Natriuretic peptides in the diagnosis of heart failure – improving clinical confidence and accuracy
Natriuretic peptide blood testing can increase diagnostic accuracy and facilitate earlier and more appropriate treatment for heart failure, as well as reduce other unnecessary investigations. One test per patient per year is now reimbursed on the Medicare Benefits Schedule for outpatients in Australia to help diagnose or exclude heart failure.
Correction
A correction for this article appears in the January/February 2025 issue of Medicine Today. The online version and the full text PDF of this article (see link above) have been corrected.
- Natriuretic peptide (NP) is released from the ventricular myocardium in response to stretch or stress.
- Measuring NP levels can improve diagnostic accuracy in patients presenting with shortness of breath. If NP levels are below 125 pg/mL, a diagnosis of heart failure is unlikely.
- NP levels correlate with symptoms and with prognosis, but if these levels are reduced in response to treatment, the patient carries a better prognosis.
- One NP test per patient per year is now reimbursed on the Medicare Benefits Schedule for outpatients in Australia to help diagnose or exclude heart failure.
Heart failure (HF) is a common cause of breathlessness leading to impaired quality of life and poor prognosis, but it may be difficult to diagnose as the symptoms are nonspecific. An estimated 511,000 people in Australia (2.1% of the Australian population) have HF.1 There are 67,000 new cases of HF reported per year and 61,000 deaths per year due to HF,2 with HF having a worse prognosis than that of many cancers, including bowel, breast, prostate and bladder cancer.3 Up to 50% of patients diagnosed with HF will not survive five years after diagnosis, with a one-year mortality rate of 30 to 50% in those with shortness of breath at rest or with mild exertion.4
About 158,000 hospitalisations are reported for patients with HF per year, occupying 1.12 million days of hospital stay in Australia with an overall estimated cost of $3.1 billion per year.2 The in-hospital mortality rate in Australia is 6.5%.5 If a patient is hospitalised with HF, there is a 2.65-fold increase in annualised mortality, with a 3.69-fold increase in mortality if hospitalised twice and an almost six-fold increase if hospitalised three or more times, compared with those with HF who have not been hospitalised.6
HF is associated with a poorer quality of life compared with chronic lung disease, angina, arthritis, diabetes and hypertension.7 Seventy-six percent of patients with HF find it difficult to carry out normal activities, 66% have mobility problems, 50% have anxiety and 24% struggle to take care of themselves.8 Patients with HF are heavily comorbid, with 94.5% having two or more comorbidities, such as hypertension in 66%, atrial fibrillation in up to 50%, chronic obstructive pulmonary disease (COPD) in 20%, type 2 diabetes in 40%, chronic kidney disease in over 60% and sleep disordered breathing in more than 50%.9
This article discusses how natriuretic peptide (NP) blood testing is an important tool for the diagnosis and exclusion of HF.
Symptoms and signs of heart failure
HF is a clinical syndrome with typical symptoms and signs that generally occur on exertion but can also occur at rest (particularly when recumbent). These are caused by an abnormality in cardiac structure or function that impairs the ability of the heart to fill with blood at normal pressure (HF with preserved ejection fraction [HFpEF]) or eject blood (HF with reduced ejection fraction [HFrEF]) sufficient to fulfil the needs of organs involved in metabolism.9
The cardinal symptoms of HF are breathlessness, ankle swelling, fatigue, paroxysmal nocturnal dyspnoea, orthopnoea, bloating, palpitations and postural hypotension. Important signs of HF include elevated jugular venous pressure, pulmonary crepitations, peripheral oedema, a third heart sound, a laterally displaced apex beat, pleural effusions, cardiac murmurs, tachycardia, tachypnoea and fluid retention.9,10 However, these symptoms and signs are nonspecific and the diagnosis may be missed or delayed because of clinical complexity, the impact on other organ systems, the fact that these symptoms and signs may mimic other common conditions and their absence in mild or partially treated cases.11
Some factors may make the diagnosis of HF more likely, such as prior myocardial infarction, longstanding hypertension, alcohol misuse, family history of cardiomyopathy or sudden cardiac death, longstanding type 2 diabetes, chronic kidney disease, previous cardiotoxic chemotherapy or advanced age,11 but the clinical diagnosis can be difficult and more accurate diagnostic tools may be required.9 Owing to the difficulty in diagnosing HF, fewer than 50% of patients with HF in Australia are referred by GPs to a cardiologist.12
What is natriuretic peptide?
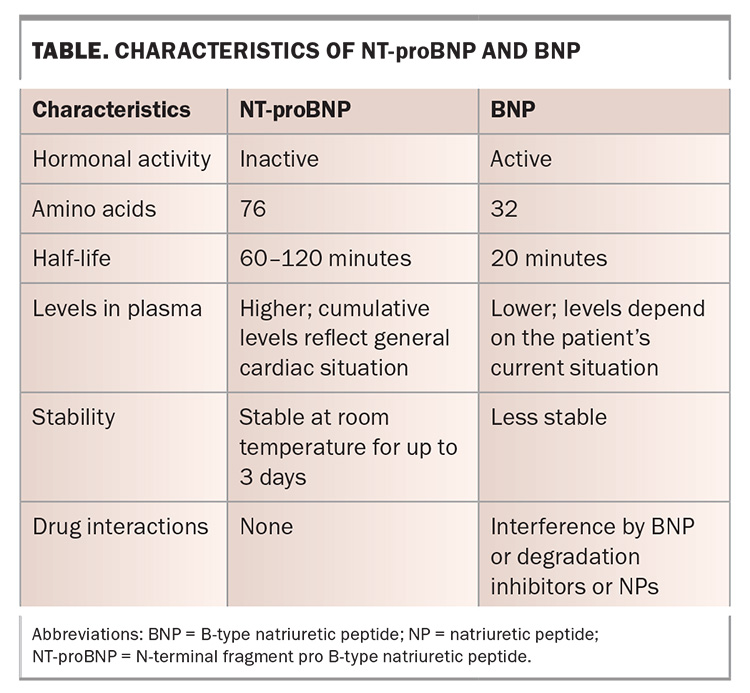
Pro B-type NP (proBNP) is a protein secreted from cardiomyocytes as a physiological response to volume overload, ventricular dilation or stress. proBNP is released and cleaved to the biologically active B-type NP (BNP) and inactive N-terminal fragment proBNP (NT-proBNP).13 The actions of BNP are mediated by the natriuretic peptide receptor-A (found in the kidneys, adrenal glands, heart, vascular smooth muscle and lungs), leading to natriuresis.14 Compared with the active BNP substrate, the inactive NT-proBNP is more stable, with blood samples stable at room temperature for up to three days (Table).15 BNP is removed from the circulation by neutral endopeptidase. Some medications, such as sacubitril/valsartan cause elevations in BNP levels, as their mechanism of action involves reducing the degradation of natriuretic peptides. NT-proBNP levels are not directly affected by medications such as sacubitril/valsartan. In fact, medications that decrease filling pressures lead to a reduction in NT-proBNP levels.16
Plasma levels of NP, including BNP and NT-proBNP, are elevated in patients with HF. There is a strong correlation with left ventricular function and the level of pulmonary congestion when NP levels are measured invasively.17,18 NP levels can help discriminate between patients with HF and without HF in those who have oedema, and NP levels also correlate with the severity of HF symptoms.19 In patients presenting with shortness of breath, NP levels can help discriminate between those with dyspnoea associated with chronic obstructive pulmonary disease and those with HF.19 NP levels are usually higher in those with HFrEF compared with HFpEF,18 but NP levels are inversely correlated with body mass index.20
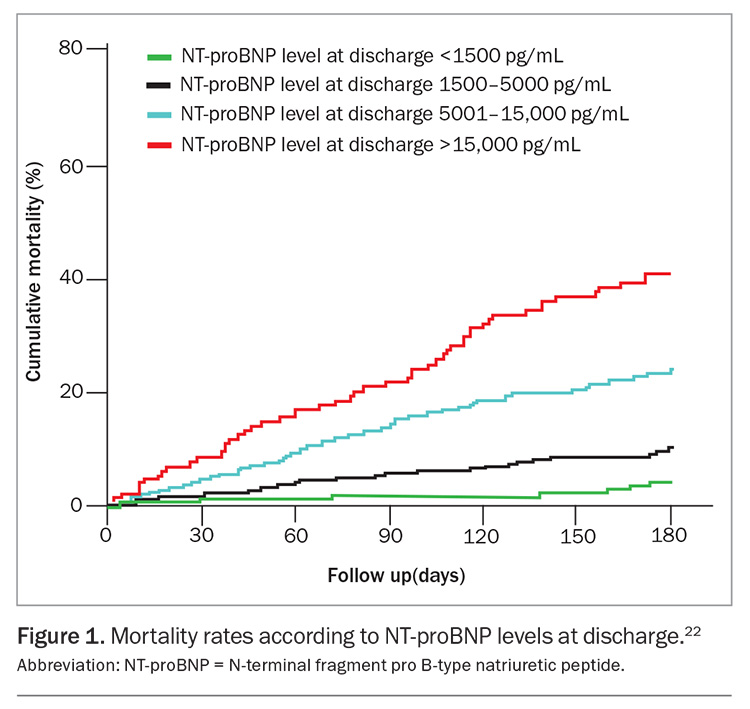
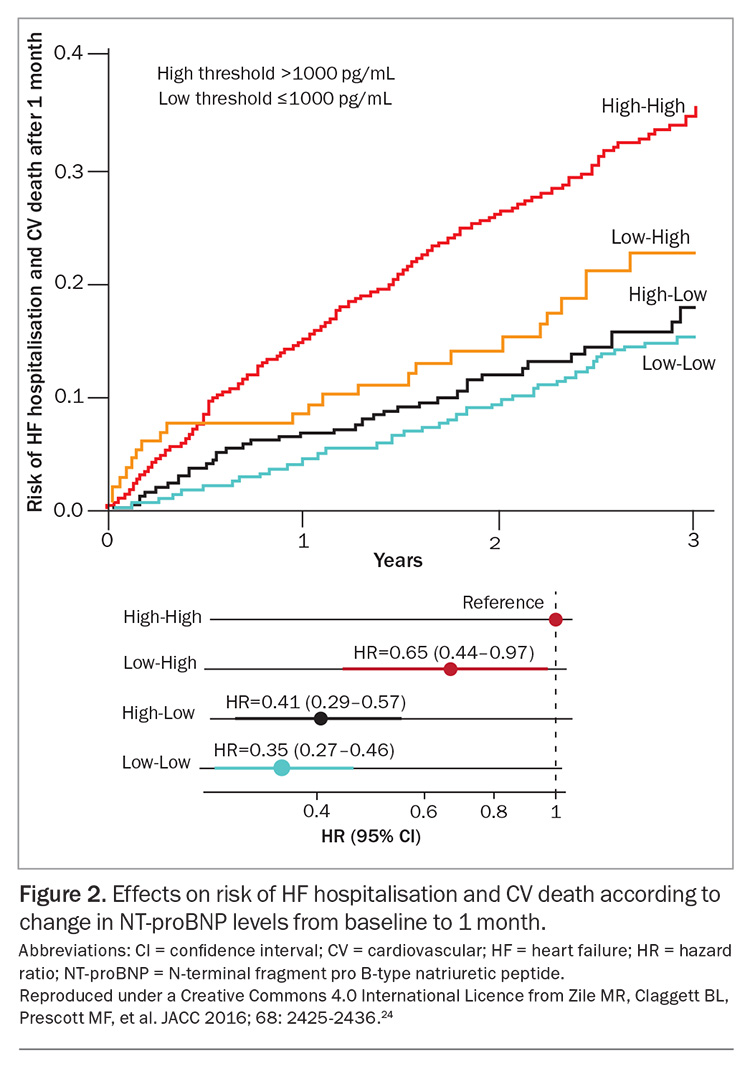
NP levels can help predict prognosis in patients with HF,21 with one study finding a mortality rate of 41% at 180 days in those with NT-proBNP levels greater than 15,000 pg/mL hospitalised with acute decompensated HF (Figure 1).22 Additionally, patients hospitalised with HF who presented with an increase in NT-proBNP levels from admission to discharge had poorer prognosis compared with patients in whom NT-proBNP levels did not change. Patients who presented with a decrease in NT-proBNP levels from admission to discharge had better prognosis.23 A change in NT-proBNP levels is a predictor of subsequent HF hospitalisation and cardiovascular death (Figure 2).24
Apart from HF, other causes of elevated NP levels include advanced age, renal dysfunction, pulmonary embolism, moderate obstructive sleep apnoea, pulmonary hypertension, advanced chronic obstructive pulmonary disease, severe infections, ischaemic or haemorrhagic stroke, extensive burns, cardiotoxic chemotherapy, severe metabolic and hormonal abnormalities and liver dysfunction.9
How can assessing natriuretic peptide levels help establish a diagnosis of heart failure?
NP levels have been shown to assist in the diagnosis of HF, even when other potential competing causes of dyspnoea are present. Elevated NP levels can help identify HF as a cause of dyspnoea in diagnostically challenging scenarios, such as in patients with COPD.19 Breathlessness presents diagnostic challenges in patients with conditions that have significant symptom overlap, such as those with COPD, as HF affects 20 to 32% of these patients.25 An Australian study showed that 16% of patients hospitalised with exacerbations of COPD had severe HF, and in 67% of cases, a HF diagnosis was missed based on clinical assessment and management alone.26
Assessing NT-proBNP levels can help rule out HF, as patients are unlikely to have HF when NT-proBNP levels are lower than 125 pg/mL.10 The testing of NT-proBNP levels significantly improves the diagnostic accuracy of HF in the primary care setting by 21%, with most of this improvement attributed to the correct ruling out of a diagnosis of HF.27 This is because NT-proBNP is highly accurate in ruling out HF, with a negative predictive value of 94 to 98%.10
In a study including 1538 patients attending the emergency
department with shortness of breath, adding NP level testing to the workup increased the diagnostic accuracy of HF from 74% to 82% and reduced the overall reported clinical uncertainty of the diagnosis by 74%.28 An Australian study including 145 patients attending the emergency department with breathlessness showed that feeding back the results of NP testing to emergency physicians led to a change in the diagnosis in 15% of cases. There was a reduction in the intermediate likelihood of HF from 52% of cases to 23% of cases, leading to an increase in clinical confidence in the diagnosis of HF.29
In summary, NP levels can:
- assist in the diagnosis or exclusion of HF in patients with co-existent COPD
- help rule out HF in patients presenting to the emergency department with dyspnoea not associated with HF
- improve the diagnostic accuracy of HF in patients presenting to the emergency department with dyspnoea
- increase physicians’ confidence in the diagnosis or exclusion of HF in patients presenting to the emergency department with dyspnoea.
As of 1 November 2024, NP (BNP or NT-proBNP) testing is reimbursed by the Australian Medical Benefits Scheme (MBS) ‘for the exclusion of a diagnosis of HF in patients presenting to a non-hospital setting to assist in decision-making regarding the clinical necessity of an echocardiogram, where HF is suspected based on signs and symptoms but diagnosis is uncertain.’ Outside of the emergency setting, this test will be reimbursed once per patient in a 12-month period (MBS item 66829).
How can assessing natriuretic peptide levels add value to diagnosing heart failure compared with echocardiography?
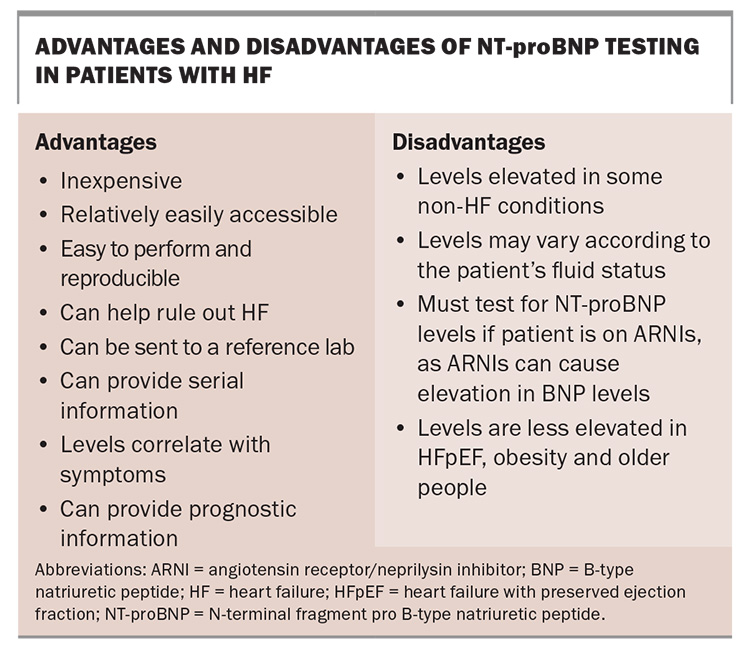
NT-proBNP testing is useful in screening high-risk patients with dyspnoea to exclude HF, with a high sensitivity and negative predictive value in avoiding misdiagnosis in primary care with a cut-off of 125 pg/mL.30 NP testing can reduce unnecessary referrals for echocardiograms and, therefore, improve resource utilisation.31 NT-proBNP testing may also have a cost benefit of ruling out HF in primary care by pre-screening based on NT-proBNP levels and QRS width.32 NP levels can be used to monitor a patient’s response to therapy and guide treatment, especially if there is uncertainty in whether a patient is overloaded; however, routine NP monitoring is not an MBS-reimbursed indication in Australia.33 The advantages and disadvantages of NT-proBNP testing are summarised in the Box.
NT-proBNP testing may reduce the number of tests needed to diagnose HF in the emergency department and was reported to lead to a 34% reduction in chest x-rays performed, 17% reduction in pulmonary function tests conducted and 10% reduction in the need for ECGs.34 There was also a reported 40% reduction in the amount of time spent in the emergency department and a 15% reduction in the costs of emergency department visits, hospitalisations and outpatient services in the subsequent 60 days compared with usual care.35
Echocardiography provides multiple pieces of information, helping to differentiate between HFrEF and HFpEF, confirm or exclude other diagnoses and provide information on cardiac valvular function and pulmonary hypertension. The potential disadvantages of echocardiography include the need for trained technicians, expensive equipment and maintenance; interobserver variability; and the fact that the findings do not always correlate with symptoms and survival in some cases of HF.36
The landmark STRONG-HF study randomised patients hospitalised with acute decompensated HF to usual care or to the initiation of a low-dose regimen of an ACE inhibitor/ARB/ARNI, plus a beta-blocker and a mineralocorticoid receptor antagonist, followed by once-weekly outpatient visits for six weeks. At each visit, the NT-proBNP level was measured and used to guide uptitration of therapy. After six months, there was a 34% reduction in all-cause mortality or HF readmission in patients who received initial NT-proBNP-guided therapy.37 NT-proBNP monitoring guided the incremental increase in prognostically beneficial medications which led to a significant improvement in patient outcomes.
What do guidelines say about natriuretic peptide testing?
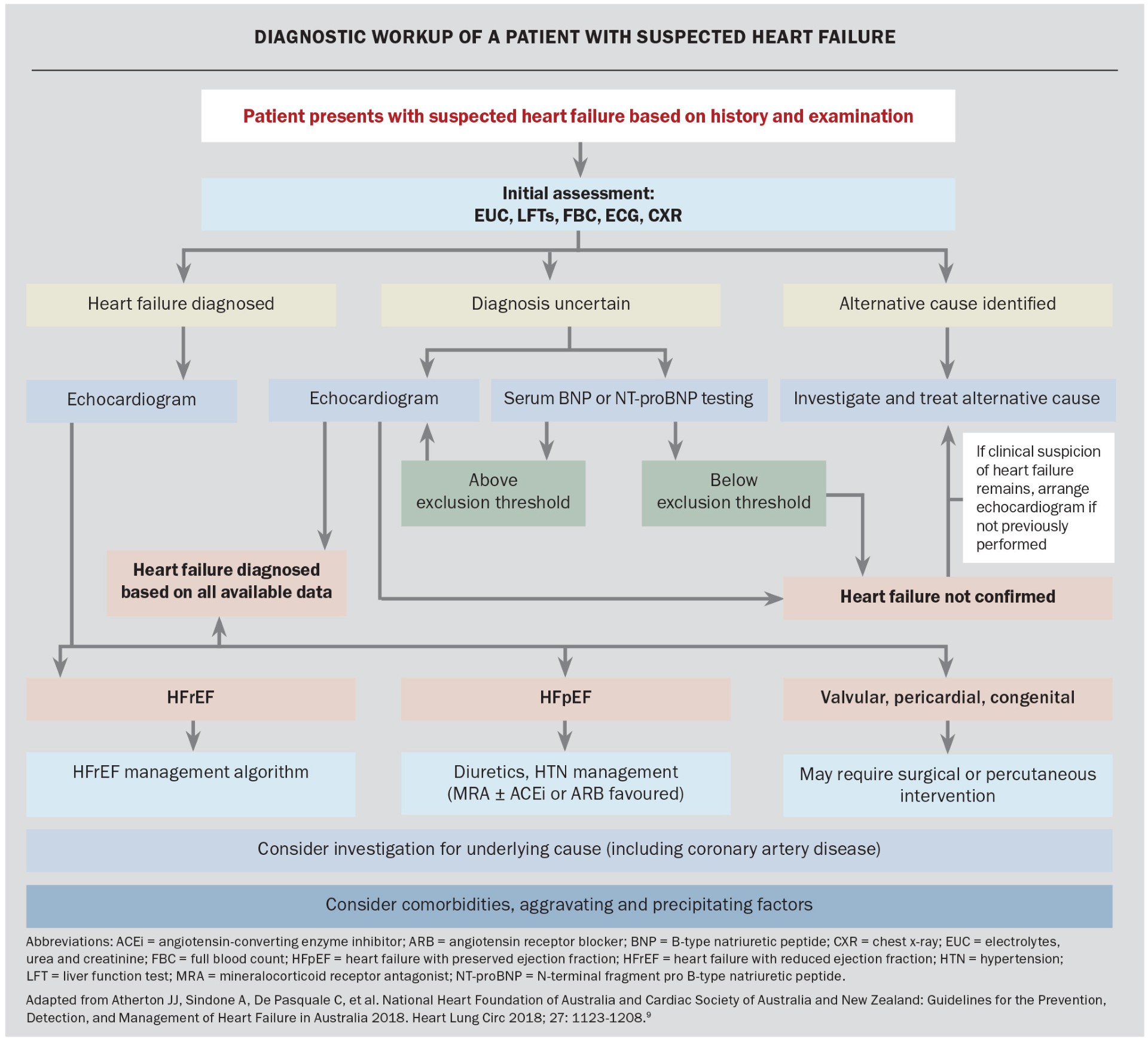
The inclusion of NT-proBNP testing in the diagnostic workup of HF has been incorporated in local and international guideline recommendations. The 2018 National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand Guidelines for the Prevention, Detection, and Management of Heart Failure in Australia recommend the use of NT-proBNP testing for diagnosis in patients with suspected HF when the diagnosis is uncertain.9 The diagnostic approach to a patient with suspected heart failure is presented in the Flowchart.9
Internationally, the European Society of Cardiology 2023 Focused Update of the 2021 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure recommends the measurement of NT-proBNP levels in suspected cases of HF with a class 1B recommendation.38 This update incorporated both HFpEF and HFrEF, whereas assessing NT-proBNP levels has been recommended for the diagnosis of HFpEF since 2019.39
The use of NT-proBNP testing has also been incorporated into The COPD-X Plan: Australian and New Zealand Guidelines for the Management of Chronic Obstructive Pulmonary Disease 2024. These guidelines suggest that NT-proBNP testing can assist in identifying HF in the setting of acute breathlessness, with the caveat that elevated NT-proBNP levels do not exclude comorbid COPD.25
The Asian Pacific Consensus Statement on the Diagnosis and Management of Heart Failure includes several helpful recommendations on the use of NT-proBNP testing:
- baseline NT-proBNP levels should be measured as soon as possible, at least in the first 24 hours of hospitalisation for patients with acute HF
- NT-proBNP levels should be measured during hospitalisation when necessary
- the higher the NT-proBNP level, the poorer the prognosis
- changes in NT-proBNP levels provide useful information for determining the optimal treatment at discharge
- the level of NT-proBNP and reduction in NT-proBNP should not be used as the only criteria to determine the admission and discharge of patients
- NT-proBNP testing provides additional information for clinical evaluation to support clinical decisions on admission, triage, discharge and optimising treatment.33
Conclusion
NT-proBNP testing is an important tool assisting clinicians in the diagnosis and exclusion of HF. It is a reliable, readily accessible biochemical marker with a high negative predictive value, which can reduce the need for echocardiography in diagnosing HF while simultaneously assisting clinicians in confirming other causes of dyspnoea via the exclusion of HF. NT-proBNP testing has been incorporated into multiple guidelines worldwide, and patients with suspected HF could consider this test as part of their diagnostic workup, both in hospital and outpatient settings. MT
COMPETING INTERESTS: Dr J. A. Sindone: None. Professor A. P. Sindone has received honoraria, speaker fees, consultancy fees or travel support, and is a member of advisory boards or has appeared on expert panels for: Abbott, Alphapharm, Amgen, Astra Zeneca, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, CSL, Edwards, Eli Lilly, Glaxo Smith Kline, HealthEd, Inside Practice, Menarini, Merck Sharp and Dohme, Moderna, Mylan, Novartis, Novo Nordisk, Orion, Otsuka, Pfizer, Pharmacosmos, Roche, Sanofi, Servier and Vifor. He also has leadership or fiduciary roles in the Cardiac Society of Australia and New Zealand, National Heart Foundation of Australia, An Asia Pacific Society of Cardiology, NSW Agency for Clinical Innovation and National Cardiac Australia; and holds stock or stock options in National Cardiac Australia.
References
1. Sindone AP, Haikerwal D, Audehm RG, et al. Clinical characteristics of people with heart failure in Australian general practice: results from a retrospective cohort study. ESC Heart Fail 2021; 8: 4497-4505.
2. Chen L, Booley S, Keates AK, Stewart S. Snapshot of heart failure in Australia. Melbourne: Mary MacKillop Institute for Health Research, Australian Catholic University; 2017. Available online at: https://www.acu.edu.au/about/acu/news/2017/june/snapshot-of-heart-failure-in-australia (accessed November 2024).
3. Stewart S, MacIntyre K, Hole DJ, Capewell S, McMurray JJV. More ‘malignant’ than cancer? Five-year survival following a first admission for heart failure. Eur J Heart Fail 2001; 3: 315-322.
4. Ho KK, Anderson KM, Kannel WB, Grossman W, Levy D. Survival after the onset of congestive heart failure in Framingham heart study subjects. Circulation 1993; 88: 107-115.
5. Atherton JJ, Hayward CS, Ahmad WAW, et al. Patient characteristics from a regional multicenter database of acute decompensated heart failure in Asia Pacific (ADHERE International–Asia Pacific). J Cardiac Fail 2012: 18; 82-88.
6. Lahoz R, Fagan A, McSharry M, et al. Recurrent heart failure hospitalizations are associated with increased cardiovascular mortality in patients with heart failure in Clinical Practice Research Datalink. ESC Heart Fail 2020; 7: 1688-1699.
7. Stewart AL, Greenfield S, Hays RD, et al. Functional status and well-being of patients with chronic conditions. Results from the Medical Outcomes Study. JAMA 1989; 262: 907-913.
8. Calvert MJ, Freemantle N, Cleland JGF. The impact of chronic heart failure on health-related quality of life data acquired in the baseline phase of the CARE-HF study. Eur J Heart Fail 2005; 7: 243-251.
9. Atherton JJ, Sindone A, De Pasquale C, et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: guidelines for the prevention, detection, and management of heart Failure in Australia 2018. Heart Lung Circ 2018; 27: 1123-1208.
10. McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2022; 24: 4-131.
11. De Pasquale CG, Audehm R. Diagnosis of heart failure. Medicine Today 2019; 20: 11-16.
12. Audehm RG, Neville AM, Piazza P, et al. Healthcare services use by patients with heart failure in Australia: findings from the SHAPE study. Aust J Gen Pract 2022; 51: 713-720.
13. Pan Y, Li D, Ma J, Shan L, Wei M. NT-proBNP test with improved accuracy for the diagnosis of chronic heart failure. Medicine (Baltimore) 2017; 96: e9181.
14. Tsutsui H, Albert NM, Coats AJS, et al. Natriuretic peptides: role in the diagnosis and management of heart failure: a scientific statement from the heart failure association of the European Society of Cardiology, Heart Failure Society of America and Japanese Heart Failure Society. J Card Fail 2023; 29: 787-804.
15. Bayés-Genís A. The circulating NTproBNP level, a new biomarker for the diagnosis of heart failure in patients with acute shortness of breath. Rev Esp Cardiol 2005; 58: 1142-1144.
16. Mohammed AA, Januzzi JL Jr. Natriuretic peptides in the diagnosis and management of acute heart failure. Heart Fail Clin 2009; 5: 489-500.
17. Davis M, Espiner E, Richards G, et al. Plasma brain natriuretic peptide in assessment of acute dyspnoea. Lancet 1994; 343: 440-444.
18. Maisel AS, Koon J, Krishnaswamy P, et al. Utility of b-natriuretic peptide as a rapid, point-of-care test for screening patients undergoing echocardiography to determine left ventricular dysfunction. Am Heart J 2001; 141: 367-374.
19. Dao Q, Krishnaswamy P, Kazanegra R, et al. Utility of B-type natriuretic peptide in the diagnosis of congestive heart failure in an urgent-care setting. J Am Coll Cardiol 2001; 37: 379-385.
20. Mundy BJ, McCord J, Nowak RM, et al. B-type natriuretic peptide levels are inversely related to body mass index in patients with heart failure [Abstract]. JACC 2003; 41 (6 Suppl 1): 158A.
21. Anand IS, Fisher LD, Chiang Y-T, et al. Changes in brain natriuretic peptide and norepinephrine over time and mortality and morbidity in the Valsartan Heart Failure Trial (Val-HeFT). Circulation 2003; 107: 1278-1283.
22. Salah K, Kok WE, Eurlings LW, et al. A novel discharge risk model for patients hospitalised for acute decompensated heart failure incorporating N-terminal pro-B-type natriuretic peptide levels: a European coLlaboration on Acute decompeNsated Heart Failure: ÉLAN-HF Score. Heart 2014; 100: 115-125.
23. Bettencourt P, Azevedo A, Pimenta J, et al. N-terminal–pro-brain natriuretic peptide predicts outcome after hospital discharge in heart failure patients. Circulation 2004; 110: 2168-2174.
24. Zile MR, Claggett BL, Prescott MF, et al. Prognostic implications of changes in N-terminal pro-B-type natriuretic peptide in patients with heart failure. JACC 2016; 68: 2425-2436.
25. Lung Foundation Australia. The COPD-X plan: Australian and New Zealand guidelines for the management of COPD. Milton: Lung Foundation Australia; 2024. Available online at: https://lungfoundation.com.au/resources/the-copd-x-plan-australian-and-new-zealand-guidelines-for-the-management-of-copd/ (accessed November 2024).
26. Leong P, MacDonald MI, King PT, et al. Treatable cardiac disease in hospitalised COPD exacerbations. ERJ Open Res. 2021; 7: 00756-2020.
27. Wright SP, Doughty RN, Pearl A, et al. Plasma amino-terminal pro-brain natriuretic peptide and accuracy of heart-failure diagnosis in primary care: a randomized, controlled trial. J Am Coll Cardiol 2003; 42: 1793-1800.
28. Maisel A, Krishnaswamy P, Nowk R, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. New Engl J Med 2022; 347: 161-167.
29. Chung T, Sindone A, Foo F, et al. Influence of history of heart failure on diagnostic performance and utility of B-type natriuretic peptide testing for acute dyspnea in the emergency department. Am Heart J 2006; 152: 949-955.
30. Huelsmann M, Neuhold S, Strunk G, et al. NT-proBNP has a high negative predictive value to rule-out short-term cardiovascular events in patients with diabetes mellitus. Eur Heart J 2008; 29: 2259-2264.
31. Taylor CJ, Roalfe AK, Iles R, et al. Primary care REFerral for EchocaRdiogram (REFER) in heart failure: a diagnostic accuracy study. Br J Gen Pract 2017; 67: e94-e102.
32. Goode KM, Clark AL, Cleland JGF. Ruling out heart failure in primary-care: the cost-benefit of pre-screening using NT-proBNP and QRS width. Int J Cardiol 2008; 130: 426-437.
33. Sim D, Lin W, Sindone A, et al. Asian Pacific Society of Cardiology Consensus Statements on the diagnosis and management of chronic heart failure. J Asian Pacific Soc Cardiol 2023; 2: e10.
34. Behnes MM, Brueckmann M, Ahmad-Nejad P, et al. Diagnostic performance and cost effectiveness of measurements of plasma N-terminal pro brain natriuretic peptide in patients presenting with acute dyspnea or peripheral edema. Int J Cardiol 2009; 135: 165-174.
35. Moe GW, Howlett J, Januzzi JL, Zowall H; Canadian Multicenter Improved Management of Patients With Congestive Heart Failure (IMPROVE-CHF) Study Investigators. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation 2007; 115: 3103-3110.
36. Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2016; 29: 277-314.
37. Mebazaa A, Davison B, Chioncel O, et al. Safety, tolerability and efficacy of up-titration of guideline-directed medical therapies for acute heart failure (STRONG-HF): a multinational, open-label, randomised, trial. Lancet 2022; 400: 1938-1952.
38. McDonagh TA, Metra M, Adamo M, et al. 2023 focused update of the 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2023; 44: 3627-3639.
39. Pieske B, Tschöpe C, de Boer RA, et al. How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur Heart J 2019; 40: 3297-3317.