COPD exacerbations: a hearty opportunity

Chronic obstructive pulmonary disease (COPD) exacerbations are common. Simultaneous cardiovascular involvement is frequent and affects prognosis adversely. COPD exacerbations are opportunities to optimise lung health, and to enhance cardiovascular diagnosis and treatment.
- Cardiovascular disease (CVD) is the leading cause of death in patients with chronic obstructive pulmonary disease (COPD); yet, cardiac issues are underdiagnosed in these patients.
- Bronchitis or an infection in a current or ex-smoker might be an exacerbation of undiagnosed COPD and also serve as an unstandardised cardiac stress test.
- COPD exacerbations are opportunities to address the gap in care that these patients receive and improve both pulmonary and cardiac outcomes.
- Coronary artery disease is very common in people with COPD, a population with numerous cardiovascular risk factors, which emphasises the need for comprehensive care.
Chronic obstructive pulmonary disease (COPD) affects around one in seven adults over the age of 40 years in Australia and the prevalence of COPD is expected to rise as the population ages.1
Exacerbations of COPD are impactful. Exacerbations are frightening for patients and signal adverse consequences, including accelerated lung function decline and mortality. They are a leading cause of preventable Australian hospitalisations.2 They are also a timely opportunity for the astute clinician to intervene and change the course of lung and heart disease.
COPD and cardiovascular disease (CVD) are intimately linked. Large, well-conducted pharmaceutical studies have shown that CVD is the most common cause of death in patients with mild and moderate COPD.3
Cardiac involvement is important in COPD exacerbations. For example, elevations in levels of cardiac biomarkers are detectable in up to 75% of patients who are hospitalised with exacerbations and lead to a greater likelihood of readmission and mortality.4 When rigorously examined with CT scanning, severe but treatable CVD is present in most people hospitalised with exacerbations of COPD.5 Deaths among patients with severe COPD are more frequently attributed to COPD than to CVD, but because cardiac involvement is often underdiagnosed, cardiovascular intervention could also improve outcomes in this population. Importantly, cardiovascular undertreatment is widespread in people with COPD and this represents a large gap for care optimisation.6-10 This article focuses on a practical approach to CVD assessment during and after COPD exacerbation.
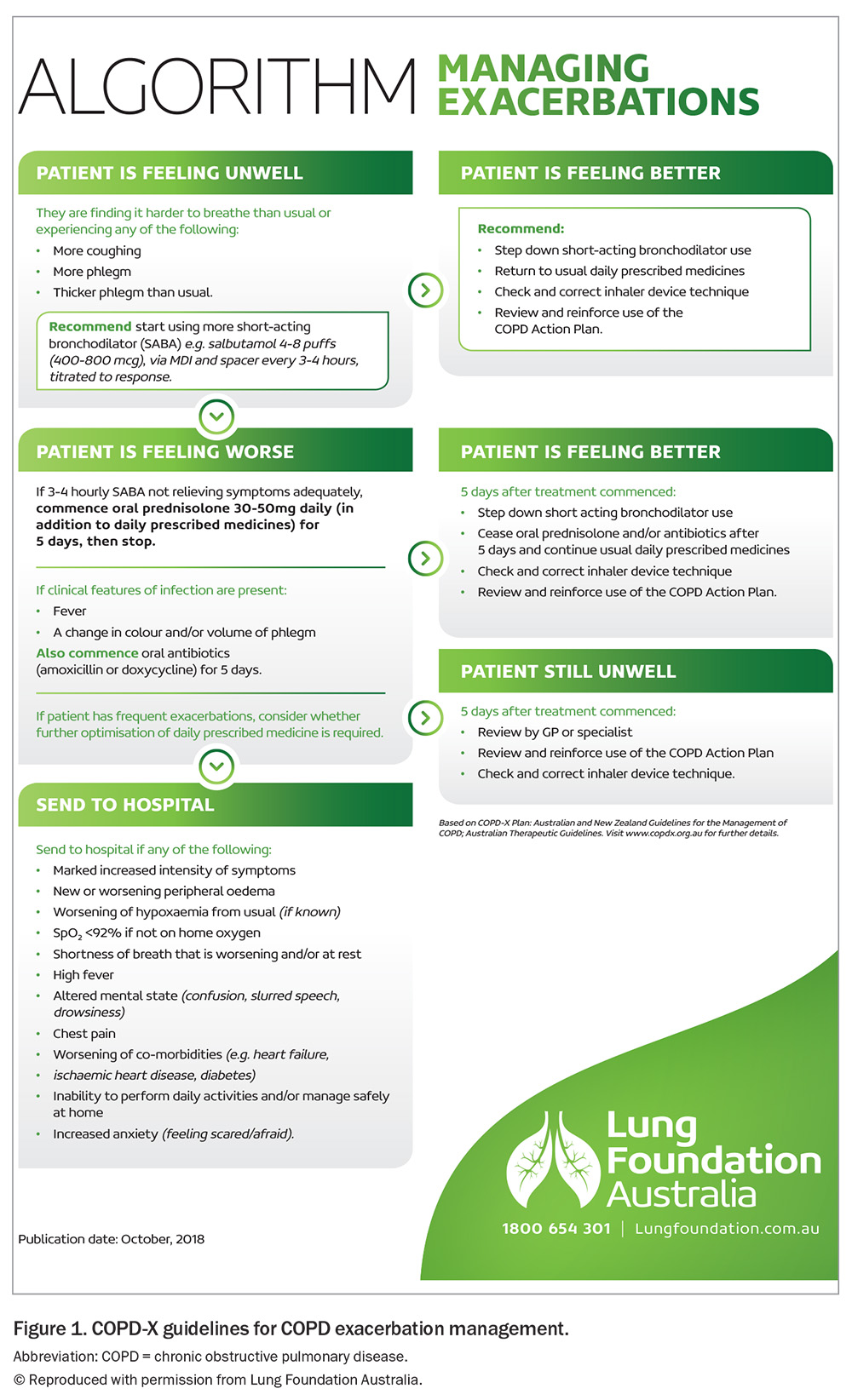
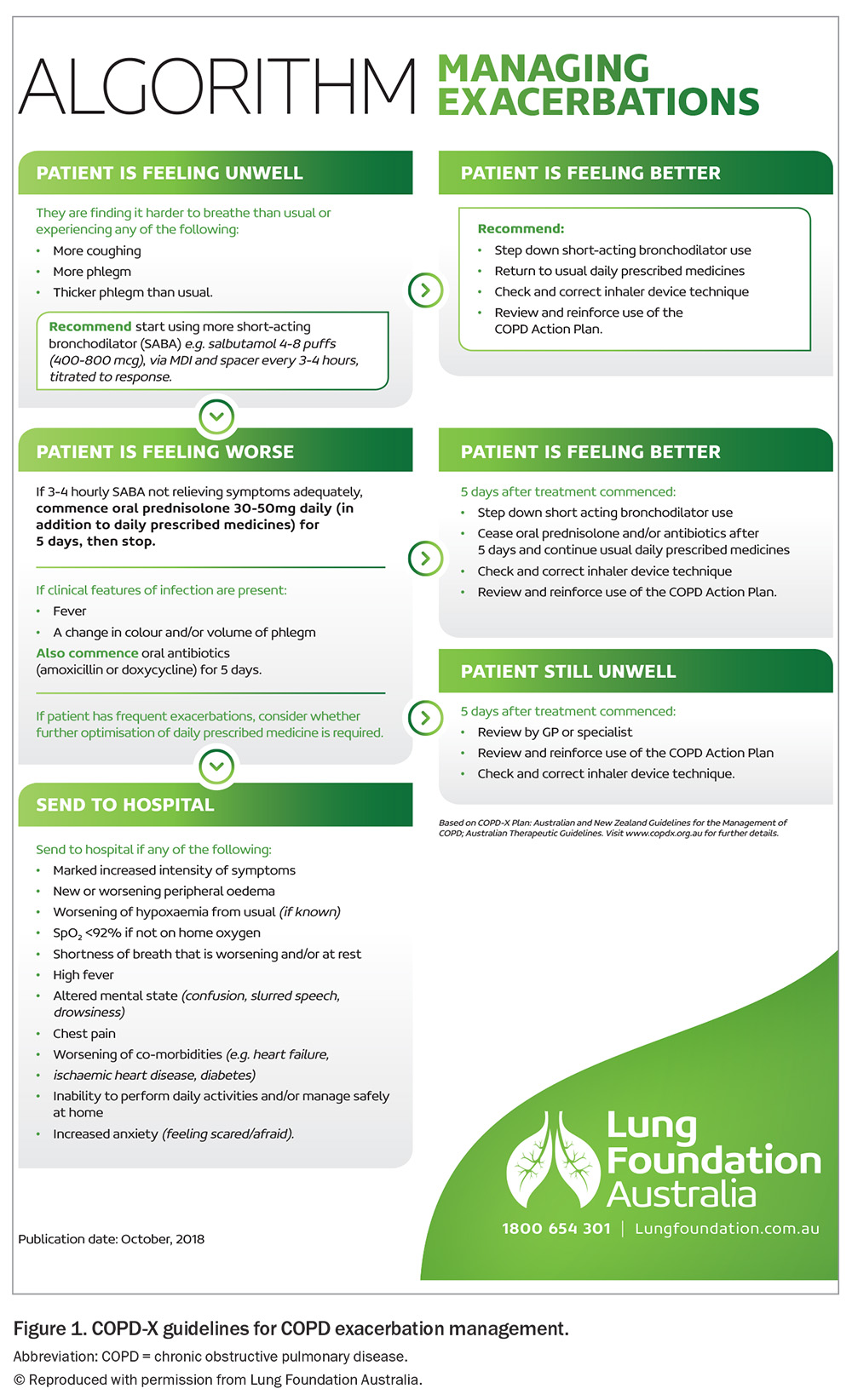
The COPD-X Plan
Guidelines for COPD management, including exacerbations, are available from the COPD-X plan (https://www.copdx.org.au), the Australian and New Zealand guidelines for COPD management. The standard approach to managing exacerbations is outlined in Figure 1. Although cardiovascular assessment is mentioned in the COPD-X guidelines, no specific approach has been outlined because prospective studies are scant.
Cardiovascular risk factors cluster in people with COPD, so it is reasonable to maintain a low threshold to performing case-finding cardiac investigations, but also to consider performing CVD risk factor assessment.
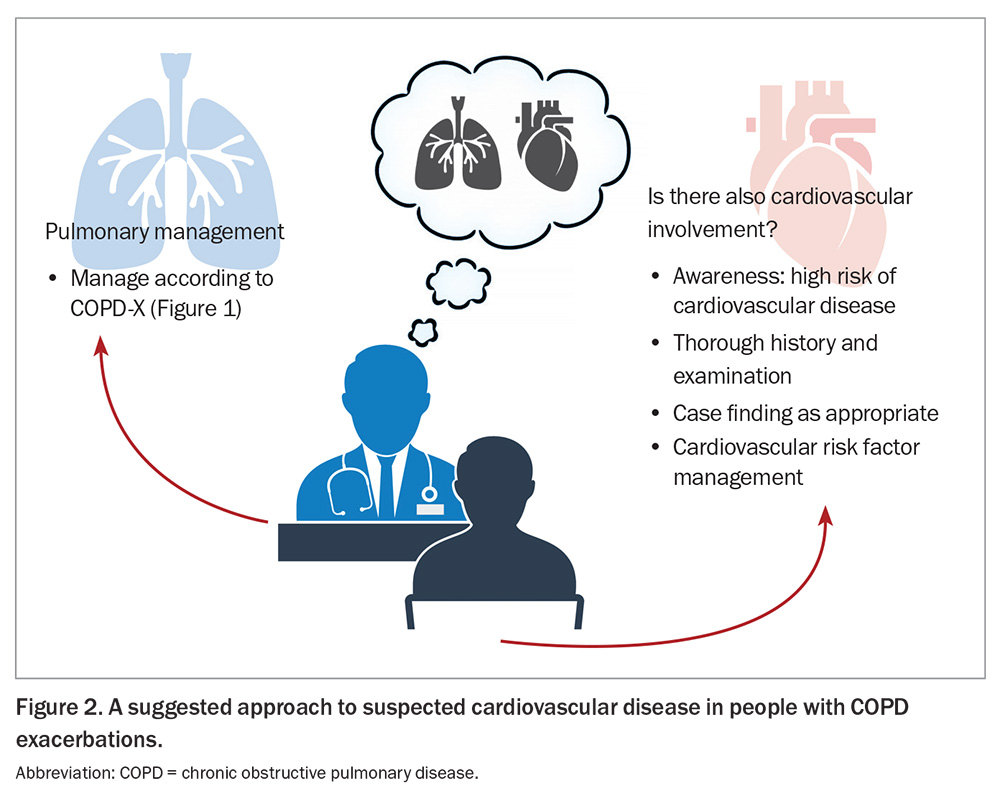
A suggested approach to suspected CVD in patients with COPD
There are two key steps in our suggested approach to potential CVD in patients with COPD: first, be aware of the possibility of CVD in patients with COPD; and second, diagnose and treat CVD or cardiovascular risk factors (Figure 2).
COPD exacerbations and CVD
The pretest probability of CVD in patients with COPD is typically high, as this population is enriched with cardiovascular risk factors. Individuals with COPD are generally older, less physically active and are current or ex-smokers. By definition, they have airflow limitation, which is an independent cardiovascular risk factor – for every 10% decrease in forced expiratory volume in one second, cardiovascular mortality increases by 28%.11 Overall, populations with COPD are at a two- to threefold increased risk of CVD compared with controls.12
During exacerbations, many factors can be active separately or together to produce cardiovascular events. Two-thirds of exacerbations are associated with infection (a proinflammatory state). Hypoxia, tachycardia, arrythmias, sudden elevations in pulmonary pressure, arterial stiffness and pulmonary hyperinflation can all contribute to cardiovascular events.4
COPD exacerbations have been likened to an unstandardised, unscheduled cardiac stress test.6 Cardiovascular event rates, including mortality, spike during exacerbation, and incidence rates remain elevated in the subsequent months.13
How might CVD present in a person with COPD?
CVD during COPD exacerbations may present in the following different ways.4,5
- CVD may mimic a COPD exacerbation. This can masquerade as a ‘refractory’ COPD exacerbation – one that does not respond as expected to standard airway-directed management.
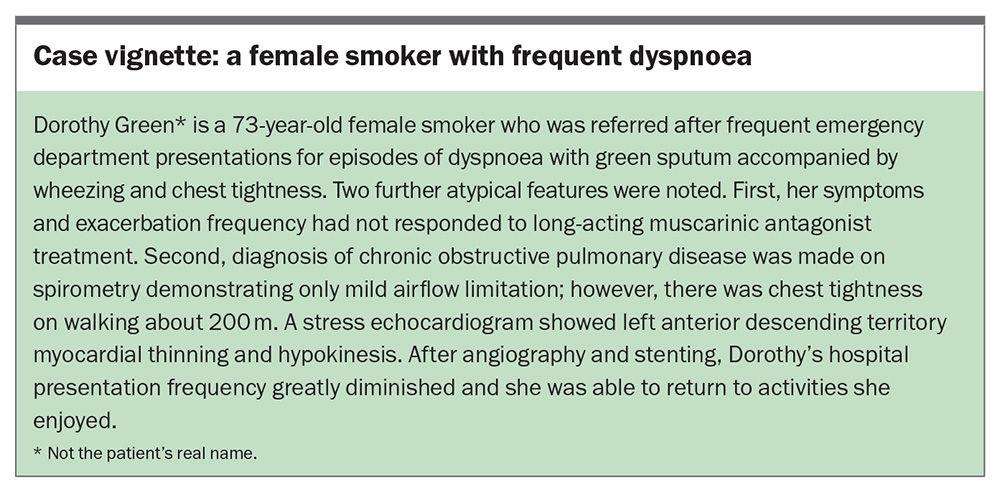
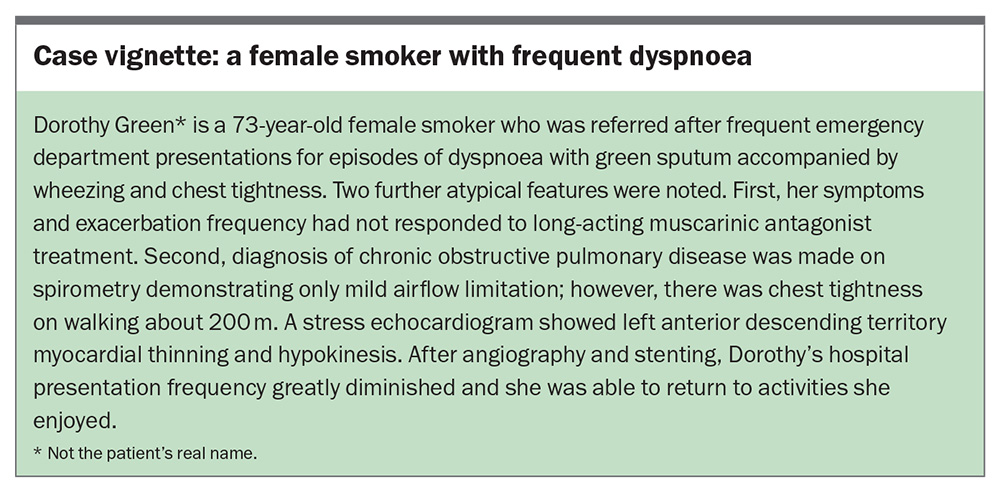
- CVD may diminish the ability of a patient to ‘tolerate’ the exacerbation, and a relatively minor airway disturbance may present with disproportionate or atypical symptoms. A case vignette of a real patient that highlights this is outlined in the Box.
- CVD may complicate COPD exacerbations – a phenomenon exemplified by type 2 (demand) myocardial infarction with elevated troponin levels4 – and may also present with new arrythmias (typically atrial fibrillation) and new heart failure.
- Importantly, CVD in people with COPD may also remain subclinical.
Diagnosis of CVD
Diagnosing CVD during COPD exacerbations relies on clinical acumen and a high index of suspicion. This is because manifestations of COPD and CVD can overlap and hints may be subtle.
For instance, it may be tempting to attribute symptoms including breathlessness, atypical chest pain and tightness to COPD exacerbations; however, CVD can present similarly. Careful assessment is suggested because it may yield clues to concurrent CVD.
- Is there chest pain or tightness and is it exertional? Could the chest pain be angina?
- Is there a background history of cardiac disease that now may be worsened?
- Are there palpitations?
- Is orthopnoea prominent?
- Is breathlessness out of proportion to spirometric airflow limitation?
- Does this patient avoid nonacute or preventive care, and thus may there be a greater opportunity for cardiovascular diagnosis and risk factor reduction?
The examination can often be helpful. For example:
- radial artery palpation may lead to a suspicion of atrial fibrillation, which complicates many exacerbations
- jugular venous pulsation elevation may hint at right heart involvement
- peripheral oedema may hint at cardiac failure
- bilateral basal crackles on auscultation could be a sign of heart failure.
Put another way, it is useful to have a low threshold to think that a supposedly straightforward COPD exacerbation might also have cardiovascular involvement.
The acute treatment of COPD exacerbations should follow COPD-X recommendations (Figure 1). Excessive beta-agonist use can lead to lactic acidosis, Takotsubo cardiomyopathy and even myocardial infarction; therefore, limiting administration to the maximum dose recommended in the COPD-X plan is suggested.4,6 This equates to four to eight puffs of salbutamol (400 to 800 mcg) via a metered dose inhaler or spacer every three to four hours. When supplemental oxygen is used, ensuring that oxygen saturations are maintained at 88 to 92% can prevent adverse respiratory and cardiac consequences.14
After recovery, COPD should be managed according to the COPD-X guidelines for stable COPD (https://lungfoundation.com.au/resources/stepwise-management-of-stable-copd). Large studies of inhaled triple therapy combinations (long-acting muscarinic antagonist, long-acting beta agonist, corticosteroid) in patients with COPD showed reductions in all-cause mortality driven by reductions in cardiovascular death; however, the data are not strong enough to recommend escalation to triple therapy solely to prevent cardiovascular mortality.15,16 Smoking cessation, encouraging a healthy lifestyle that includes exercise and considering pulmonary rehabilitation should be the cornerstones of management.
Beyond cardiovascular case finding, COPD exacerbations can be viewed as an opportunity to review cardiovascular risk. Dutch primary care guidelines recommend that cardiovascular risk assessment should be performed in all patients with COPD.17 In a retrospective study of the impact of the new Dutch guidelines on cardiovascular risk management in patients with COPD, 90% of patients with COPD were found to be at a high or very high risk of a fatal cardiovascular event (>5% risk over 10 years).17
CVD in patients with COPD: a treatment gap
Australian data indicate that 55% of patients hospitalised with COPD exacerbations have coronary atherosclerosis at a level at which guidelines recommend treatment.5 This is concordant with global data. A US study found that nearly 90% of people with COPD had coronary artery disease on CT coronary angiography.18 Coronary artery disease is highly prevalent in people with COPD and it may be prudent to investigate individuals who manifest ‘type 2 myocardial infarction’ or ‘troponin leaks’ for coronary artery disease (see case vignette in Box).
Despite an elevated cardiovascular risk, studies have consistently shown that treatments for major cardiovascular conditions including coronary disease, myocardial infarction and heart failure are routinely underprescribed in populations with COPD. Over half of all patients do not receive optimal treatment for these conditions, irrespective of the indication for treatment.5,7,8 A review of treatments may therefore identify a gap that can provide genuine therapeutic benefit.
Some therapeutic reluctance has traditionally been present owing to concerns regarding beta-blocker use in COPD; however, beta-blockers are generally safe in patients with COPD, as are aspirin, statins, ACE inhibitors and neprilysin inhibitors.6
When diagnostic or therapeutic uncertainty exists (e.g. if asthma overlap is suspected, which might contraindicate beta-blocker use), specialist respiratory or cardiac referral could be considered.
Conclusion
COPD exacerbations are opportunities to not only improve respiratory health but also detect CVD and optimise cardiovascular health in patients with often significant cardiovascular risk. Astute practitioners can address diagnostic and treatment gaps in both lung and heart health to make a meaningful difference. RMT
COMPETING INTERESTS: None.
References
1. Yang I, Dabscheck E, George J, et al. The COPD-X Plan: Australian and New Zealand Guidelines for the management of chronic obstructive pulmonary disease. Version 2.76, September 2024. Available online at: https://copdx.org.au (accessed February 2025).
2. Australian Institute of Health and Welfare. Admitted patient care 2017-18: Australian hospital statistics. Health service series no. 90; AIHW Cat. no. HSE 225. Canberra: AIHW; 2019. Available online at: https://www.aihw.gov.au/getmedia/df0abd15-5dd8-4a56-94fa-c9ab68690e18/aihw-hse-225.pdf.aspx?inline=true (accessed March 2021).
3. McGarvey LP, Magder S, Burkhart D, et al. Cause-specific mortality adjudication in the UPLIFT COPD trial: findings and recommendations. Respir Med 2012; 106: 515-521.
4. MacDonald MI, Shafuddin E, King PT, Chang CL, Bardin PG, Hancox RJ. Cardiac dysfunction during exacerbations of chronic obstructive pulmonary disease. Lancet Respir Med 2016; 4: 138-148.
5. Leong P, MacDonald MI, King P, et al. Treatable cardiac disease in hospitalised COPD exacerbations. ERJ Open Res 2021; 7: 00756-2020.
6. Leong P, Macdonald MI, Ko BS, Bardin PG. Coexisting chronic obstructive pulmonary disease and cardiovascular disease in clinical practice: a diagnostic and therapeutic challenge. Med J Aust 2019; 210: 417-423.
7. Rasmussen DB, Bodtger U, Lamberts M, et al. Beta-blocker, aspirin, and statin usage after first-time myocardial infarction in patients with chronic obstructive pulmonary disease: a nationwide analysis from 1995 to 2015 in Denmark. Eur Heart J Qual Care Clin Outcomes 2020; 6: 23-31.
8. Reed RM, Eberlein M, Girgis RE, et al. Coronary artery disease is under-diagnosed and under-treated in advanced lung disease. Am J Med 2012; 125: 1228.e13-1228.e22.
9. Neef PA, McDonald CF, Burrell LM, Irving LB, Johnson DF, Steinfort DP. Beta-blockers are under-prescribed in patients with chronic obstructive pulmonary disease and co-morbid cardiac disease. Intern Med J 2016; 46: 1336-1340.
10. Rothnie KJ, Smeeth L, Herrett E, et al. Closing the mortality gap after a myocardial infarction in people with and without chronic obstructive pulmonary disease. Heart 2015; 101: 1103-1110.
11. Sin DD. Chronic obstructive pulmonary disease as a risk factor for cardiovascular morbidity and mortality. Proc Am Thoracic Soc 2005; 2: 8-11.
12. Chen W, Thomas J, Sadatsafavi M, FitzGerald JM. Risk of cardiovascular comorbidity in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Lancet Respir Med 2015; 3: 631-639.
13. Wang M, Lin EP-Y, Huang L-C, Li C-Y, Shyr Y, Lai C-H. Mortality of cardiovascular events in COPD patients with preceding hospitalized acute exacerbation. Chest 2020; 158: 973-985.
14. Barnett A, Beasley R, Buchan C, et al. Thoracic Society of Australia and New Zealand Position statement on acute oxygen use in adults: ‘swimming between the flags’. Respirology 2022; 27: 262-276.
15. Lipson DA, Barnhart F, Brealey N, et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med 2018; 378: 1671-1680.
16. Rabe KF, Martinez FJ, Ferguson GT, et al. Triple inhaled therapy at two glucocorticoid doses in moderate-to-very-severe COPD. N Engl J Med 2020; 383: 35-48.
17. Nies LM, Looijmans-van den Akker I, Rozendaal L, Baar B, Vos RC, Hart HE. The impact of the new Dutch guideline on cardiovascular risk management in patients with COPD: a retrospective study. BJGP Open 2021; 5(1): bjgpopen20X101139.
18. Macleod MA, Knott KD, Allinson JP, et al. Prevalence and clinical correlates of radiologically detected coronary artery disease in COPD: a cross-sectional observational study. Am J Respir Crit Care Med 2024 Dec 16; e-pub (https://doi.org/10.1164/rccm.202404-0838oc).