we should lower LDL-C targets as low as 1.4 mmol/L. While this might be theoretically desirable in terms of ‘the lower the better’, it is my personal view that Australian doctors might improve outcomes in more patients by being more aggressive with currently available treatment modalities in high-risk patients and being less aggressive in genuinely low-risk patients.
Who should be treated with a PCSK9 inhibitor?
As they are monoclonal antibodies that are costly to develop, produce and bring to market, there arise serious cost constraints with use of PCSK9 inhibitors. Cost-effectiveness of PCSK9 inhibitors generally remains problematic, but this is influenced by base price and the level of population risk.10 Although timing is uncertain, this is one major reason inhibitors may not be available on the PBS until 2019, except for the very rare situation of homozygous familial hypercholesterolaemia for which the current listing is complicated and contradictory. Homozygous familial hypercholesterolaemia can usually be diagnosed in the presence of the following clinical criteria: age generally below 20 to 25 years, LDL-C of more than 10 to 15 mmol/L that is poorly responsive to statins, and widespread skin and tendon xanthomas.
This is a personal, suggested approach for use of PCSK9 inhibitors on private prescription, in patients who might benefit the most. These suggestions are consistent with overseas guidelines:
- Patients who have a markedly elevated LDL-C (e.g. 5 to 6 mmol/L or more) despite taking the maximum tolerated dose of a statin (and possibly ezetimibe) – some cases of heterozygous familial hypercholesterolaemia.
- Patients at high risk of a future CVD event (e.g. those with pre-existing CVD, especially those covered above).
- Patients who are genuinely intolerant of statin drugs or ezetimibe who are also described above.
The future
PCSK9 synthesis and activity may also be reduced through administration of a chemically synthesised small interfering RNA designed to silence messenger RNA. Known as inclisiran, it is also administered by subcutaneous injection and has produced major reductions in LDL-C. It may only need to be administered at intervals of three months or longer.11 This product is currently undergoing intensive evaluation and a CVD outcomes study known as ORION-4 has commenced.
Conclusion
The administration of fully humanised monoclonal antibodies to PCSK9 appears to be a generally safe and well-tolerated therapy and this is associated with a significant reduction in CVD events in patients with prior CVD who are already receiving standard therapy. Cost-effectiveness remains problematic and cost containment may prevent more widespread use of alirocumab and evolocumab. MT