Advanced respiratory disease: managing symptoms in the last years of life

Symptoms in advanced respiratory disease are varied and commonly include breathlessness, fatigue and cough. Symptom control can be complex and difficult to navigate, particularly in the last few years of life as the disease progresses and patients’ needs escalate. Management is best optimised through holistic multidisciplinary approaches, with management of individual symptoms alongside treatment of the underlying disease process.
- Symptoms in advanced respiratory disease are varied, complex and require specific attention to improve patient experiences.
- Key symptoms include the cluster of chronic breathlessness, fatigue and cough, as well as depression and anxiety, insomnia, cachexia, pain and dry mouth.
- Clinical care is best optimised through a holistic, multidisciplinary approach, with individual symptoms targeted through additional management strategies when symptoms persist despite maximising treatment of the underlying disease(s).
- Nonpharmacological interventions for breathlessness are effective and are the main approach to manage chronic breathlessness. These include mobility aids, activity pacing, breathing techniques and the use of a handheld fan to move airflow on the face.
- The psychological impact of advanced respiratory disease is often overlooked and needs to be directly addressed in best practice care.
- Early introduction of advance care planning (ACP) offers patients the opportunity to document their care preferences and address evident lack of support for chronic lung disease in the final stages of disease. The conversation around ACP should be ongoing as patients’ preferences evolve throughout disease progression.
Management of advanced respiratory disease has increasingly shifted to primary care and community settings, owing to a growing focus on supported, home-based care and preferences to avoid hospital presentation. Symptoms in advanced respiratory disease are varied, and can be complex to manage, particularly in the last years of life as the disease progresses and patients’ needs escalate.1 The symptoms discussed in this article are most common in chronic obstructive pulmonary disease (COPD) but are also relevant to other chronic conditions such as pulmonary fibrosis, bronchiectasis and lung cancer. Breathlessness in particular is also highly prevalent in advanced cancers and heart failure.2
Defining the last years of life in advanced respiratory disease
Despite well-recognised fluctuation in chronic respiratory conditions (often with periods of exacerbation), indicative prognostic characteristics have been established. In particular, the question ‘Would I be surprised if this patient did not survive the next 12 months?’ is a useful clinical prompt.3,4 This question has been found to have high specificity and is a simple prompt for clinicians to actively focus on symptom control, in combination with ongoing disease-directed management of the underlying condition.3,4
The nature and intensity of symptoms also signal a patient’s changing needs. A modified Medical Research Council (mMRC) breathlessness scale score of 3 (‘breathless after walking a few minutes or 100 metres on the flat’) or 4 (‘too breathless to leave the house or breathless when dressing or undressing’) indicates severe breathlessness.5,6
Hospitalisation with an acute exacerbation of COPD has long been recognised as a prognostic indicator of advanced respiratory disease.6,7 Mortality risk varies across studies; however, a 2017 retrospective study reported one- and five-year mortality of patients hospitalised for COPD as 26.2% and 64.3%, respectively, with mechanical ventilation further increasing these risks.7 Acute hospitalisation is therefore recommended as an opportunity to discuss and plan for future care.7,8 Low body mass index (less than 21.75 kg/m2) and cachexia are also reliable prognostic indicators in advanced respiratory disease.9,10
Although the ability of prognostic indicators to predict death varies considerably across patients, its utility lies in the opportunity to prompt an additional care focus – notably the treatment of symptoms as a specific treatment goal.
Management of key symptoms
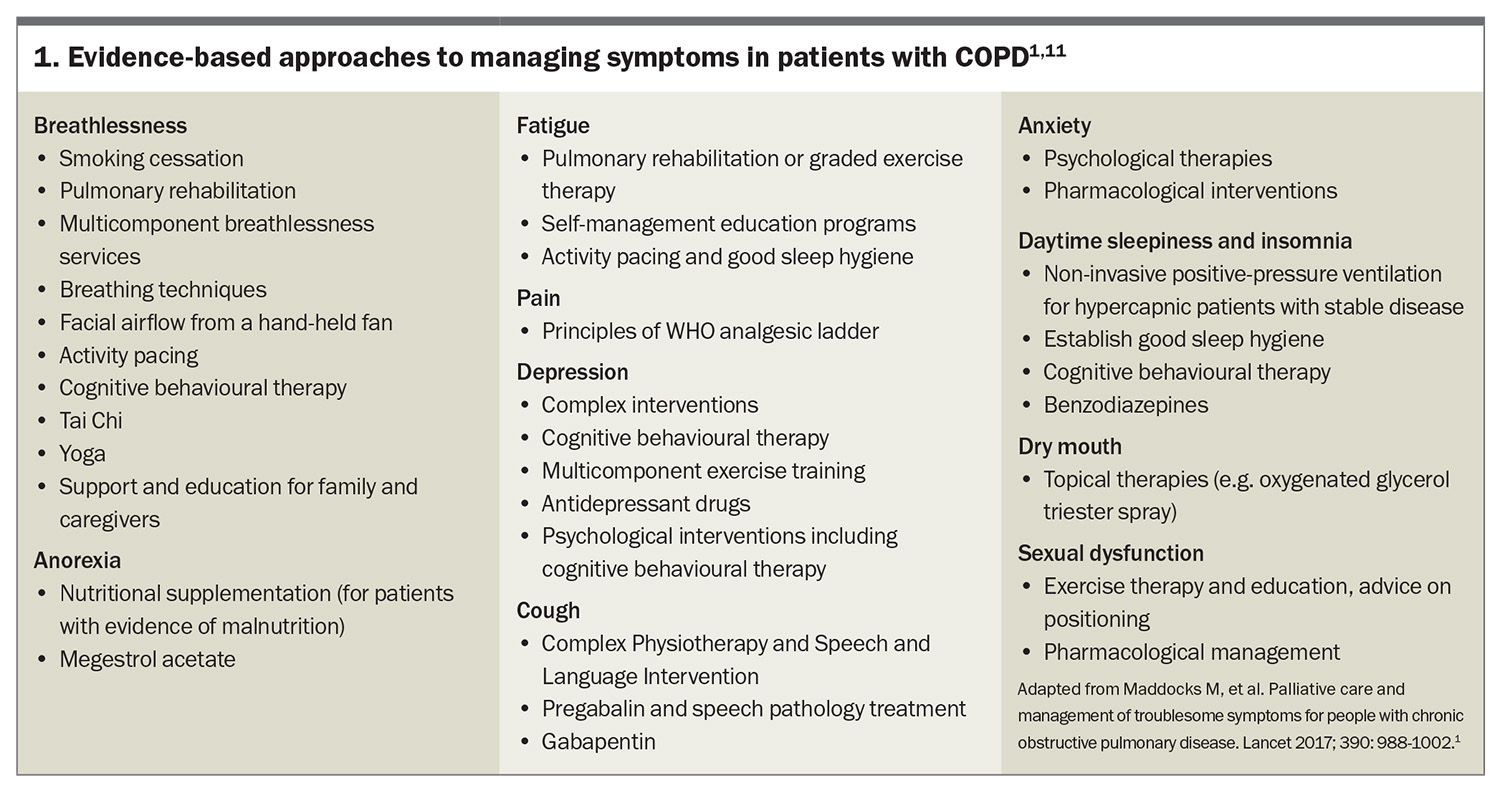
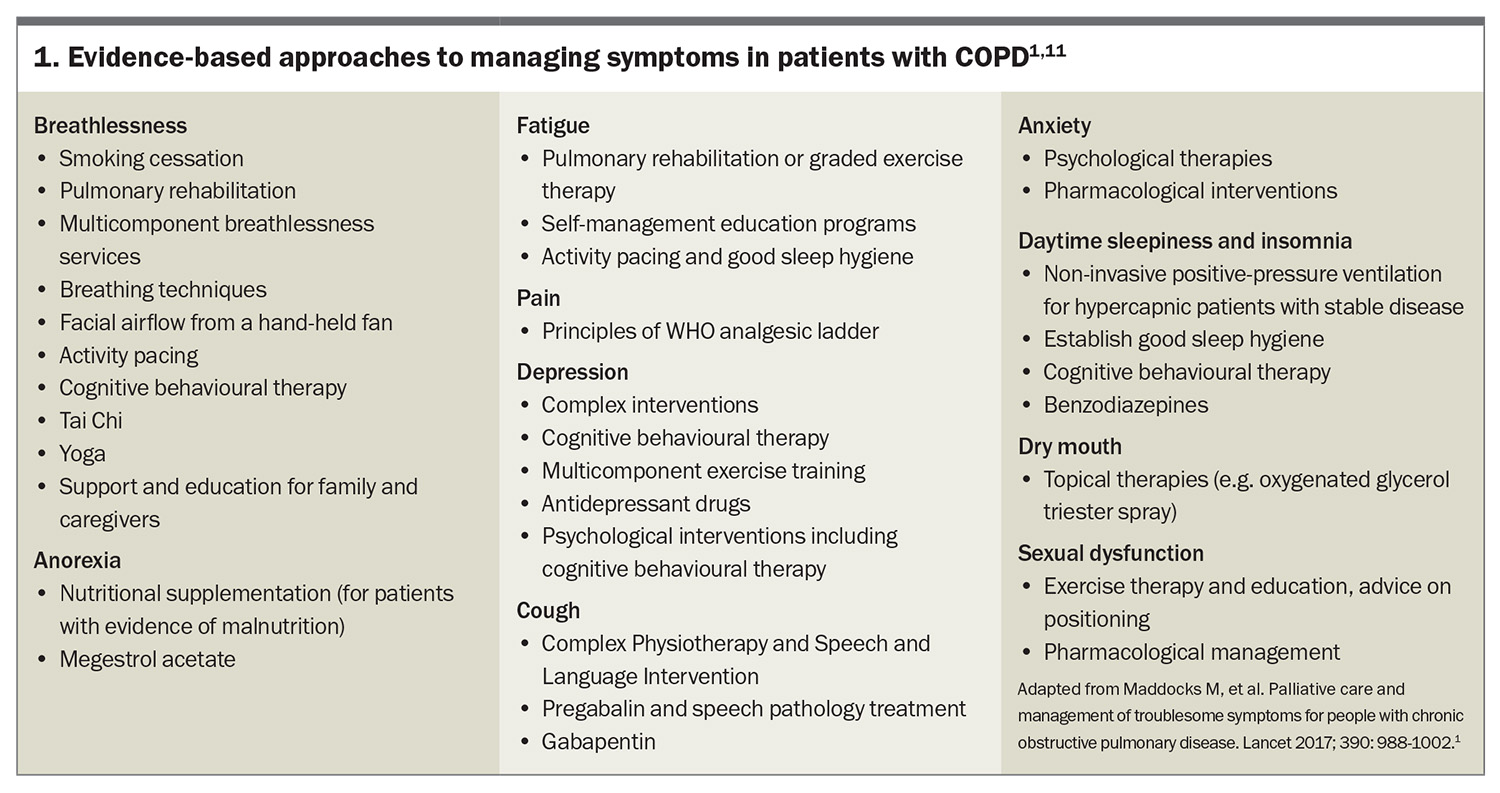
Symptoms in advanced respiratory disease vary; however, key symptoms may occur as a ‘respiratory cluster’, including chronic breathlessness, fatigue and cough. Other important symptoms include depression, anxiety, insomnia, cachexia, pain and dry mouth.1 Comprehensive, individualised assessment of the underlying illness, symptoms and the needs of the patient and their carers is essential. This needs assessment usually occurs iteratively over time.11 Although a broad and holistic approach to symptom management is recommended, individual symptoms should be addressed if they persist despite optimal management of the underlying disease.1 A useful summary of evidence-based approaches to individual symptom management of COPD is presented in Box 1.1,11
Breathlessness
Chronic breathlessness is extremely distressing for patients with chronic respiratory disease, and highly prevalent in people with severe COPD. Both GPs and specialists often voice a lack of confidence in its management.12,13 Breathlessness is multidimensional and defined as ‘an unpleasant subjective experience of discomfort with breathing that worsens as underlying disease processes increase in severity; in its chronic and severe state, breathlessness can lead to significant disability, progressive inactivity, social isolation and substantive suffering’.14 In addition, ‘chronic breathlessness’ is defined as breathlessness that ‘persists despite optimal treatment of the underlying pathophysiology and that results in disability’.15,16 A comprehensive approach to the evaluation and treatment of breathlessness is helpful and includes addressing reversible contributing causes, including anaemia, pleural effusion or anxiety; and implementation of evidence-based nonpharmacological interventions.11
Nonpharmacological interventions
Nonpharmacological interventions for breathlessness are effective and accessible; therefore, they should be offered to all patients with chronic breathlessness.1,11 For example, activity pacing, mobility aids and adjusting a patient’s living environment can assist in conserving energy for valued activities.1,11 Increased physical activity and personalised exercise programs (such as pulmonary rehabilitation) can improve stamina and breathlessness.11 Breathing exercises, such as pursed lip breathing, slow relaxed deep breathing and yoga breathing have been shown to be safe and to improve breathlessness for some people with advanced lung disease.17,18 Hand-held motorised fans (Figure and videos) are similarly low harm, low cost, easy interventions that directly target and reduce the sensation of breathlessness.1,11,19 Breathing retraining, accessed through specialist physiotherapy services, can also help improve associated dysfunctional breathing patterns.
Anxiety associated with breathlessness can lead to avoidance of those physical activities that address deconditioning.1 Psychological and counselling therapies, including cognitive behavioural therapy (CBT), discussed below, can address negative thought processes and reluctance to engage in helpful activities.1,20 Similarly, education and supported self-management can help patients improve self-efficacy, which in turn can reduce anxiety and depression, increase activity and social contact, and boost quality of life.1
Opioids
The 2024 European Respiratory Society Clinical Practice Guideline on symptom management for people with serious respiratory illness recommended against the use of opioids to treat chronic breathlessness.11 This recommendation is based on the findings from a systematic review undertaken for the Guideline.21 This systematic review identified that although clinical trials administering one to two doses of opioids in an exercise laboratory-setting led to improved exertional breathlessness during standardised exercise testing, when opioids were administered regularly at home over several days or weeks, there was no beneficial impact on breathlessness experienced in daily life.21 Importantly, adverse effects (nausea, constipation and drowsiness) were significantly increased amongst people receiving opioids, and serious adverse events (including hospitalisation and death) occurred in approximately one-third of people receiving opioids in one clinical trial.21 Additionally, many patients express concerns regarding taking opioids for chronic breathlessness because of concerns regarding medication safety, impacts on the ability to drive, dependence, addiction, stigma and the associations with substance misuse and death or dying.21
Importantly, the data for this recent systematic review were predominantly drawn from clinical trials undertaken in people with COPD.21 As such, there is little evidence regarding the use of opioids to treat chronic breathlessness in people with other advanced, nonmalignant, respiratory illnesses.21 Opioids may therefore be considered on an individual basis in people at the end of life or with other non-malignant respiratory illnesses with severe persisting breathlessness (despite optimisation of disease-directed treatment and nonpharmacological interventions for symptom management).21 When opioids are prescribed to treat chronic breathlessness, clinicians must weigh up the potential harms versus benefits, ensure the treatment aligns with the patient’s values and goals, and carefully discuss this treatment as part of shared decision-making.21
Other pharmaceutical approaches
Benzodiazepines are not recommended to treat breathlessness, except as second- or third-line therapy, or at the very end of life.22 A recent multisite, randomised, double-blind, placebo-controlled, clinical trial evaluating the effectiveness of mirtazapine on chronic breathlessness in people with severe breathlessness (mMRC score of 3-4) and COPD or interstitial lung disease (ILD), failed to demonstrate any benefits.23 However, the trial was substantially underpowered because of difficulties with recruitment during the pandemic. It should be noted that there were more adverse effects in the people receiving mirtazapine (64%) compared with people taking placebo (40%); therefore, the authors recommended against the use of mirtazapine to treat severe breathlessness.23 Further efficacy trials for anxiolytics are needed; however, in the interim, all patients receiving such agents should be monitored for benefit and adverse effects when treated with these or other symptom relief measures.2,22
Fatigue
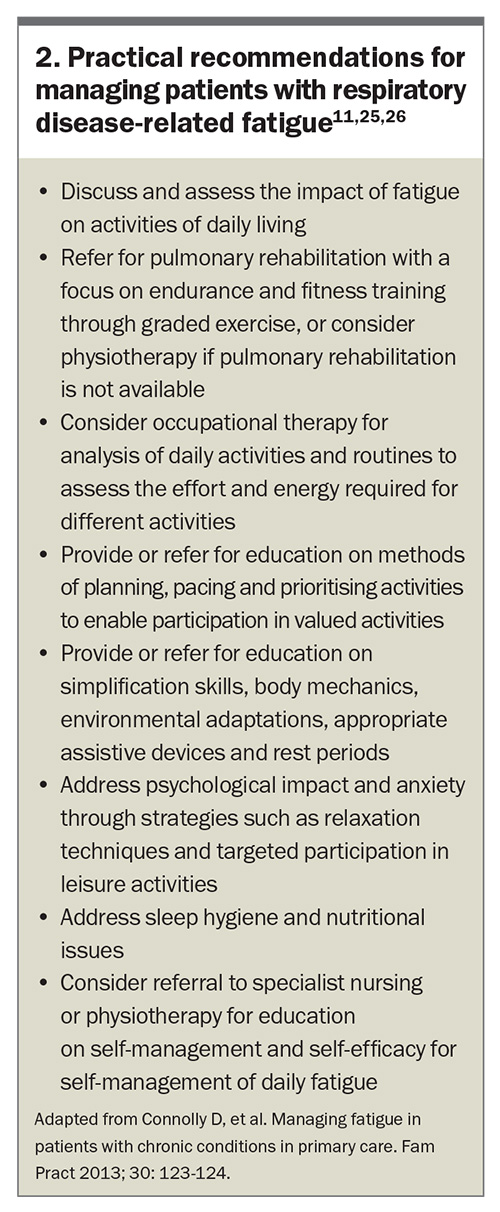
Fatigue is defined as ‘a profound feeling of physical and psychological weariness that is not relieved by sleep or rest’.1 Similar to breathlessness, fatigue is complex and requires a multicomponent approach to management, including physical conditioning (individualised pulmonary and graded exercise programs), psychological support, supported self-management and resilience training.11,24 Additionally, treatment for comorbid depression is crucial, as this may compound the experience of fatigue.1,25
The recent European Respiratory Society Clinical Practice Guideline on symptom management for adults with serious respiratory illness emphasised the role of physical activity as the primary approach for managing fatigue in people with chronic respiratory conditions. The Guideline recommends graded exercise, which involves ‘establishing a baseline of achievable exercise or physical activity and then making fixed incremental increases in the time spent being physically active’.
Occupational therapy-driven management, with a focus on daily life adjustment and maximising participation, has shown promise. Such evidence-based interventions aim to increase patients’ understanding of fatigue, identify exacerbating factors and facilitate development of fatigue management strategies (Box 2).11,25,26
Cough
Chronic cough related to underlying maximally-treated respiratory disease is a significant source of distress for patients.1 Primary management approaches include physiotherapy, speech and language therapies (such as sputum-clearance techniques, cough control and cough-reflex hypersensitivity training), and psychoeducational counselling (Box 1).1
Pharmacological treatments are not well evidenced. However, a recent systematic review and meta-analysis of the neuromodulator gabapentin reported significant improvement in cough-specific quality of life, cough severity and frequency in chronic refractory cough.27 Antitussive P2X purinoceptor 3 (P2X3) antagonists, which target airway vagal afferent nerve hypersensitisation, may also provide a pathway to mediate cough reflex. Although P2X3 antagonists are not yet available in Australia, preclinical and preliminary trial data are promising and P2X3 antagonists may be the new dawn in addressing this distressing symptom.28
Psychological impact
One often overlooked area within advanced respiratory disease is the psychological impact on patients, particularly in light of sustained symptoms.29,30 The association between chronic respiratory disease and depression and anxiety is well documented, as is social and existential isolation. Psychological issues are reported in as many as 60% of people with COPD.20,31,32
Despite disease and symptom management optimisation, for many, a significant burden remains. Raising issues around psychological coping and patient experience provides patients the opportunity and permission to voice the full impact of their condition.
Key treatments for depression and anxiety include behavioural therapies and CBT, as well as pharmacological interventions (Box 1). Multicomponent exercise training has also shown positive impact for patients with advanced respiratory disease and depression.1 Psychological therapy and counselling are acknowledged as useful, particularly in patients with chronic disease. CBT is a well-established treatment for anxiety and depression that seeks to increase a patient’s understanding of their current difficulties and help manage unhelpful thoughts, and has shown promising outcomes for patients with COPD.20 Of importance, several studies, including a recent large randomised controlled trial, showed that respiratory nurses trained in, and delivering CBT, improved anxiety and healthcare utilisation (emergency department presentations and hospitalisation) among patients with chronic respiratory disease.29,33 Peer and facilitated support groups have similarly shown improvement in the wellbeing of patients with chronic respiratory conditions.29 Empowerment through shared experience and collegial support may also improve active engagement with healthcare.29
Connecting patients with support and social services is increasingly important.34 ‘Social prescribing’, in which primary care services actively link patients to support services within the community and volunteer sectors, can help improve health and wellbeing.35 Social prescribing activities, including community gardening, group learning, volunteer work and music- and arts-based activities, are of particular value to patients with chronic conditions, such as advanced respiratory disease, in whom disease-related social isolation plays a key role in psychological dysfunction.
Other symptoms
Other symptoms associated with chronic respiratory disease include anorexia, dry mouth and insomnia. Evidence for the management of these symptoms is varied. Anorexia management relies primarily on nutritional supplementation, patient education and dietetic support. For patients with dry mouth, it can be helpful to review inhaler therapies that may contribute to this symptom and consider changing the device or the medication. Additionally, local topical therapies (such as oral lubricants of saliva substitutes) can be helpful.36 Insomnia and daytime sleepiness is treated with sleep hygiene and CBT, and benzodiazepines may be prescribed for short-term intervention.1 Comorbidities may also contribute to symptoms, thus the approach to management should always be to maximise the treatment of all contributing underlying conditions.
The importance of advance care planning
Despite the life-limiting nature of chronic respiratory diseases, few patients have plans in place for the later stages of disease and care, and less than 18% of patients with COPD in Australia access palliative care in the last 12 months of life.37-40
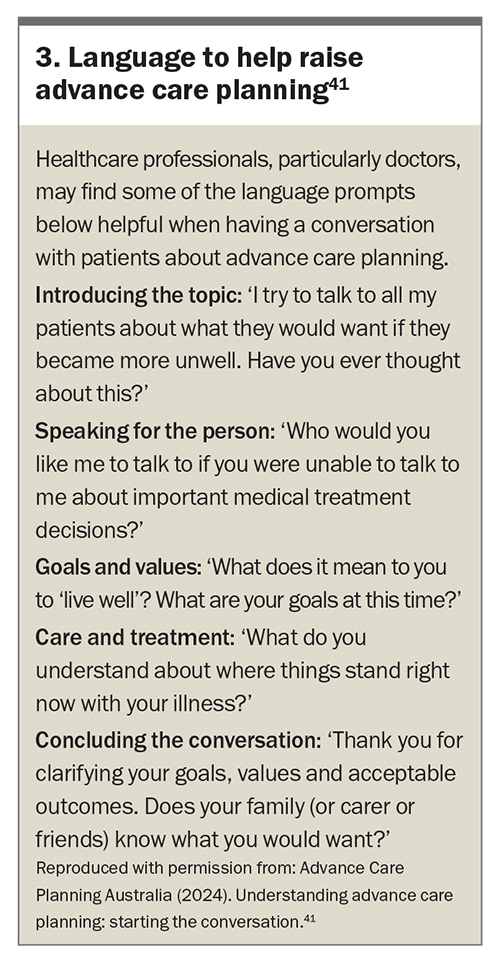
Advance care planning (ACP) is a process and opportunity in which patients ‘think about, discuss and record preferences for the type of care they wish to receive and the outcomes they would consider acceptable’.41 The process involves a series of conversations engaging patients and their family in exploring values, burdens and preferences, and allows healthcare professionals, the patient and their family to develop a shared understanding of how to best provide care that addresses and reflects the person’s expressed goals.41
ACP increases palliative care involvement, and reduces the likelihood of clinically futile treatments and decision-making in a period of crisis. For patients with COPD, ACP can provide a heightened sense of control, and reduce anxiety and depression.42,43
Providing multiple and early opportunities to discuss long-term care wishes and priorities with patients is recommended.41 These conversations are likely to evolve, as the patient’s perspectives may change over time, emphasising the importance of ongoing conversations and willingness for continued discussion of healthcare preferences, even after an advance directive is in place.41 Advance Care Planning Australia provides information on ACP, and includes language to help raise the conversation (Box 3) and videos for health professionals.41
Efficient conversations for long-term care
Patient-driven and patient-led consultations are sometimes erroneously considered too time consuming within the constraints of busy clinical practice.44 Instead, evidence indicates that interactions commenced with a simple question as to the patient’s priorities result in more time-efficient consultations and care that is more strongly aligned with patient’s current and ongoing needs.45 This becomes increasingly important when addressing care within the final years of life. Creating opportunities for patients to voice their priorities for care and ensuring the opportunity is taken to start a longer discussion over several consultations that plans care for now and the future, rather than attempting to address all issues raised, is essential.44,45
When to start a palliative approach in COPD
The recent European Respiratory Society Clinical Practice Guideline: Palliative care for people with COPD or ILD recommends that a palliative care approach should be considered ‘when people with COPD or ILD and their informal caregivers have physical, psychological, social or spiritual/existential unmet needs’. And that ‘needs should be assessed using report from the person with illness, or their informal caregiver report, but surrogate markers of disease severity and/or health service utilisation may help identify those likely to have unmet needs.’ 46
Healthcare professionals often hesitate to consider a palliative approach ‘due to the uncertain disease trajectory, lack of a clear transition to "end of life", normalisation of living with COPD, and lack of professional awareness of the potential role of palliative care’. However, early engagement with palliative care is recommended and has been shown to improve survival and quality of death in patients with COPD.46,47
Involvement of specialist palliative care teams may be of benefit for patients experiencing unresolved symptoms and challenging situations.6 Reasons for referral may include: management of persisting refractory symptoms; psychosocial, spiritual or existential care; co-ordination of care; active management of the terminal phase (at home or in a hospice); and emotional care and bereavement support of relatives and carers.47 Patient and caregiver reluctance and misunderstanding of palliative care (as specific to cancer and the final days of life), compounds referral challenges; however, once referred, acceptability is high.46
Conclusion
Management of respiratory symptoms is best optimised through holistic approaches that address individual symptoms in addition to the underlying disease. Symptom burden commonly escalates in the last years of life as the disease progresses. Identifying patients within this category is crucial for well-managed and planned care. Key prognostic indicators for chronic disease include the question ‘would I be surprised if this patient did not survive the next 12 months?’. Similarly, discussing patients’ priorities for care and early engagement with ACP can better facilitate care that addresses their ongoing needs. RMT
COMPETING INTERESTS: None.
References
1. Maddocks M, Lovell N, Booth S, Man WD, Higginson I. Palliative care and management of troublesome symptoms for people with chronic obstructive pulmonary disease. Lancet 2017; 390: 988-1002.
2. Wiseman R, Rowett D, Allcroft P, Abernethy A, Currow D. Chronic refractory dyspnoea: evidence based management. Aust Fam Physician 2013; 42: 137-140.
3. Noppe D, Veen In’t, Mooren KJ. COPD patients in need of palliative care: Identification after hospitalization through the surprise question. Chron Respir Dis 2019; 16: 1479972318796219.
4. Tripp D, Janis J, Jarrett B, et al. How well does the surprise question predict 1-year mortality for patients admitted with COPD? J Gen Intern Med 2021; 36: 2656-2662.
5. Bestall J, Paul E, Garrod R, Garnham R, Jones P, Wedzicha J. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax 1999; 54: 581-586.
6. Philip j, Chang YK, Collins A. Consensus palliative care referral criteria for people with chronic obstructive pulmonary disease. Thorax 2024; 79: 1006-1016.
7. García-Sanz M-T, Cánive-Gómez J-C, Senín-Rial L, et al. One-year and long-term mortality in patients hospitalized for chronic obstructive pulmonary disease. J Thorac Dis 2017; 9: 636-645.
8. Suissa S, Dell’Aniello S, Ernst P. Long-term natural history of chronic obstructive pulmonary disease: severe exacerbations and mortality. Thorax 2012; 67: 957-963.
9. Kwan HY, Maddocks M, Nolan CM, et al. The prognostic significance of weight loss in chronic obstructive pulmonary disease‐related cachexia: a prospective cohort study. J Cachexia Sarcopenia Muscle 2019; 10: 1330-1338.
10. Guo Y, Zhang T, Wang Z, et al. Body mass index and mortality in chronic obstructive pulmonary disease: a dose–response meta-analysis. Medicine (Baltimore) 2016; 95: e4225.
11. Holland AE, Spathis A, Marsaa K, et al. European Respiratory Society Clinical Practice Guideline on symptom management for adults with serious respiratory illness. Eur Respir J 2024; 63: 2400335.
12. Smallwood N, Currow D, Booth S, Spathis A, Irving L, Philip J. Differing approaches to managing the chronic breathlessness syndrome in advanced COPD: a multi-national survey of specialists. COPD 2018; 15: 294-302.
13. Politis J, Eastman P, Le B, Furler J, Irving L, Smallwood N. Managing severe chronic breathlessness in chronic obstructive pulmonary disease is challenging for general practitioners. Am J Hosp Palliat Care 2021; 38: 472-479.
14. Mularski RA. Advancing a common understanding and approach to dyspnea management. Consensus proposal for the chronic breathlessness syndrome. American Thoracic Society; 2017; 14: 1108-1110.
15. Johnson MJ, Yorke J, Hansen-Flaschen J, et al. Towards an expert consensus to delineate a clinical syndrome of chronic breathlessness. Eur Respir J 2017; 49: 1602277.
16. Kochovska S, Ekström M, Hansen-Flaschen J, et al. Hiding in plain sight: the evolving definition of chronic breathlessness and new ICD-11 wording. Eur Respir J 2023; 61: 2300252.
17. Donescky-Cuenco D, Nguyen HQ, Paul S, Carrieri-Kohlman V. Yoga therapy decreases dyspnoea-related distress and improves functional performance in people with chronic obstructive pulmonary disease: a pilot study. J Altern Complement Med 2010; 15: 225-234.
18. Burge AT, Gadowski AM, Jones A, et al. Breathing techniques to reduce symptoms in people with serious respiratory illness: a systematic review. Eur Respir Rev 2024; 33: 240012.
19. Bausewein A, Holland L, Romero A, et al. Airflow for the reduction of breathlessness in people with serious respiratory illness: a systematic review. Eur Respir Rev 2024 [in press, not yet published].
20. Heslop-Marshall K, Burns G. The role of cognitive behavioural therapy in living well with COPD. Breathe 2019; 5: 95-97.
21. Smallwood NE, Pascoe A, Wijsenbeek M, et al. Opioids for the palliation of symptoms in people with serious respiratory illness: a systematic review and meta-analysis. Eur Respir Rev 2024; 33: 230265.
22. Verberkt CA, van den Beuken-van Everdingen MHJ, Schols JM, Datla S, Dirksen CD, Johnson MJ, et al. Respiratory adverse effects of opioids for breathlessness: a systematic review and meta-analysis. Eur Respir J 2017; 50: 1701153.
23. Higginson IJ, Brown ST, Oluyase AO, et al. Mirtazepine to alleviate severe breathlessness in patients with COPD or interstitial lung diseases (BETTER-B): an international, multicentre, double-blind, randomised, placebo-controlled, phase 3 mixed-method trial. Lancet 2024: 12; 763-774.
24. Burge AT, Gadowski AM, Romero L, et al. The effect of graded exercise therapy on fatigue in people with serious respiratory illness: a systematic review. Eur Respir Rev 2024; 33: 240027.
25. Kahlmann V, Moor CC, Wijsenbeek MS. Managing fatigue in patients with interstitial lung disease. Chest 2020; 158: 2026-2033.
26. Connolly D, O’Toole L, Redmond P, Smith SM. Managing fatigue in patients with chronic conditions in primary care. Fam Pract 2013; 30: 123-124.
27. Xie S, Xie M, Shen Y, Cheng D. Gabapentin for chronic refractory cough: a systematic review and meta-analysis. Heliyon 2023; 9: e15579.
28. Abdulqawi R, Dockry R, Holt K, et al. P2X3 receptor antagonist (AF-219) in refractory chronic cough: a randomised, double-blind, placebo-controlled phase 2 study. Lancet 2015; 385: 1198-1205.
29. Hunter R, Barson E, Willis K, Smallwood N. Mental health illness in chronic respiratory disease is associated with worse respiratory health and low engagement with non-pharmacological psychological interventions. Intern Med J 2021; 51: 414-418.
30. Wang J, Willis K, Barson E, Smallwood N. The complexity of mental health care for people with COPD: a qualitative study of clinicians’ perspectives. NPJ Prim Care Respir Med 2021; 31: 40.
31. Bolton LE, Seymour J, Gardiner C. Existential suffering in the day-to-day lives of those living with palliative care needs arising from chronic obstructive pulmonary disease. BMJ & Supportive Palliative Care; 2020; 10 (Suppl1): A66-A67. [Poster presentation] Abstract available online at: https://spcare.bmj.com/content/10/Suppl_1/A66.3 (accessed March 2025).
32. Disler RT, Green A, Luckett T, et al. Experience of advanced chronic obstructive pulmonary disease: metasynthesis of qualitative research. J Pain Symptom Manage 2014; 48: 1182-1199.
33. Heslop-Marshall K, Baker C, Carrick-Sen D, et al. Randomised controlled trial of cognitive behavioural therapy in COPD. ERJ Open Res 2018; 4: doi: 10.1183/23120541.00094-2018.
34. Wildman JM, Moffatt S, Steer M, Laing K, Penn L, O’Brien NJ. Service-users’ perspectives of link worker social prescribing: a qualitative follow-up study. BMC Public Health 2019; 19: 98.
35. Pescheny JV, Randhawa G, Pappas Y. The impact of social prescribing services on service users: a systematic review of the evidence. Eur J Public Health 2020; 30: 664-673.
36. Frydrych A. Dry mouth: xerostomia and salivary gland hypofunction. Aust Fam Physician 2016; 45: 488-492.
37. Rosenwax L, Spilsbury K, McNamara BA, Semmens J. A retrospective population based cohort study of access to specialist palliative care in the last year of life: who is still missing out a decade on? BMC Palliat Care 2016; 15: 46.
38. Smallwood N, Thompson M, Warrender-Sparkes M, et al. Integrated respiratory and palliative care may improve outcomes in advanced lung disease. ERJ Open Res 2018; 4: doi: 10.1183/23120541.00102-2017.
39. Australian Institute of Health and Welfare (AIHW). Palliative care services in Australia. AIHW; 2024. Available online at: https://www.aihw.gov.au/reports/palliative-care-services/palliative-care-services-in-australia/contents/palliative-care-workforce (accessed March 2025).
40. Smallwood N, Ross L, Taverner J, et al. A palliative approach is adopted for many patients dying in hospital with chronic obstructive pulmonary disease. COPD 2018; 15: 503-511.
41. Advance Care Planning Australia. Understanding advance care planning. Advance Care Planning Australia 2024. Available online at: https://www.advancecareplanning.org.au/understand-advance-care-planning/starting-the-conversation (accessed March 2025).
42. Ke LS, Huang X, O’Connor M, Lee S. Nurses’ views regarding implementing advance care planning for older people: a systematic review and synthesis of qualitative studies. J Clin Nurs 2015; 24: 2057-2073.
43. Janssen DJ, Engelberg RA, Wouters EF, Curtis JR. Advance care planning for patients with COPD: past, present and future. Patient Educ Couns 2011; 86: 19-24.
44. Warnecke E. The art of communication. Aust Fam Physician 2014; 43: 156-158.
45. Stewart M, Brown JB, Weston W, McWhinney IR, McWilliam CL, Freeman T. Patient-centered medicine: transforming the clinical method. 3rd edn. London: Taylor & Francis; 2013.
46. Janssen DJA, Bajway S, Hilton Boon M, et al. European Respiratory Society clinical practice guideline: palliative care for people with COPD or interstitial lung disease. Eur Respir J 2023; 62: 2202014.
47. COPD-X Plan Guidelines. Palliative and supportive care. COPD-X Plan Guidelines 2024. Available online at: https://copdx.org.au/copd-x-plan/o-optimise-function/o10-palliation-and-end-of-life-issues/ (accessed March 2025).