Systemic lupus erythematosus: challenging for both diagnosis and management
Despite improvements in the treatment of systemic lupus erythematosus in recent years, patients can still suffer profound morbidity, with significant impact on quality of life. A coordinated approach to management is crucial.
Systemic lupus erythematosus (SLE) is a multisystem autoimmune disease of unknown cause that can present with a variety of clinical manifestations.1,2 The most common symptoms and signs include fatigue, rashes and arthralgias, but any organ system can be involved (Figure 1).3 The wide-ranging and nonspecific nature of these symptoms may make early diagnosis challenging and contribute to problems with both under- and overdiagnosis. SLE more commonly affects women of childbearing age, as well as people of certain ethnic backgrounds, such as Asian and African people.4 In Australia, it affects Aboriginal people more commonly than non-Aboriginal people.4
Although improvements in care have led to a survival rate of more than 90% at five years, patients with SLE often have profound morbidity from the disease and its treatment, with a significant impact on their quality of life.4 SLE is a disease characterised by ‘flares’ of activity over time. Careful monitoring of the disease and consideration of the side effects of treatment are needed. As SLE often affects young women, pregnancy planning needs to be considered. As with many chronic diseases, close collaboration between the patient, GP and involved specialists leads to the best long term outcomes.
Clinical manifestations
Constitutional
Constitutional features such as fatigue, fever and weight loss are likely to affect most patients with SLE at some point, and it is crucial that other possible contributing factors are excluded. Fatigue is a very common complaint in patients with SLE and is often associated with coexistent conditions such as anaemia, hypothyroidism, fibromyalgia and sleep and mood disorders. Although fever and weight loss may signal disease activity, they should raise concern for other serious problems such as infection, particularly in patients taking long term corticosteroids or other immunosuppressive treatments.5
Cutaneous
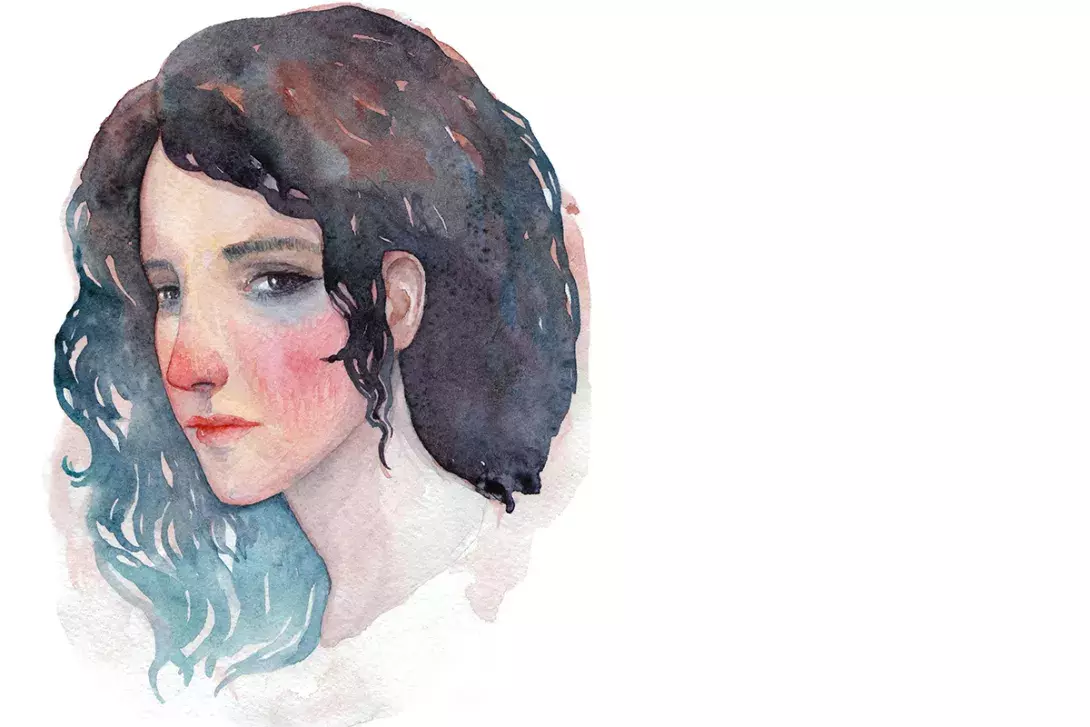
The cutaneous manifestations of SLE often occur in sun-exposed areas. Cutaneous lupus erythematosus can be classified into three main categories: acute, subacute and chronic.6 The chronic cutaneous lupus erythematosus subtype occurs most commonly.6 Patients with SLE often present with a malar rash or a discoid rash (Figure 2 and Figure 3), which are examples of acute cutaneous lupus erythematosus and chronic cutaneous lupus erythematosus, respectively. A malar rash, or ‘butterfly’ rash, presents as either flat or raised erythema over the malar prominence, with sparing of the nasolabial folds (Figure 2).2 A discoid rash presents as raised erythematous disk-like plaques, which can be widespread in nature and can lead to scarring alopecia (Figure 3).7 Often patients with SLE have photo-sensitivity, whereby sunlight induces or exacerbates cutaneous lesions.2,3 Other cutaneous manifestations of SLE include Raynaud’s phenomenon, alopecia and mouth ulcers.
Musculoskeletal
Arthritis is one of the most common and earliest manifestations of SLE, affecting up to 95% of patients.8 It classically presents as a symmetrical polyarthritis predominantly affecting the small joints.8 It is important to differentiate between inflammatory arthritis and other causes of widespread pain, such as fibromyalgia and vitamin D deficiency. Rarely, patients may develop Jaccoud’s arthropathy, a deforming arthropathy that arises in the context of joint subluxation and ligamentous laxity, without erosion of the joints.8
Serosal
Serositis, a common feature of SLE, may affect the pericardium, pleura and peritoneum, resulting in pain and the accumulation of fluid, and potentially leading to fibrosis in the long term.9,10 Patients with pericarditis and pleuritis often present with pleuritic chest pain, with or without dyspnoea, and other causes of pleurisy such as pneumonia must be considered. It is important to note that patients with SLE are at greater risk of venous thromboembolism, particularly if they have anti- phospholipid antibodies, and pulmonary embolism must also be excluded.
Renal
Lupus nephritis, which affects about 30 to 50% of patients with SLE, poses a major risk for morbidity and mortality, with 10% of affected patients developing end-stage renal failure.11 Patients often present with proteinuria, microscopic haematuria or renal insufficiency, thereby signifying the importance of undertaking a urinalysis and measuring the serum creatinine and eGFR.11 The definitive diagnosis of lupus nephritis is based on a renal biopsy, which can provide useful prognostic information depending on the histological features. Further, the treatment approach varies widely depending on the histology and classification of the renal lesions.
Haematological
Patients with SLE may develop anaemia, leukopenia or thrombocytopenia. Anaemia may be secondary to nutritional deficiency, anaemia of chronic disease or autoimmune haemolytic anaemia. Leukopenia may be secondary to lymphopenia or neutropenia, which may correlate with other features of disease activity or may be a side effect of immunosuppressive treatment.
Neuropsychiatric
The neuropsychiatric manifestations of SLE can affect the central and peripheral nervous systems, and include delirium, psychosis and seizures.7,12 More broadly, it is recognised that subtle ‘brain fog’ and depression occur frequently in patients with SLE. Less than 40% of cases of neuropsychiatric lupus are a direct consequence of the disease (that may therefore respond to immunosuppression), with the remainder attributable to factors such as complications of treatment including corticosteroid psychosis and infection.13
Pregnancy and family planning
Pregnancy in women with SLE is associated with an increased risk of complications for both the mother and the baby. Despite this, most women with SLE are able to have successful pregnancies. The biggest predictors of outcome include the presence of antiphospholipid antibodies (increased risk of miscarriage and thrombosis), the presence of SSA and SSB antibodies (increased risk of congenital fetal heart block and neonatal lupus) and the presence of disease activity, hypertension or active lupus nephritis within the six months prior to pregnancy. It is now common to continue compatible medications throughout pregnancy (including corticosteroids, hydroxychloroquine and azathioprine), and this has led to better pregnancy outcomes. In some cases, other medications such as aspirin and heparins may be needed. Ideally, pregnancy care should be provided in centres with experience in managing SLE in pregnant women.
Women with SLE should be advised about contraception so as to avoid pregnancy during periods of high disease activity or while using teratogenic agents, which could pose a risk to both the mother and the baby. In general, all patients with SLE can be offered an intrauterine device, unless there is a contraindication from a gynaecological perspective.14 Patients with stable SLE who are negative for antiphospholipid antibodies can potentially be offered combined hormonal contraceptives – generally the lowest possible dose of oestrogens is preferred so as to avoid exacerbating the disease or increasing the risk of thrombosis.14 Patients who are positive for antiphospholipid antibodies with or without antiphospholipid syndrome can potentially be offered progestin-only hormonal contraception, although the risk of thrombosis needs to be carefully considered.14
Diagnosis
It is important to remember that SLE is a clinical diagnosis supported by serological testing – there is no diagnostic test. In recent years, there have been attempts to refine ‘classification criteria’ using various permutations of the well-recognised clinical and laboratory features that are seen in SLE. In 2019, the European League Against Rheumatism (EULAR) and the American College of Rheumatology (ACR) proposed new classification criteria for SLE,7 thereby replacing the 2012 Systemic Lupus International Collaborating Clinics (SLICC) classification criteria.15 The 2019 EULAR/ACR classification criteria, which have a sensitivity of 96.1% and a specificity of 93.4% compared with the gold standard of clinician diagnosis, are useful for the standardisation of patients enrolled in clinical trials and as guides to the widespread features of the disease (Box).7 However, classification criteria should not be used directly as ‘diagnostic criteria’, and ultimately, clinician diagnosis remains the gold standard.
The hallmark immunological test for SLE is the antinuclear antibody (ANA) test. It has a high sensitivity (>98%), meaning that a repeatedly negative result makes SLE very unlikely.2 Unfortunately, it has low specificity for SLE, with a positive ANA result seen in many other chronic diseases and up to 20% of the normal healthy population.2 Other immunological tests that are important to consider include anti-double-stranded (ds) DNA antibodies and anti-Smith antibodies, which occur in less than half of patients with SLE at the time of diagnosis but are highly specific for SLE. Further, levels of the C3 and C4 complement proteins and antiphospholipid antibodies (i.e. lupus anticoagulant, anticardiolipin antibodies and anti-beta-2 glycoprotein 1 antibodies) should be assessed in patients with the disease. Of these, the anti-dsDNA and complement levels can be used to monitor disease activity, whereby the anti-dsDNA rises and the complement levels drop with flares of disease activity. Changes in the ANA test, on the other hand, do not reflect changes in disease activity and it should not be repeated on a routine basis.
Management
In SLE, the goals of management are to induce remission, prevent flares and minimise the side effects of therapy. Treatment intensity should be titrated to the seriousness of the disease activity and must be directed at preventing complications of active disease and maintaining quality of life. If induction of remission is not possible, the aim should be towards achieving a low level of disease activity. Risk factors for higher likelihood of flaring include younger age at onset, the presence of renal disease, active serology (increased anti-dsDNA and reduced C3 and C4 levels) and lack of use of hydroxychloroquine.16
General measures
All patients with SLE should be educated about the importance of sun protection (and subsequent vitamin D supplementation) because sunlight may induce or exacerbate cutaneous lesions and provoke systemic flares of the disease. Education concerning the fluctuating nature of the condition and the need for monitoring and preventive approaches is also important. Fibromyalgia symptoms (noninflammatory pain and fatigue) occur in as many as 40% of people with SLE and do not generally respond to immunosuppressive treatments, and this should be acknowledged. In addition, education regarding appropriate sleep and exercise strategies should be provided where relevant.
There are a number of aspects of the long-term management of SLE in which the GP plays a crucial role. Patients with SLE are at greater risk of cardiovascular disease, and should therefore be advised against smoking. Comorbidities such as obesity, hypertension, dyslipidaemia and diabetes need to be controlled. Patients are also at greater risk of infection, as a consequence of either their condition or their treatment. Thus, they should be encouraged to receive immunisations against influenza and pneumococcal disease.16 Live vaccinations may need to be avoided in patients who are significantly immunosuppressed, due to the potential to trigger disseminated infection.2
Corticosteroids
Although corticosteroids are effective for the management of various aspects of SLE, the aim should be for the dose of prednisone to not exceed 7.5 mg daily in the long term because of its significant side-effect profile.16 Pulsed methylprednisolone at high doses (e.g. 1 g daily for three days) is reserved for patients with serious complications of SLE, such as renal or neuropsychiatric manifestations.16 Appropriate treatment of corticosteroid side effects, including osteoporosis and metabolic complications, is needed.
Hydroxychloroquine
Hydroxychloroquine should be used by all patients with SLE, unless there is a contraindication. The daily dose of hydroxychloroquine should not exceed 5 mg/kg of real bodyweight in the long term, although this level is commonly exceeded if necessary during flares of the disease. Hydroxychloroquine is usually continued long term, provided that there is no toxicity. It can be given in conjunction with other immunosuppressive treatments and continued throughout pregnancy. There is high-quality evidence to suggest that hydroxychloroquine reduces disease activity in SLE, including during pregnancy, and that it reduces mortality.17 Further, there is moderate quality evidence to suggest that hydroxychloroquine is protective against irreversible organ damage and thrombotic events.17
The most significant side effect of hydroxychloroquine is retinal toxicity, which is irreversible. The risk of developing retinal toxicity rises with higher daily doses of hydroxychloroquine and longer periods of use. If used at recommended doses, the risk of retinal toxicity is substantially less than 1% up to 5 years and less than 2% up to 10 years.18 In terms of screening for retinal toxicity, patients should undergo a baseline retinal examination with an ophthalmologist within a year of being commenced on hydroxychloroquine, and then annual screening from five years onwards, provided that there are no major risk factors (e.g. pre-existing macular disease).18
Other medications
In cases where corticosteroids and hydroxychloroquine are unable to provide adequate disease control, other medications may need to be added. These treatments are generally off-label and should only be started by specialists experienced in managing patients with SLE. If the disease manifestations are nonrenal in nature, the agents of choice are generally either methotrexate (off-label) or azathioprine. In patients of childbearing age, methotrexate is best avoided due to the risk of teratogenicity. Azathioprine is safe to use in pregnancy. If the manifestations are renal in nature or if the aforementioned agents are proving ineffective in controlling the disease, consideration needs to be given to mycophenolate and cyclophosphamide (both off-label). Occasionally, other off-label treatments are used, such as leflunomide, ciclosporin or tacrolimus.
In lupus nephritis, mycophenolate or cyclophosphamide are the agents of choice for induction of remission, while mycophenolate or azathioprine can be used for maintenance of remission.16 Unfortunately, both mycophenolate and cyclophosphamide pose a risk of teratogenicity, and cumulative cyclophosphamide can lead to infertility and premature menopause.
For difficult to control nonrenal manifestations, belimumab may be considered. Belimumab targets B cells by inhibiting B lymphocyte stimulator protein. It has proven to be modestly effective in clinical trials and is widely used in the US and the UK but has not received PBS funding in Australia, despite being the only new drug approved for SLE in many years. For difficult to control renal or nonrenal manifestations, rituximab may also be considered (off-label). Although this drug failed to meet its primary endpoints in two randomised controlled trials,19,20 there were enough problems with the study designs and outcome measures used that it is still widely used in severe disease. The failure of these (and other) trials has informed current trial design and treatment targets. Recently, there have been several successful early trials targeting other immune pathways such as the interferon alfa pathway, the interleukin 12/23 pathway and the Janus kinase-signal transducer and activator of transcription (JAK/STAT) pathway that hold hope for future therapeutic options.
Conclusion
The myriad of symptoms and signs experienced by patients with SLE, which often present over years, can prove challenging with respect to both diagnosis and management. Early diagnosis, often before fulfilling ‘classification criteria’, is necessary to institute appropriate treatment. On the other hand, overdiagnosis of SLE can occur with indiscriminate ANA testing in people with only vague pain or fatigue, and careful clinical assessment and consideration of the diagnosis is needed. With the use of hydroxychloroquine, judicious and proportionate use of immunosuppressive treatments and better management of treatment side effects, mortality has improved substantially in recent years. The morbidity of SLE remains high, and a coordinated approach between the patient, GP, rheumatologist and other specialists is crucial. MT
SLE and COVID-19
Advice from the authors of this article on SLE and the COVID-19 pandemic is provided in the Box.
