Postadolescent acne in women – what is the cause and how can it be managed?

Increasing numbers of women worldwide continue to have acne after adolescence or may even develop it in their 20s to 40s. These patients may have underlying hormonal abnormalities and may benefit from hormone therapy.
- Postadolescent acne in women may continue beyond the teenage years or develop at or after the age of 20 years.
- Women with postadolescent acne may have normal or raised serum androgen levels.
- Polycystic ovary syndrome may be an underlying cause of postadolescent acne in women.
- Assessment should include menstrual history taking and examination for clinical signs of hyperandrogenism, such as hirsutism.
- Hormone therapy (usually the combined oral contraceptive pill) is an effective adjunct in the management of post-adolescent acne in women, including those with normal serum androgen profiles. Other antiandrogens, such as spironolactone or cyproterone acetate, may need to be taken in addition to the oral contraceptive pill.
Acne vulgaris is a common, self-limiting disorder affecting about 9.4% of the world’s population, making it the eighth most prevalent disease globally.1 Women, including transgender and gender-diverse individuals with female reproductive organs, can have postadolescent acne that persists from the teenage years into later life, or late-onset acne that develops at or after the age of 20 years in those who have not had acne during their teens, and may even persist until menopause.2 The two presentations can also overlap and merge in many patients. It is important to recognise women with postadolescent acne as a distinct group because:
- the number of women affected worldwide is increasing3
- the psychosocial effects of acne in this group may be profound and disproportionate to the severity of acne; many women find that their acne affects their working life or professional careers (e.g. self-consciousness when having to give work presentations or meet with clients)4
- some women may have abnormal serum androgen levels that require further investigation
- these patients typically respond well to hormone therapy alone or as an adjunct to other acne therapy, even in the presence of normal laboratory investigation findings.
Acne, hormones and the sebaceous glands
Acne is a complex multifactorial disorder. Its pathogenesis involves:
- abnormal keratinisation of the pilosebaceous opening
- increased sebum production by the sebaceous glands
- colonisation of Cutibacterium acnes
- inflammation.5
Blockage of the sebaceous duct due to abnormal keratinisation produces a microscopic plug: the microcomedone. Colonisation of C. acnes in the pilosebaceous duct contributes to an inflammatory response that manifests as papules, pustules and inflammatory cysts. Effective acne management involves targeting these pathogenic steps; combination therapy is often used to target as many pathogenic factors as possible.
Sebaceous glands are found throughout the body and are present in the greatest quantity and density on the face. These glands secrete sebum in response to androgenic stimulation. In general, patients with acne produce more sebum than individuals without acne, and sebum production is greater in those with more severe acne.6
Under normal conditions, the ovaries contribute about 50% of the circulating androgens in women. Overproduction of androgens by the ovaries can occur in conditions such as polycystic ovary syndrome (PCOS) or ovarian tumours. The adrenal glands contribute the remaining 50% of circulating androgens in women. Stress may be a trigger that increases adrenal androgen production, which then stimulates increased sebum production.7,8
A detailed discussion of PCOS and other hormonal causes of acne, such as ovarian tumours and congenital adrenal hyperplasia, as well as steroid ingestion as a cause, is beyond the scope of this article.
Recognising postadolescent acne: history taking
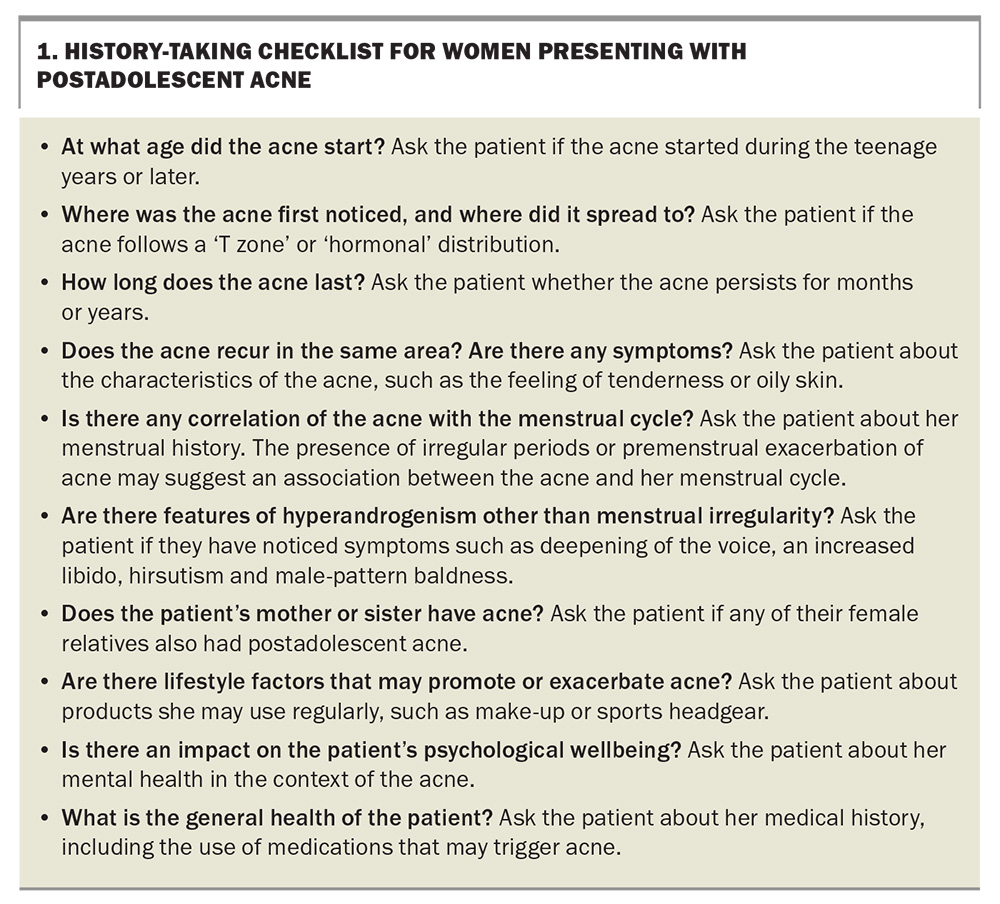
Clinical history taking of a woman presenting with postadolescent acne should include a number of factors, as discussed below and summarised in Box 1.7,9
Age of onset
Some patients develop acne with the onset of menstruation (i.e. during the teenage years), whereas some patients develop acne when they are in their 20s or older.
Distribution of acne
In some patients, the clinical pattern of postadolescent acne may look indistinguishable from teenage ‘T zone’ acne, which affects the forehead, nose and chin, with or without upper chest and upper back involvement. In other patients, there is a more ‘hormonal’ distribution, with the lower third of the face being affected, particularly the lower cheeks, jawline, chin and neck (Figure 1). The trunk may also be affected, and most patients will note seborrhoea or oily skin.
Duration of acne
Patients may complain that their current acne tends to last longer compared with acne that occurred during adolescence – for weeks, rather than days.
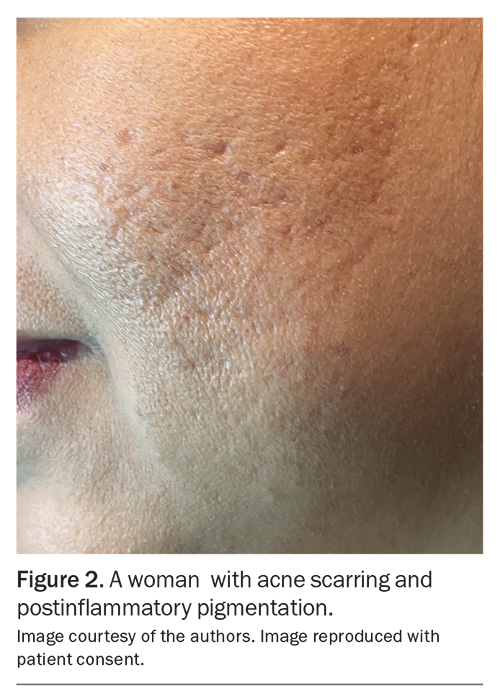
Characteristics of acne
Patients often report that their acne feels tender or ‘deep seated’. Some may describe their face as hurting. The acne may persist for weeks, heal and then recur weeks or months later in the same area. The patient may present with postinflammatory redness or pigmentation lasting for weeks or months as the acne resolves, which is often distressing for the patient. The inflammatory and chronic nature of such acne may also lead to scarring (Figure 2).
Menstrual history
It is common for acne to develop a week before menses and continue for one to two weeks. Some patients will notice acne activity at ovulation. A careful menstrual history is important in the assessment of a woman who has late-onset acne. About 60 to 70% of women may complain of worsening of their acne on a cyclical basis, usually premenstrually. An irregular menstrual cycle may suggest underlying hyperandrogenism and the presence of PCOS. It may be worthwhile for the patient to chart her menstrual cycle because patients often assume their cycle is regular. Menstrual irregularity is defined as amenorrhoea for more than three months or irregularity of the menstrual cycle of greater than seven days from a standard 28-day cycle over three consecutive cycles.
Hyperandrogenism
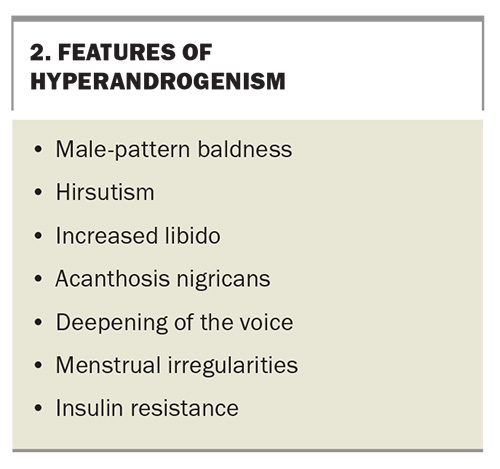
Features of hyperandrogenism other than menstrual irregularity may need specific enquiry; these features are listed in Box 2. Hirsutism may not be readily evident because patients may have undergone hair removal by a variety of means, such as waxing, electrolysis or laser treatment. Mild hirsutism and irregular menstrual cycles have been reported in up to 29% and 14%, respectively, of women with postadolescent acne.10
Obesity, hirsutism and irregular menstrual cycles are features of PCOS but are not always present in women with the syndrome.11 Data regarding the number of women with postadolescent acne who have underlying PCOS are conflicting; figures range between 10 and 50%.9,12 However, the diagnosis of PCOS can be difficult in some cases because the presentation of PCOS has marked clinical heterogeneity (including features that may have different potential causes). The presentation is also affected by individual differences (e.g. weight, ethnicity, lifestyle differences) because there are no universally accepted diagnostic criteria for PCOS.13,14
Family history
Individuals with a family history of acne tend to have an increased risk of more severe acne.8
Lifestyle factors
Many patients report flares of acne when they are feeling increased stress. Creamy or ‘greasy’ cosmetics can promote the plugging of the pilosebaceous follicle opening and are comedogenic. Some patients may work in occupations where heat may play a role, such as working in kitchens. Friction or trauma due to occlusive headgear, such as that worn for cycling, rollerblading or softball, may rupture existing comedones and cause inflammatory acne.
The use of personal protective equipment has become more important in the development of acne since the COVID-19 pandemic. Women with a prior history of acne who wore face masks continuously had significantly higher rates of experiencing ‘maskne’ compared with women without a history of acne.15
Mental health
The psychological impact of acne can be assessed using questionnaires, such as the Dermatology Life Quality Index. Stigma can be associated with adult acne, which may affect personal and professional relationships.
General medical history
Certain drugs taken for coexisting medical conditions may exacerbate acne. Some examples include phenytoin and lithium, which are prescribed for neurological diseases.16,17 Use of the 52-mg levonorgestrel-releasing intrauterine system for contraception may be associated with the development of acne, which is the most commonly reported reason for removal of the device.18
Examination of postadolescent acne
Postadolescent acne may be clinically indistinguishable from adolescent acne. The examination should focus on:
- the distribution of acne – this can include the lower cheeks, jawline, chin, neck and trunk
- the severity of acne – the acne may present as nodules, cysts and scarring
- the presence of psychological distress – this includes how the patient feels, and whether that prevents her from engaging in normal activities
- features of hyperandrogenism – these include hirsutism or androgenic alopecia, in particular.
Late-onset acne typically localises to the lower third of the face, especially the lower cheeks, jawline, chin and neck. This distribution contrasts with that of adolescent acne, which is often midfacial in distribution – in the ‘T zone’ (i.e. the forehead, nose and cheeks). Features of hyperandrogenism should be investigated (Box 2). Although there is often a typical ‘hormonal’ distribution, the pattern may be the same as that of teenage acne; thus, the two types cannot always be differentiated by the distribution of the acne.
Investigations for postadolescent acne
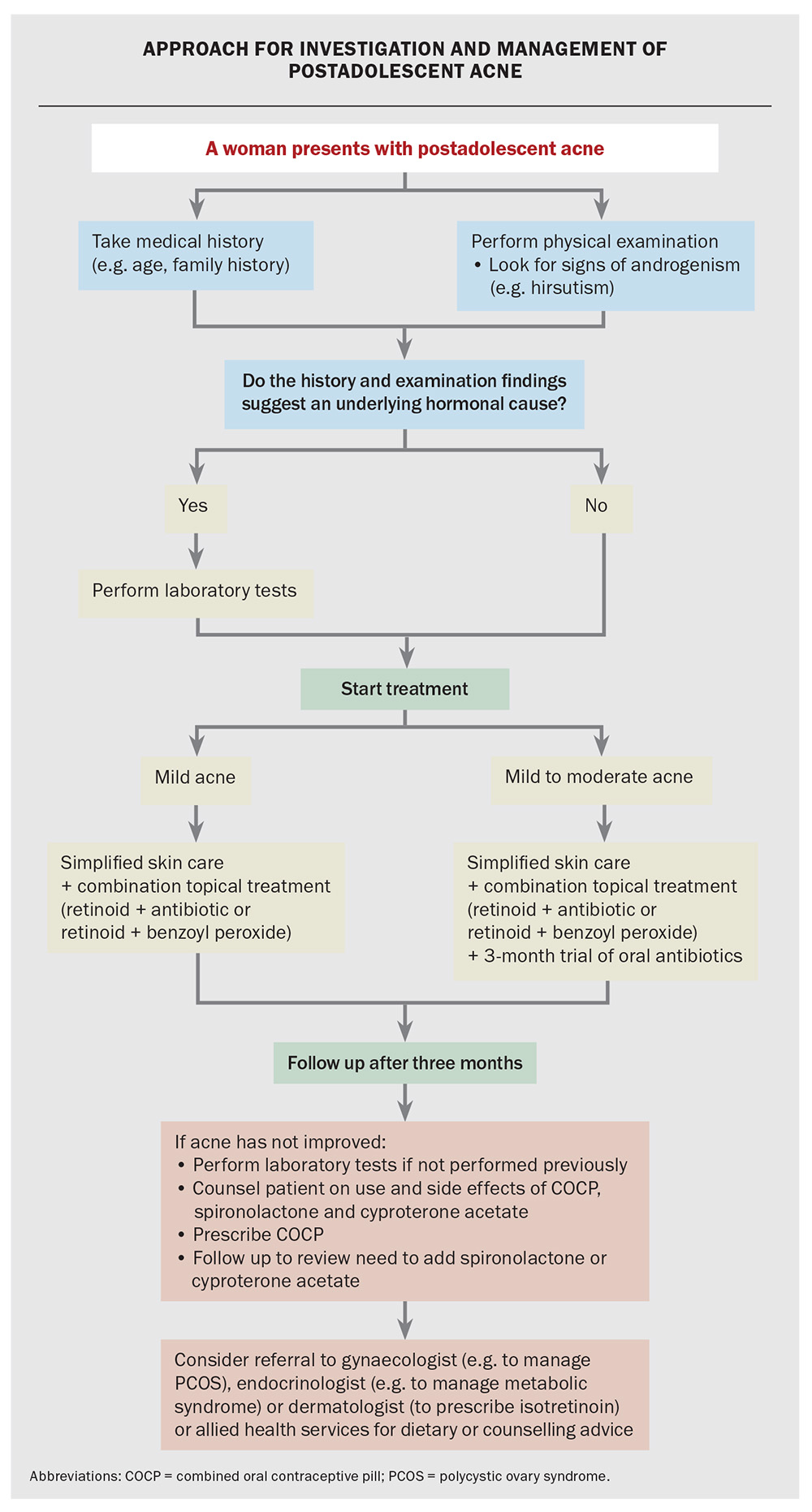
Although laboratory investigations are not indicated for most patients with acne, hormone investigations are appropriate for women with postadolescent acne, menstrual irregularities or evidence of hyperandrogenism, such as hirsutism. Hormonal contraception and spironolactone should be ceased before conducting hormone investigations.
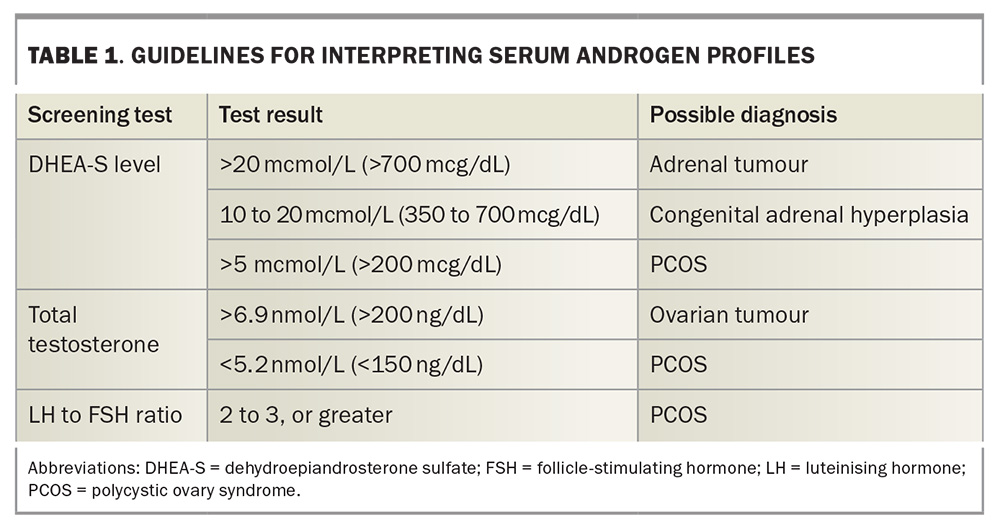
A basic screening test for androgenic abnormalities should include levels of serum free testosterone, dehydroepiandrosterone sulfate (DHEA-S) and sex hormone-binding globulin, as well as the ratio of luteinising hormone (LH) to follicle- stimulating hormone (FSH). Elevated levels of free testosterone suggest hyperandrogenism but do not indicate the origin of the elevated testosterone. Increased levels of DHEA-S suggest an adrenal cause, which may include congenital adrenal hyperplasia or, rarely, an adrenal tumour.6 Elevated levels of testosterone with an increased LH to FSH ratio (greater than 2 to 3) are consistent with a diagnosis of PCOS. The interpretation of serum androgen profiles is summarised in Table 1.
Frequently, both the ovaries and adrenals are implicated in androgen overproduction in women with late-onset acne.6 Blood samples should be obtained in the early follicular phase (days 1 to 7) of the menstrual cycle where possible, and patients taking oral contraceptives should discontinue their medication for one month before testing.
Depending on the clinical circumstances, other investigations may be indicated. These include testing levels of serum fasting glucose and lipids, prolactin, androstenedione and 17α-hydroxyprogesterone, and performing pelvic ultrasound to detect polycystic ovaries. Patients with PCOS often have insulin resistance and are at an increased risk of developing diabetes mellitus and cardiovascular disease.11 Referral to an endocrinologist or gynaecologist may be indicated. Patients may also benefit from weight reduction or a low-glycaemic-index diet; therefore, a dietitian may also provide expert advice.19
Compared with women of the same age without acne, women with postadolescent acne tend to have higher plasma levels of free androgens, often at high normal levels.6,20 It is important to appreciate, however, that the serum androgen measurements may be normal in many patients with postadolescent acne; this may reflect errors in sampling, contraceptive therapy or the end-organ response to androgens.
Sebaceous glands have a range of enzymes capable of metabolising androgens to more potent forms. For example, dihydroxytestosterone is converted to testosterone by type 1 5α-reductase in acne-prone follicles. The local androgen levels may be more significant in regulating sebum production because of metabolism or end-organ hyper-responsiveness compared with the circulating androgen levels.6,20 This is important to explain to patients because they often cannot understand why hormone treatments are prescribed in the presence of ‘normal’ hormonal assay findings.
Management of postadolescent acne
General advice and counselling
Resources on managing acne can be found on the All About Acne website (https://acne.org.au). Excessive washing and the use of antibacterial soaps and scrubs are not necessary for the cleansing of acne-affected skin; adversely, these actions may irritate the skin. Gentle cleansing using an oil-free, soap-free cleanser is appropriate, particularly for those women who have sensitive skin, whereas a foaming cleanser may be more appealing to those who have oily skin. General measures include using oil-free sunscreens, make-up products and moisturisers.
Educating and counselling patients regarding their acne is vital. Myths related to acne (e.g. ‘poor hygiene’ being a cause) should be dispelled. Patient expectations about treatments should be clarified because it may take up to three months before significant improvements are observed. Patients may need reassurance because they may have had acne for a long time or may be resistant to previously tried conventional treatments.21 Therefore, they can be frustrated by the time they present to you. Encouragement during this period is helpful to promote treatment adherence.
Women with PCOS may have abnormal lipid profiles and are at an increased risk of type 2 diabetes.11 Lifestyle modifications, including weight reduction measures and exercise, are recommended for these patients.14,19 A multidisciplinary team approach involving a dietitian, gynaecologist or endocrinologist may be required.
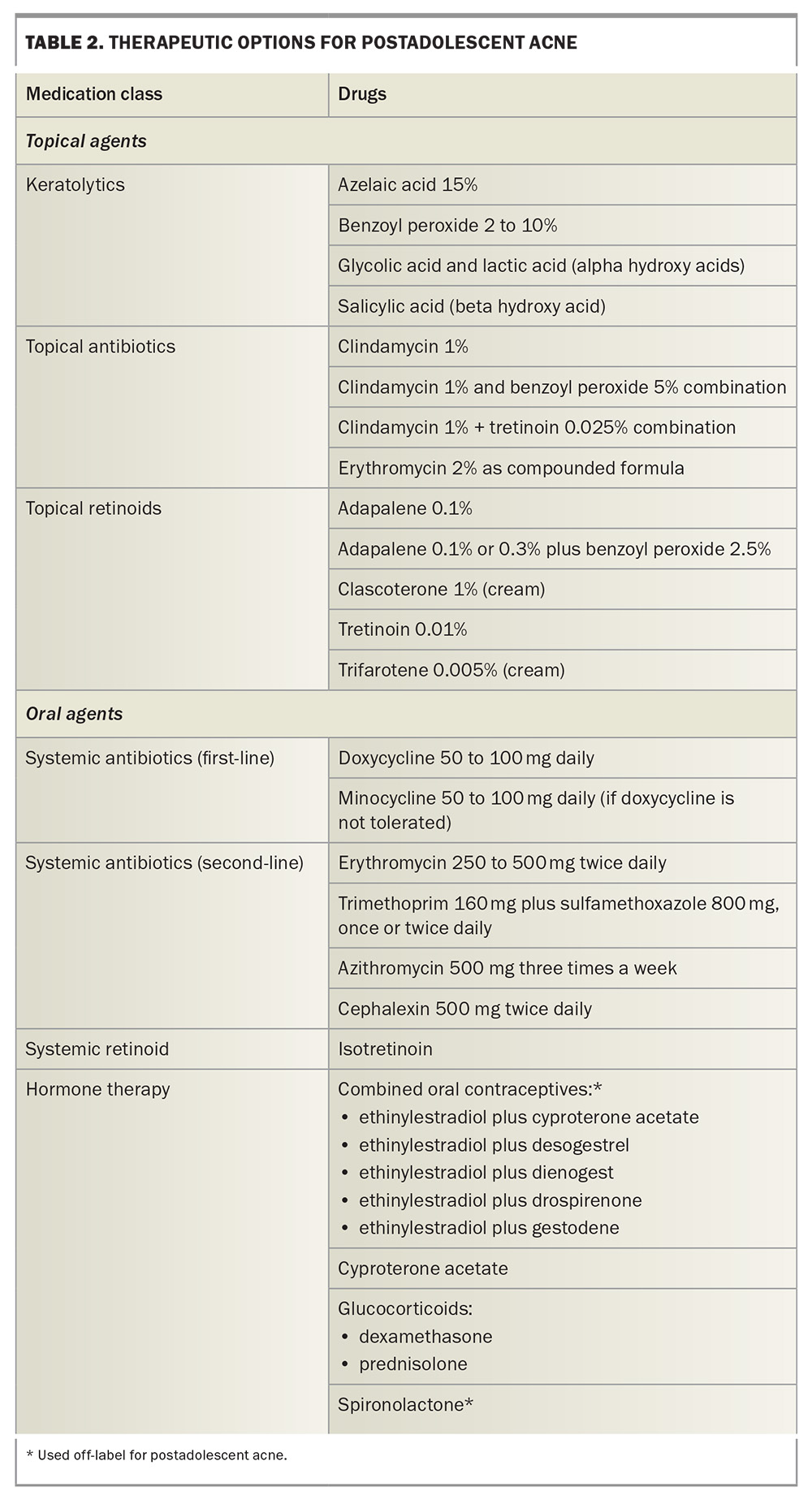
Addressing the psychological impact of acne may include referring the patient to counselling, psychology or psychiatric services.9,22 The therapeutic options for acne are summarised in Table 2. A suggested approach for the investigation and management for a patient presenting with postadolescent acne is shown in the Flowchart.
Topical agents
Topical salicylic acid, glycolic acid, azelaic acid and benzoyl peroxide are available without prescription in the form of cleansers or leave-on products. They are keratolytic and reduce comedone formation.
Cleansing, moisturising and protecting against sun exposure are important steps in caring for acne-prone skin. Skin cleansers should be non-irritating, fragrance-free, alcohol-free and noncomedogenic, and should maintain the function of the skin barrier. These may also contain anti-acne ingredients such as salicylic acid or benzoyl peroxide. Moisturisers should be alcohol-free, oil-free, noncomedogenic and fragrance-free, and should help manage the drying effects of acne treatments without promoting acne formation. Sunscreens should also be non-irritating, contain minimal ingredients, provide broad-spectrum coverage and have SPF30+ as a minimum.23
Topical antibiotic acne treatments include clindamycin 1% lotion or gel and erythromycin 2%, which can be compounded. Both these agents may be used in pregnant women, but as they may be secreted in breast milk their use should be avoided during lactation. They are particularly helpful in cases of inflammatory acne.
Topical tretinoin is the original vitamin A analogue in the retinoids class of medications, and these act mainly as keratolytic agents. Adapalene is a third-generation topical retinoid that is photostable and does not cause photosensitivity; therefore, may be applied during the daytime. A combination topical retinoid treatment containing adapalene 0.1% plus benzoyl peroxide 2.5% is available; it should be applied once daily. A stronger preparation containing adapalene 0.03% plus benzoyl peroxide 2.5% is also available. The newest fourth-generation retinoid, trifarotene, is available as a 0.005% cream. Ideally, these retinoids should be applied at night, and patients should be advised about their side effects, which include irritation and photosensitivity. These agents should be avoided in pregnancy.
Clascoterone 1% cream is a novel androgen receptor inhibitor that has recently been approved by the TGA for acne. This blocks the stimulation of oil glands in the skin by androgens. It does not cause increased skin sensitivity and is nonirritating. It should be applied twice a day.24
Combination topical and oral therapy is often required in patients with postadolescent acne.
Systemic antibiotics
Oral antibiotic therapy is effective for inflammatory acne and suppresses acne until spontaneous clearing occurs.
Doxycycline 50 to 100 mg daily and minocycline 50 to 100 mg daily are usually used as the first-line antibiotics. Erythromycin 250 to 500 mg twice daily (or erythromycin ethyl succinate 400 to 800 mg twice daily) and trimethoprim 160 mg plus sulfamethoxazole 800 mg once or twice daily are second-line antibiotic choices. Other options include cephalexin 500 mg twice daily or azithromycin 500 mg three times a week. The choice of antibiotic choice is influenced by drug interactions.
Ideally, oral antibiotics should only be used for a maximum of three months at a time to minimise potential antibiotic resistance. If longer courses are required, then the antibiotic should be used in combination with topical benzoyl peroxide, as this reduces the risk of developing antibiotic resistance.21,25 Alternatively, a break of one to two weeks may be taken between three-month oral antibiotic courses during which benzoyl peroxide is used. Therefore, systemic antibiotics are not an ideal option for long-term therapy, which is often needed for hormonal acne.
Oral isotretinoin
Women who have nodulocystic or scarring acne should be referred to a dermatologist for treatment with oral isotretinoin. Oral isotretinoin reduces comedogenesis, reduces sebum secretion and is anti-inflammatory.26
Patients should be given counselling with respect to contraception and the risk of birth defects while taking systemic retinoid medication. Pretreatment investigations include a serum lipid level test, a serum pregnancy test and liver function tests; liver function tests should be conducted regularly during therapy.
Although patients with hormonal acne respond well to isotretinoin, they may relapse when their treatment courses are complete because of the underlying hormonal stimulation of the oil glands. Although low-dose or even intermittent oral isotretinoin will help control acne in some patients, oral isotretinoin should be considered a treatment option for refractory cases. If acne tends to recur quickly after a course of isotretinoin has been completed, then antiandrogen hormone therapy, such as the oral contraceptive, should be considered as maintenance treatment.
Hormone therapy
Hormone therapy, usually with the oral contraceptive pill, is very effective in women who have postadolescent acne with or without elevated serum androgen levels.27 Hormone therapy reduces sebum production by decreasing androgenic stimulation of the sebaceous glands. It may be used in combination with other anti-acne therapies.
Hormone therapy for postadolescent acne in women is indicated:
- in those with ovarian, adrenal or peripheral hyperandrogenism
- in those with PCOS
- for moderate to severe acne unresponsive to other therapies
- if relapse occurs after multiple courses of antibiotics
- if relapse occurs quickly after a course of isotretinoin as an alternative to repeated courses of isotretinoin.
The therapeutic effect of hormone therapy is slow, and patients should be warned not to expect noticeable improvement for three months. Therapy should be continued for at least 12 months. Relapses are common when hormone therapy is ceased.
Combined oral contraceptives
The oestrogenic component of the combined oral contraceptive pill suppresses ovarian production of androgens and stimulates the production of sex hormone-binding globulin, thus reducing free testosterone levels. This is beneficial and hence oral contraceptives are prescribed off-label for acne because the oil glands are exposed to a reduced androgenic stimulus.28
Although all combined oral contraceptives are effective for acne because of the oestrogenic component, those containing androgenic progestins, such as norgestrel and levonorgestrel, are theoretically less effective. Preparations containing low-androgenic progestogens, such as desogestrel or gestodene, are considered helpful anti-acne contraceptives, as they impart fewer androgenic effects, such as oily skin that can promote acne.29 For many years, the ‘gold standard’ has been the combination of ethinylestradiol 35 mcg plus cyproterone acetate 2 mg. Alternatives include the combinations ethinylestradiol 30 mcg plus dienogest 2 mg, ethinylestradiol 30 mcg plus drospirenone 3 mg and ethinylestradiol 20 mcg plus drospirenone 3 mg.
Side effects of hormone therapy include nausea, breast tenderness, weight gain and headache. There may also be an increased risk of breast cancer and this should be discussed with the patient, along with other relative contraindications.30 Mention should also be made of the several long-term benefits of oral contraceptive therapy, which include reduced risks of ovarian and uterine cancers.31
Appropriate patient selection and counselling are required with the use of the oral contraceptive pill. Although this article focusses on postadolescent acne, hormone therapy is also appropriate for female adolescents with acne; however, oral contraceptive therapy should be avoided before puberty because of the risk of accelerated epiphyseal closure.
The efficacy of oral contraceptives for acne is attributed largely to the oestrogenic component. Progestogen-only pills and implants are therefore unsuitable as anti-acne therapies, and some patients using these have noted a worsening of their acne. Patients should be warned that acne improvement may be slow (taking at least three months) and that treatment is long term (at least one year). Combination treatment may yield improved efficacy; if the acne has not improved significantly after three to six months of oral contraceptive therapy, then an androgen receptor antagonist, such as cyproterone acetate or spironolactone, can be added.
Cyproterone acetate
Cyproterone acetate is an antiandrogenic progestogen that acts by both inhibiting ovulation and blocking the androgen receptor. The combination of cyproterone acetate 2 mg plus ethinylestradiol 35 mcg is very effective for the treatment of acne in women with mild to moderate hyperandrogenism.32
Cyproterone acetate is also available as a single agent in 10 mg and 50 mg tablets and can be prescribed in addition to a combined oral contraceptive preparation containing it, or any other combined oral contraceptive. The dose of cyproterone acetate can therefore be increased if the acne is unresponsive to an ethinylestradiol plus cyproterone acetate oral contraceptive. For example, 50 mg of cyproterone acetate may be added to the first 10 days of a cycle of an ethinylestradiol 35 mcg plus cyproterone acetate 2 mg combined oral contraceptive (or another combined oral contraceptive), starting with the first active pill. Alternatively, 10 mg of cyproterone acetate can be added to the first 15 days of the pill cycle. In postmenopausal women or in those who have undergone hysterectomy, 50 mg of cyproterone acetate may be added to the entire active cycle (21 days) of therapy with an ethinylestradiol plus cyproterone acetate-containing oral contraceptive.
Improvement can be seen in 75 to 90% of women with acne who are treated with cyproterone acetate 50 to 100 mg per day.33 Oestrogen is necessary in these regimens because cyproterone acetate has strong antioestrogenic effects. Side effects of cyproterone acetate therapy include menstrual abnormalities, breast tenderness and enlargement, mood changes, headache, nausea, melasma and fluid retention.
Glucocorticoids
If a woman’s hyperandrogenism is caused by an adrenal disorder, low-dose prednisolone (2.5 mg daily) or dexamethasone (0.25 mg daily) can be used to suppress the adrenal production of androgens. Long-term use of these agents poses a risk of adrenal cortisol suppression, and patients should be monitored for this with periodic adrenocorticotropic hormone stimulation tests. Ideally, these patients should be co-managed with an endocrinologist.
Spironolactone
Spironolactone is useful for women who are intolerant to oestrogens, have a contraindication to oestrogen therapy or do not wish to use oral contraceptives. Spironolactone acts as a competitive androgen receptor antagonist and as an inhibitor of 5α-reductase and is effective in doses of 50 to 200 mg daily. Using it off-label as monotherapy at low doses of 25 to 50 mg may improve acne and not alter the menstrual cycle. If higher daily doses are required, these are often combined with the oral contraceptive pill so that the menstrual cycle is kept regular. Treatment may be prolonged (six months or more), but dosages may be reduced once an adequate clinical response is achieved.
Dose-dependent side effects of spironolactone therapy include menstrual irregularities, breast tenderness, hyperkalaemia, headache, dizziness, drowsiness and hypotension. Side effects may be minimised if therapy is started with a low dose of 25 to 50 mg daily. As an antiandrogen, spironolactone may cause feminisation of a male fetus and, therefore, patients should not become pregnant while taking the medication. Although the monitoring of blood pressure and serum electrolytes may be required in some patients, most young and healthy patients show no abnormalities in their blood pressure and do not require laboratory tests.
Other treatments
This article does not address physical therapy modalities that may be helpful in managing postadolescent acne, such as chemical peels and laser therapy. A potentially promising modality is the new 1726 nm laser, which selectively targets sebaceous glands.34
Conclusion
Women with postadolescent acne are a relatively common presentation in general practice. Assessment of such patients should include identifying the presence of hyperandrogenism and possible underlying causes. Hormone therapy, such as the combined oral contraceptive pill, is an effective treatment and may be combined with other acne therapies such as topical agents and oral antibiotics. MT
COMPETING INTERESTS: Dr See has received consulting fees from Viatris, L’Oreal, Galderma, SunPharma and CSL; has received payment from Viatris, L’Oreal, Galderma, SunPharma and CSL; is co-chair of the All About Acne group; and is a member of the Public Affairs committee of the Australasian College of Dermatology. Dr Byrom has received payment from Oraderm; has been a board member for SunPharma; is a member of the All About Acne group; and is a member of the Australasian College of Dermatologists.
References
1. Tan JKL, Bhate K. A global perspective on the epidemiology of acne. Br J Dermatol 2015; 172: 3-12.
2. Dreno B, Layton A, Zouboulis CC, et al. Adult female acne: a new paradigm. J Eur Acad Dermatol Venereol 2013; 27: 1063-1070.
3. Chang J, Nock MR, Cohen JM, et al. Acne accounts for an almost 2.5-fold higher proportion of dermatology visits among adult females compared to adult males in the United States: a study of the national ambulatory medical care survey from 2002-2016. PLoS One 2023; 18: e0290763.
4. Gisondi P, Puig L, Richard MA, et al. Quality of life and stigmatization in people with skin diseases in Europe: a large survey from the ‘burden of skin diseases’ EADV project. J Eur Acad Dermatol Venereol 2023; 37: 6-14.
5. Dréno B. What is new in the pathophysiology of acne, an overview. J Eur Acad Dermatol Venereol 2017; 31: 8-12.
6. Del Rosso JQ, Kircik L. The cutaneous effects of androgens and androgen-mediated sebum production and their pathophysiologic and therapeutic importance in acne vulgaris. J Dermatolog Treat 2024; 35; 2298878.
7. Bagatin E, de Freitas THP, Machado MCR, Ribeiro BM, Nunes S, da Rocha MAD. Adult female acne: a guide to clinical practice. An Bras Dermatol 2019; 94: 62-75.
8. Heng AHS, Chew FT. Systematic review of the epidemiology of acne vulgaris. Sci Rep 2020; 10: 5754.
9. Kutlu O, Karadağ AS, Wollina U. Adult acne versus adolescent acne: a narrative review with a focus on epidemiology to treatment. An Bras Dermatol 2023; 98: 75-83.
10. Goulden V, Clark SM, Cunliffe WJ. Postadolescent acne: a review of clinical features. Br J Dermatol 1997; 136: 66-70.
11. Goodman NF, Cobin RH, Futterweit W, Glueck JS, Legro RS, Carmina E; American Association of Clinical Endocrinologists (AACE); American College of Endocrinology (ACE); Androgen Excess and PCOS Society (AES). American Association of Clinical Endocrinologists, American College of Endocrinology, and Androgen Excess and PCOS Society disease state clinical review: guide to the best practices in the evaluation and treatment of polycystic ovary syndrome - part 1. Endocr Pract 2015; 21: 1291-1300.
12. Kim GK, Michaels BD. Postadolescent acne in women: more common and more clinical considerations. J Drugs Dermatol 2012; 11: 708-713.
13. Teede H, Tay CT, Laven J, et al. International evidence-based guideline for the assessment and management of polycystic ovary syndrome 2023. Melbourne: Monash University; 2023. Available online at: https://www.monash.edu/medicine/mchri/pcos/guideline (accessed March 2024).
14. Teede HJ, Tay CT, Laven JJE, et al.; International PCOS Network. Recommendations from the 2023 international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Eur J Endocrinol 2023; 189: G43-G64.
15. Masood S, Ghulam U, Rahmatullah Z, et al. MASKNE - prevalence and association of causative factors during Covid-19 pandemic at a tertiary care hospital of Karachi. J Pak Med Assoc 2023; 73: 1221-1225.
16. Asadi-Pooya AA, Rostaminejad M, Zeraatpisheh Z, Damabi NM. Cosmetic adverse effects of antiseizure medications; a systematic review. Seizure 2021; 91: 9-21.
17. Kazandjieva J, Tsankov N. Drug induced acne. Clin Dermatol 2017; 35: 156-162.
18. Oliveira ECF, Baeta T, Cotta RCF, et al. Use of 52-mg levonorgestrel-releasing intrauterine system in adolescents and young adult women: 3-year follow-up. J Pediatr Adolesc Gynecol 2023; 36: 45-50.
19. Shahid R, Ul Haq I, Mahnoor, et al. Diet and lifestyle modifications for effective management of polycystic ovarian syndrome (PCOS). J Food Biochem 2022; 46: e14117.
20. Ju Q, Tao T, Hu T, Karadağ AS, Al-Khuzaei S, Chen WC. Sex hormones and acne. J Clin Dermatol 2017; 35: 130-137.
21. Walsh TR, Efthimiou J, Dréno B. Systematic review of antibiotic resistance in acne: an increasing topical and oral threat. Lancet Infect Dis 2016; 16: e23-e33.
22.Rocha MA, Bagatin E. Adult-onset acne: prevalence, impact, and management challenges. Clin Cosmet Investig Dermatol 2018; 11: 59-69.
23. Goh CL, Wu Y, Welsh B, et al. Expert consensus on holistic skin care routine: Focus on acne, rosacea, atopic dermatitis, and sensitive skin syndrome. J Cosmet Dermatol 2023; 22: 45-54.
24. Peterson H, Kircik L, Armstrong AW. Individual article: clascoterone cream 1%: mechanism of action, efficacy, and safety of a novel, first-in-class topical antiandrogen therapy for acne. J Drugs Dermatol 2023; 22: SF350992s7-SF350992s14.
25. Baldwin H, Elewski B, Hougier F, et al. Sixty years of benzoyl peroxide use in dermatology. J Drugs Dermatol 2023; 22: 54-59.
26. Sadeghzadeh-Bazargan A, Ghassemi M, Goodarzi A, Roohaninasab M, Nobari NN, Behrangi E. Systematic review of low-dose isotretinoin for treatment of acne vulgaris: Focus on indication, dosage, regimen, efficacy, safety, satisfaction, and follow up, based on clinical studies. Dermatol Ther 2021; 34: e14438.
27. Elsaie ML. Hormonal treatment of acne vulgaris: an update. Clin Cosmet Investig Dermatol 2016; 9: 241-248.
28. Schindler AE. Antiandrogenic progestins for treatment of signs of androgenisation and hormonal contraception. Eur J Obstet Gynecol Reprod Biol 2004; 112: 136-141.
29. Stewart M, Black K. Choosing a combined oral contraceptive pill. Aust Prescr 2015; 38: 6-11.
30. Mørch LS, Skovlund CW, Hannaford PC, Iversen L, Fielding S, Lidegaard Ø. Contemporary hormonal contraception and the risk of breast cancer. N Engl J Med 2017; 377: 2228-2239.
31. Loizzi V, Cerbone M, Arezzo F, et al. Contraception as chemoprevention of ovarian cancer in BRCA1 and BRCA2 women. Hormones (Athens) 2023; e-pub (https://doi.org/10.1007/s42000-023-00519-6).
32. Beylot C, Doutre MS, Beylot-Barry M. Oral contraceptives and cyproterone acetate in female acne treatment. Dermatology 1998; 196: 148-152.
33. Van Wayjen RG, van den Ende A. Experience in the long-term treatment of patients with hirsutism and/or acne with cyproterone acetate-containing preparations: efficacy, metabolic and endocrine effects. Exp Clin Endocrinol Diabetes 1995; 103: 241-251.
34. Scopelliti MG, Hamidi-Sakr A, Möller S, Karavitis M, Kothare A. Selective photothermolysis in acne treatment: the impact of laser power. J Cosmet Dermatol 2024; 23: 457-463.