RSV infection in an infant

A 5-month-old boy presents in general practice with two days of fever, cough and runny nose. What are the important steps in management of this child?
- Respiratory syncytial virus (RSV) infection is a common presentation in general practice, and can result in severe morbidity and rarely death in infants and children.
- Long-term sequelae of early severe RSV infection include increased risk of recurrent wheeze, asthma, lower respiratory tract infection and impaired lung function. This can persist through to adulthood.
- Prevention of RSV is paramount. Vaccinations should be offered to pregnant women and monoclonal antibodies should be offered to infants.
Case scenario
Harry, a 5-month-old boy, presents in general practice with two days of fever, a cough and runny nose. His older brother attends daycare, and has been unwell with the same symptoms for the past week. Harry was born at 30 weeks’ gestation, but does not have any other comorbidities, is fully immunised, growing well and developing normally.
You note that Harry is pink in room air and has mild increased work of breathing when unsettled and tachypnoea with intercostal and subcostal recession. He has good air entry bilaterally, with transmitted upper airway sounds. He is breastfeeding more than half his usual volume with good wet nappies.
You diagnose Harry with a viral upper respiratory tract infection but are satisfied there are no red flags that indicate Harry is significantly unwell. You perform a nasopharyngeal viral swab. You also provide advice to the parents for supportive care and plan to review him in two days.
Harry returns for review two days later, and is noted to have moderate to severe work of breathing with bilateral crackles and wheeze. His interest in feeding is markedly reduced and he struggles to latch on to the breast consistently. His nappies have been dry for the past 12 hours. The swab results detected respiratory syncytial virus (RSV) and you diagnose Harry with bronchiolitis.
What are the next steps in management? Should Harry be referred to the local emergency department?
Commentary
Respiratory tract infections, including those caused by RSV, are a leading cause of hospitalisations and presentations to GPs. When reviewing infants and young children with respiratory symptoms, it is important to consider the severity of disease, risk of deterioration and hydration status to determine the level of additional support that they may require.
Key aspects of assessment of the sick child in the GP setting
To assess for red flags in children with respiratory tract infections in a GP setting, it is important to consider the following.
- Does the child have increased work of breathing? Classify this as mild, moderate or severe.
- Is the child hypoxaemic (oxygen saturation lower than 93%)?
- Is the child adequately hydrated? Assess their fluid intake and urine output.
- Is the child at risk of deterioration? Consider risk factors, such as preterm infants, underlying respiratory conditions and previous intensive care unit admissions.
- Has the fever been present for more than five days? Consider secondary bacterial infections.
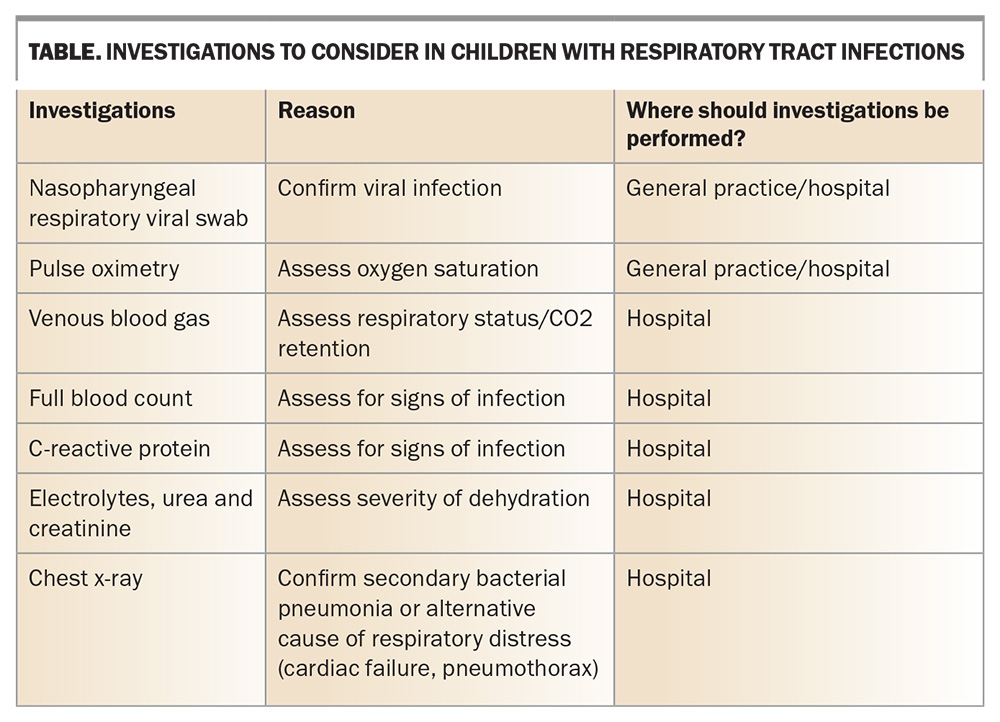
If the child is assessed as having mild illness, with no red flags, the GP may perform a nasopharyngeal viral swab, explain the natural history of RSV infections and provide advice regarding supportive care. However, it is important to provide a safety net for follow up and signs to monitor for, such as deterioration in feeding, dehydration or worsening work of breathing (e.g. chest wall recession, tracheal tug and tachypnoea), which may become evident as the infant becomes increasingly unwell. Further investigations to consider in children with respiratory tract infections are listed in the Table.
Management
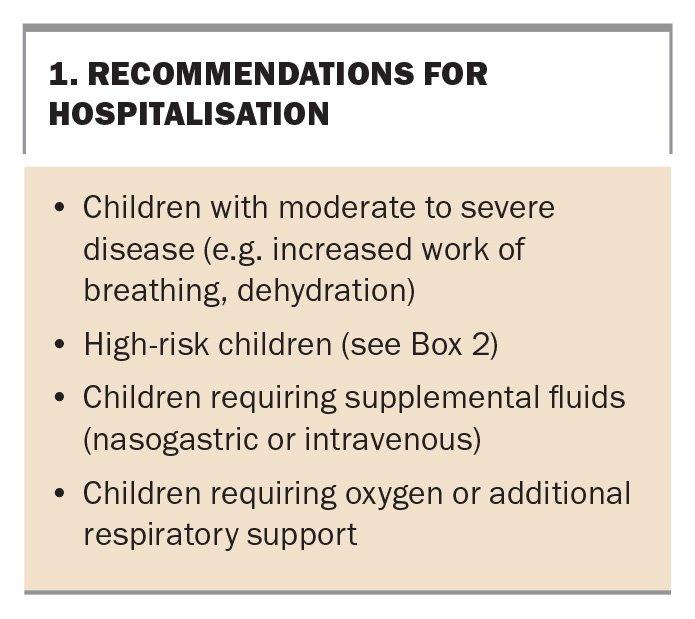
Management of RSV infection in children is largely focused on supportive care. This includes nasal suction to relieve congestion, antipyretics, hydration and oxygen for children with hypoxia.1 Recommendations on when to refer a child to the local emergency department are outlined in Box 1.
Dehydration should be managed in a stepwise manner, starting with smaller frequent feeds. If the child is not tolerating this, or there are still signs of dehydration, continuous nasogastric feeds should be commenced. Finally, if the child is still dehydrated, intravenous fluid therapy may be required. Children with more severe disease resulting in respiratory compromise or failure may also require additional respiratory supports, such as high-flow nasal cannula and noninvasive or invasive ventilation. These children should also be assessed for complications, such as secondary bacterial pneumonia, and treated accordingly.
Disease burden in Australia
Children are disproportionately affected by RSV infection compared with adults. Those aged less than 5 years account for the majority of RSV-associated hospitalisations, with the highest rates of admission occurring in children under 6 months of age (2224 per 100,000 population).2 Furthermore, the hospitalisation rate of those born at less than 28 weeks’ gestation is almost eight times higher than their term counterparts.3 The median length of stay for children less than 5 years of age admitted to Australian hospitals with RSV infections is three days.2 Although death is rare, children under 5 years of age account for 15% of all RSV-related hospital deaths.2
Long-term complications
Although most children recover from RSV infection without complications, there is evidence that severe RSV infection early in life increases the risk of recurrent wheeze, asthma, recurrent lower respiratory tract infections and impaired lung function.4 These effects can persist into adulthood.4 A recently published long-term study found that people with early lower respiratory tract infections were almost twice as likely to die prematurely of respiratory disease, irrespective of lifestyle factors.5 Although the long-term effects are not fully understood, potential mechanisms include altered epithelial cell barrier, changes to the innate and adaptive immune responses and altered airway microbiome.4
RSV prevention
Attention has recently turned to RSV prevention because of the large burden on healthcare and potential for long-term sequelae of early RSV infection. Options for RSV prevention include monoclonal antibodies for infants under 2 years of age and vaccination for adults.
Monoclonal antibodies
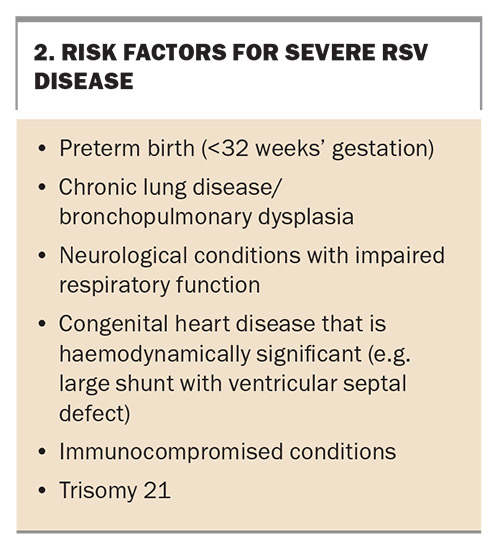
Palivizumab was the first approved monoclonal antibody developed, targeting the F surface protein. This is administered monthly via intramuscular injections throughout RSV season to high-risk populations, including preterm infants and those with congenital heart disease (Box 2).6 This has resulted in a statistically significant reduction in hospitalisations compared with placebo.7
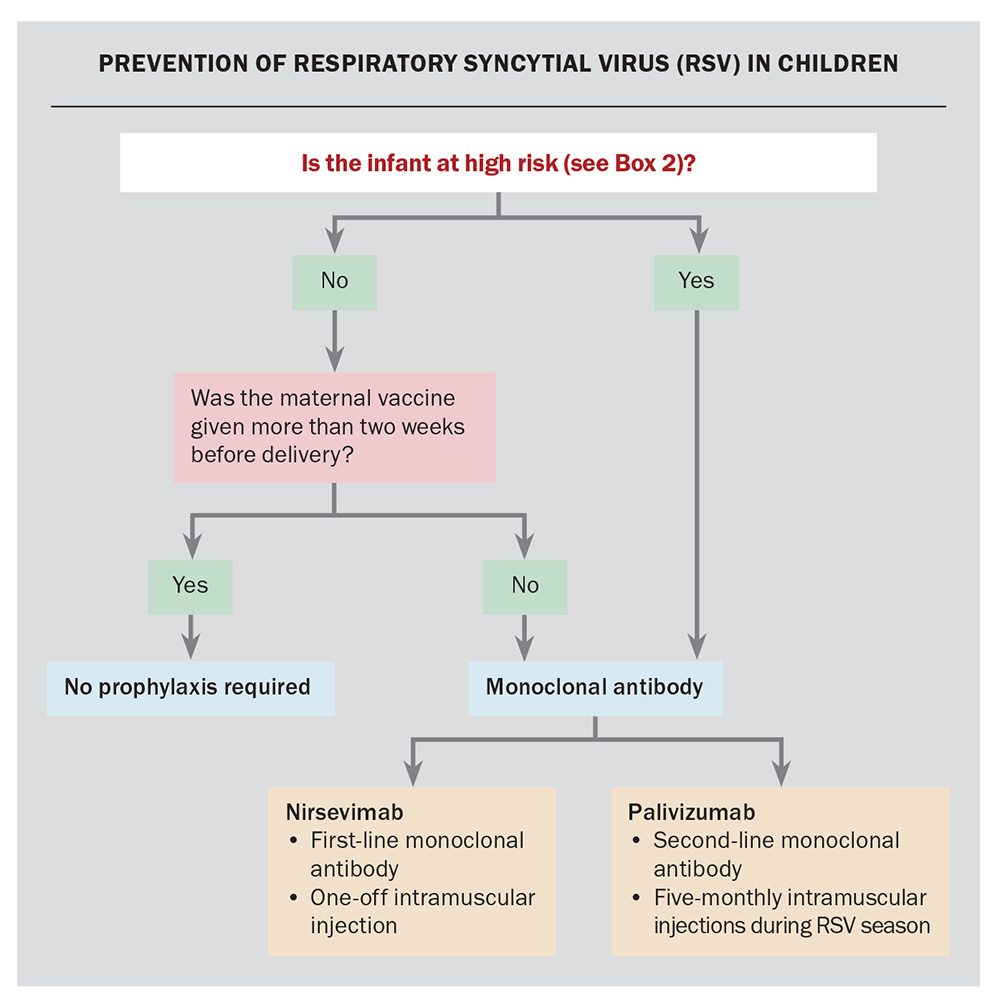
Nirsevimab is the newer, and now preferred, long-acting monoclonal antibody, which targets the pre-F protein. It is also administered via intramuscular injection. However, the longer half-life means that a single dose provides coverage for the full RSV season. It is recommended for infants with inadequate maternal RSV vaccination. Nirsevimab is also recommended for young infants who have additional medical risk factors for severe RSV disease, regardless of maternal vaccination status (Flowchart).
Nirsevimab has been shown to reduce medically attended RSV infections, hospital admissions and severe RSV infections in both term and preterm infants.8 For best protection, this should be given before their first RSV season.
Vaccination
Although there are currently no RSV vaccinations available for children, there are vaccines available for use in adults. In Australia, both Abrysvo and Arexvy are available; however, Abrysvo is the only vaccine approved for use in pregnant women. Abrysvo should be offered to pregnant women regardless of the time of year. For adequate protection, this must be administered between 28 and 36 weeks’ gestation and at least two weeks before delivery. If the child is born less than two weeks after administration of the vaccine, the current recommendation is that they should also receive nirsevimab for adequate protection.
Harry’s progress
You refer Harry to the local emergency department, where he is diagnosed with RSV bronchiolitis. Harry’s increased work of breathing persists despite nasal suctioning, continuous nasogastric feeds, low flow oxygen and, finally, high-flow nasal cannula oxygen. He is subsequently admitted to the paediatric intensive care unit, and commenced on continuous positive airway pressure for 48 hours. His respiratory support is gradually weaned off, and he is discharged from hospital and feeding well seven days later. MT
COMPETING INTERESTS: None.
References
1. Jain H, Schweitzer JW, Justice NA. Respiratory syncytial virus infection in children. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK459215/ (accessed December 2024).
2. Saravanos GL, Sheel M, Homaira N, et al. Respiratory syncytial virus-associated hospitalisations in Australia, 2006-2015. Med J Aust 2019; 210: 447-453.
3. Hamaira N, Oei JL, Mallitt KA, et al. High burden of RSV hospitalization in very young children: a data linkage study. Epidemiol Infect 2016; 144: 1612-1621.
4. Zar HJ, Cacho F, Kootbodien T, et al. Early-life respiratory syncytial virus disease and long-term respiratory health. Lancet Respir Med 2024; 12: 810-821.
5. Allinson JP, Chaturvedi N, Wong A, et al. Early childhood lower respiratory tract infection and premature adult death from respiratory disease in Great Britain: a national birth cohort study. Lancet 2023; 401: 1183-1193.
6. Australian Technical Advisory Group on Immunisation. Australian Immunisation Handbook. Respiratory syncytial virus. Australian Government Department of Health and Aged Care, Canberra; 2022.
7. Garegnani L, Styrmisdottir L, Roson Rodriquez P, et al. Palivizumab for preventing severe respiratory syncytial virus (RSV) infection in children. Cochrane Database Syst Rev 2021; 11(11): CD013757.
8. Bourassa M, Lands L. Preventative therapies for respiratory syncytial virus (RSV) in children: Where are we now? Paediatr Respir Rev 2024; 49: 24-27.