Heart failure with preserved ejection fraction – an exclusive diagnosis
Heart failure with preserved ejection fraction is common but difficult to diagnose. Echocardiography can identify structural and functional cardiac disease and may help determine an alternative cause. Exercise echocardiography can help confirm the diagnosis. GPs play an important role in facilitating early diagnosis and excluding alternative causes for symptoms.
- Exertional dyspnoea, fatigue and exercise intolerance are common presentations in general practice and causes of these symptoms include heart failure, anaemia, obesity and lung disease.
- A diagnosis of heart failure with preserved ejection fraction (HFpEF) should be considered in patients with heart failure symptoms who have preserved ejection fraction on echocardiography, accompanied by objective evidence of significant diastolic dysfunction, where elevated left ventricular filling pressures (mean left atrial pressure) drive heart failure symptoms.
- Echocardiography may identify alternative diagnoses, including previous myocardial infarction, significant valvular disease and pulmonary arterial hypertension.
- As HFpEF symptoms are classically exertional, a resting echocardiogram may not be sufficiently sensitive to fulfill diagnostic criteria when diastolic dysfunction or elevated filling pressures occur only on exertion.
- Exercise echocardiography can quantify exercise intolerance and assess cardiac function with exertion. Significant exercise-induced diastolic dysfunction may confirm the diagnosis of HFpEF or identify inducible ischaemia as an alternative cause of symptoms.
- In select patients, cardiologists may investigate further with advanced cardiac imaging and invasive right heart catheterisation, and exclude coronary artery disease with coronary angiography (invasively or using CT).
Exertional dyspnoea, fatigue and leg swelling are common presentations in primary care. These are characteristic symptoms of heart failure, including heart failure with preserved ejection fraction (HFpEF), but are also typical for many other conditions. Despite accounting for half of all incident heart failure presentations, the diagnosis of HFpEF remains one of exclusion and a challenge for clinicians.1 This article focuses on the assessment and investigation of patients presenting with signs and symptoms of heart failure who may meet criteria for the diagnosis of HFpEF.
Broadly speaking, HFpEF is a heterogeneous syndrome defined by a preserved left ventricular (LV) ejection fraction (EF; 50% or higher) and abnormalities of diastolic filling in patients with signs and symptoms of heart failure.2,3 In HFpEF, diastolic dysfunction is thought to be the predominant driver of elevated LV filling pressures. However, many comorbid conditions can mimic HFpEF and should be considered and excluded (Box 1). Specific causes of HFpEF require targeted therapies, with management of HFpEF classically centred around the prevention and control of comorbidities including diabetes and hypertension. However, unlike in heart failure with reduced ejection fraction, traditional heart failure therapies have shown limited benefit.4 Newer therapies, such as the sodium-glucose transporter 2 (SGLT-2) inhibitors, have recently been reported to improve outcomes in patients with HFpEF, although the definition of ‘preserved EF’ used to classify patients with HFpEF has varied considerably between trials.5,6
Causes of HFpEF
Principally, HFpEF is thought to be driven by LV diastolic dysfunction, where a stiff, often relatively small cavity is unable to fill without significant elevation in LV filling pressure (specifically, mean left atrial pressure). This may be detected at rest, but is often only revealed on exercise testing, when the required increase in cardiac output cannot be achieved without an elevation in mean left atrial pressure. This may result in pulmonary congestion causing dyspnoea and exercise intolerance.
Coronary artery disease, diabetes and hypertension, particularly in older patients, are the most common risk factors for HFpEF, and can cause myocardial fibrosis and scarring, resulting in reduced ventricular compliance and diastolic dysfunction. Compared with patients with reduced ejection fraction, those with HFpEF are typically older, more frequently obese and more commonly female with a higher burden of comorbidities (Box 2). Atrial fibrillation is common. The loss of co-ordinated atrial contraction, with or without associated tachycardia, is poorly tolerated in individuals with HFpEF, resulting in a higher symptom burden and greater frequency of heart failure decompensation.
In older patients with increased LV wall thickness, transthyretin (ATTR) cardiac amyloidosis should be considered as an underlying cause of HFpEF. It is probable that many of the landmark trials in HFpEF enlisted patients with ATTR amyloidosis, who are less likely to respond to heart failure therapies.7 Heart failure symptoms accompanied by bilateral carpal tunnel syndrome, biceps tendon rupture, spinal canal stenosis, new hypotension in those with a history of hypertension and intolerance to regular heart failure therapy (beta blockers and inhibitors or blockers of the renin angiotensin system) are particularly suggestive of ATTR amyloidosis. These features may be accompanied by low amplitude voltages on ECG and increased LV wall thickness on echocardiography with increased LV filling pressure.
Diagnosing HFpEF
Both Australian and European guidelines recommend a simple framework for identifying most patients with HFpEF.2,3 The following features are sufficient to identify patients with, or with high probability of, HFpEF: the presence of symptoms and/or signs of heart failure, the presence of ‘preserved’ LVEF (50% or higher) and evidence of structural (i.e. LV hypertrophy or left atrial enlargement) or functional (i.e. significant diastolic dysfunction) heart disease. Exercise limitation is a ubiquitous symptom and is considered the hallmark feature of HFpEF.
Clinical scoring systems may help identify patients with HFpEF. The H2FPEF score uses the following six variables, giving a score between 0 and 9, to estimate the probability of HFpEF:8
H2 – increased body mass index (>30 kg/m2, i.e. ‘heavy’; scored 2) and hypertension (two or more antihypertensive medicines; scored 1)
F – atrial fibrillation (paroxysmal or persistent; scored 3)
P – pulmonary hypertension (estimated pulmonary artery systolic pressure by echocardiography >35 mmHg; scored 1)
E – elderly (age >60 years; scored 1)
F – filling pressure by Doppler echocardiography (E/e’ >9; scored 1).
A score of 6 or greater indicates a high probability of an HFpEF diagnosis. A patient with an intermediate score between 2 and 5 should be referred for further specialist assessment. The HFA-PEFF algorithm is an alternative and comprehensive scoring system containing more variables; however, it has been reported to have a lower diagnostic performance than the H2FPEF score.9,10
Investigations in general practice
When HFpEF is suspected, based on heart failure signs, symptoms and risk factors, a 12-lead ECG and chest x-ray should be arranged (Flowchart). These investigations may reveal arrhythmia, increased or decreased voltages (i.e. LV hypertrophy or amyloidosis, respectively), increased cardiothoracic ratio, pulmonary congestion or other causes for symptoms. It is important to exclude or consider other contributing factors such as anaemia, obesity, lung disease, sleep apnoea, diabetes, severe renal impairment and liver disease (Box 1).
B-type natriuretic peptide (BNP) is released from the ventricles in response to volumetric distention, and elevated BNP or N-terminal proBNP (NT-proBNP) levels in the clinical setting of heart failure can be diagnostic. However, those with HFpEF often have normal or only minor elevations; therefore, a low BNP (or NT-proBNP) level does not exclude a diagnosis of HFpEF.11
Echocardiography
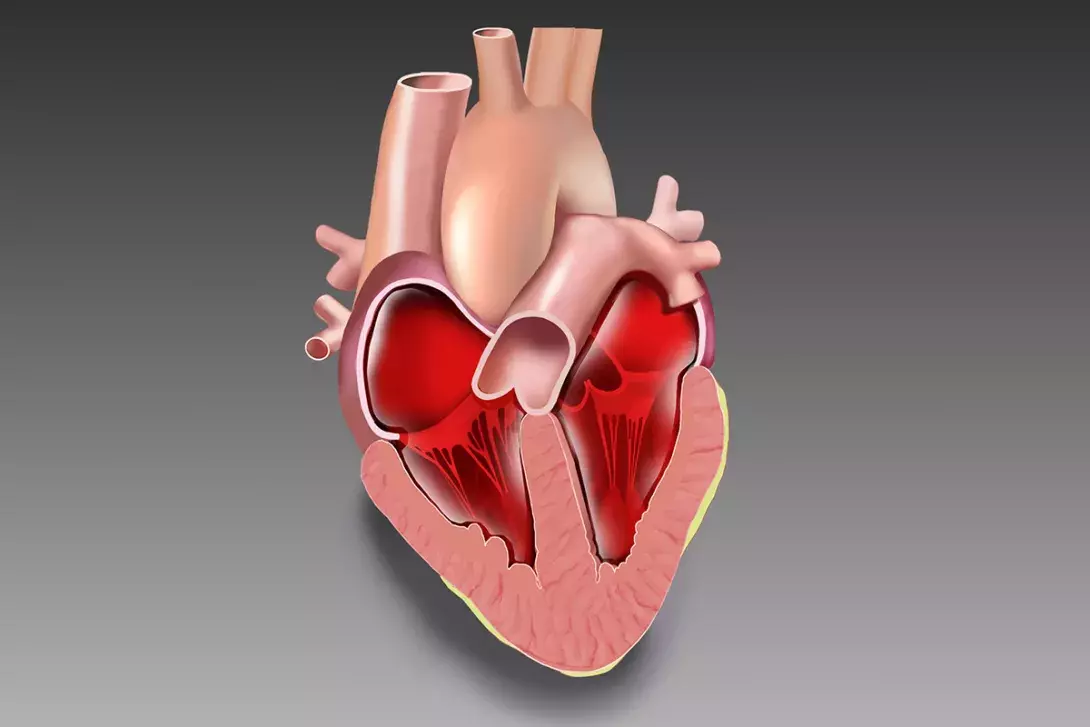
The final and most essential step of the initial workup is referral for echocardiography. Resting echocardiography provides a measurement of LVEF and, although the EF is preserved by definition, other more sensitive indices, such as tissue Doppler and strain imaging, may reveal abnormal systolic function. In this population, diastolic dysfunction is the most common contributor to elevated LV filling pressure (specifically, elevated mean left atrial pressure; Figure). Echocardiography can also provide clues to the aetiology of heart failure when myocardial infarction, significant valvular heart disease, pericardial disease and pulmonary hypertension have been excluded. Importantly, specific imaging techniques may suggest an underlying infiltrative cardiomyopathy such as cardiac amyloidosis.
Exercise echocardiography
As symptoms of HFpEF are classically exertional, resting echocardiography may not identify an elevation in LV filling pressure required for diagnosis.12-14 Echocardiography performed before and after exercise (usually on a treadmill) allows the assessment of wall motion, valvular heart disease and diastolic function.15 Exercise stress testing is preferred over pharmacological testing, as dobutamine and other agents used in stress testing do not replicate the haemodynamics of exercise.
Diastolic stress echocardiography provides formal documentation of exercise tolerance, and may help determine whether ischaemia resulting from coronary artery disease or elevation in LV filling pressure and pulmonary pressure occur during exertion.16,17 Importantly, the presence of exercise-induced diastolic dysfunction predicts outcomes, including cardiovascular death and hospitalisation, even in those with inducible ischaemia.18 However, patient selection is important, as diastolic stress echocardiography may not be appropriate for those in whom underlying comorbidities, such as obesity and lung disease (rather than abnormalities in cardiac function), are the likely cause of exercise intolerance. Owing to the specialised protocol, the diastolic stress echocardiogram is best performed in experienced centres using a semi-recumbent bicycle protocol when clinically appropriate and feasible.
As the HFpEF syndrome is a heterogeneous and comorbid condition, not all patients require referral to a cardiologist. Further cardiologist review, including exercise echocardiography or advanced cardiac imaging, may be appropriate for patients in whom heart failure is strongly suspected as the principal cause for symptoms.
Advanced investigations
The gold-standard investigation for suspected HFpEF is right heart catheterisation; however, is rarely performed in clinical practice as it is an invasive procedure. When combined with arm or leg ergometer exercise, raised pulmonary capillary wedge pressure can confirm elevated mean left atrial pressure.19 Coronary angiography, either invasively or by CT, can be undertaken if coronary artery disease is suspected. If ATTR cardiac amyloidosis is suspected on clinical grounds or based on echocardiography results, bone scintigraphy (a nuclear medicine bone scan, usually with technetium pyrophosphate) or cardiac MRI should be ordered to support the diagnosis, and serological immuno-globulin testing done to exclude a diagnosis of amyloidosis resulting from haematological malignancy.20
Conclusion
Owing to nonspecific symptoms and a wide range of contributing risk factors, diagnosing HFpEF is challenging and requires a stepwise investigative approach to rule out differential diagnoses and contributions from comorbid conditions. GPs play a vital role in identifying those at risk so that appropriate investigations can be undertaken. It is important to address the underlying factors contributing to HFpEF, most commonly hypertension, diabetes and coronary artery disease, and to exclude other potential causes of symptoms. Referral to a cardiologist should be considered when there is a high index of suspicion based on initial investigations. MT

