Takotsubo cardiomyopathy: how can you mend a broken heart?
Takotsubo cardiomyopathy, or stress-induced cardiomyopathy, occurs more commonly than recognised. It is important to consider this condition as a differential diagnosis for acute chest pain or dyspnoea, as it often presents like acute coronary syndrome and can have life-threatening complications.
- Takotsubo cardiomyopathy (TCM) is an increasingly recognised differential diagnosis of acute cardiac presentations.
- Patients with TCM present with symptoms mimicking acute coronary syndrome or heart failure with acute chest pain, dyspnoea, associated ECG changes and raised troponin levels triggered by acute physical or emotional stressors.
- The diagnosis of TCM is based on hallmark findings of left ventricular apical ballooning, with no corresponding obstructive coronary artery disease on coronary angiography.
- TCM can cause serious complications including heart failure, shock, left ventricular thrombus, stroke, ventricular arrhythmia, rupture or death.
- Treatment is supportive with diuretics and heart failure medications including ACE inhibitors and beta blockers.
- In almost all cases, left ventricular dysfunction resolves after weeks to months of follow up, but some patients may have residual chest pain, dyspnoea or dizziness.
- Uncomplicated cases of TCM are often referred back to the patient’s GP for follow up.
Takotsubo cardiomyopathy (TCM), also known as stress-induced cardiomyopathy, apical ballooning syndrome or ‘broken heart’ syndrome, is a condition characterised by the acute onset of transient segmental left ventricular dysfunction, almost always triggered by acute physical or emotional stressors. The hallmark apical ballooning with hypercontractile basal left ventricular segments is reminiscent of the design of the traditional Japanese octopus trap, the tako-tsubo pot, hence the descriptive term ‘Takotsubo’ cardiomyopathy. Although the condition was initially considered rare, TCM accounts for 1 to 2% of admissions for acute coronary syndrome and, therefore, should be considered as a differential diagnosis.1 This article provides an overview of TCM to help GPs recognise and manage this condition.
Clinical presentation
The most common presentation of TCM in general practice or emergency is acute chest pain and dyspnoea following a stressful event. These symptoms are associated with ST segment changes on 12-lead ECG, consistent with acute coronary syndrome. Alternatively, patients with concurrent acute medical illness may present without symptoms but with typical ECG changes or elevations in cardiac biomarkers or new-onset decompensated heart failure.2 Further cardiac testing is required for suspected TCM.
The condition affects women, particularly postmenopausal women, more than men, and underlying mental health illness is also a predisposing factor.3 The presence of emotional or physical stressors in the preceding one to five day(s) is often identified in two-thirds of patients with TCM, although the absence of a stressor does not exclude its diagnosis. Emotional triggers include recent deaths, financial losses, domestic arguments and situations of extreme fear, including anticipated fear of medical procedures. Some physical triggers include the postsurgical period, pain, haemorrhage, sepsis and respiratory failure.
Findings of physical examination are usually unremarkable or, if abnormal, are signs of heart failure. Diagnosis is often only made after coronary imaging and echocardiography.
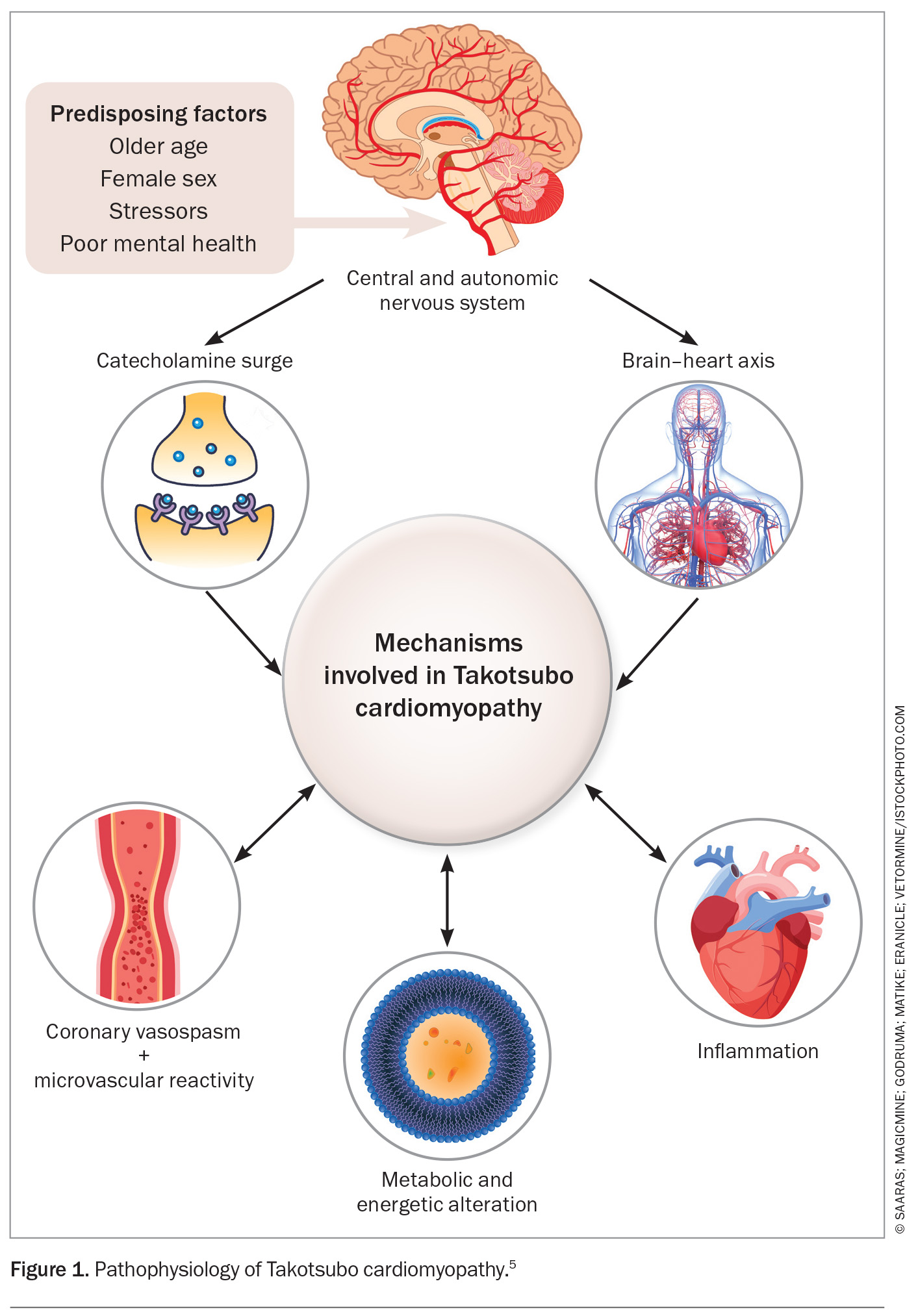
Pathophysiology
The precise pathophysiology of TCM is not fully understood but several key mechanisms are thought to contribute to the development of transient and acute left ventricular dysfunction (Figure 1).4,5
Diagnosis
The diagnosis of TCM is made only after the exclusion of significant obstructive coronary artery disease, together with characteristic wall motion abnormalities of the left ventricle. The Mayo Clinic developed diagnostic criteria in 2004 to assist with the diagnosis. These have since been revised and include:
- transient wall motion abnormalities in the left ventricular midsegments, with or without apical involvement, that extend beyond a single epicardial vascular distribution. There is often, but not always, a stressful trigger
- absence of obstructive coronary artery disease or acute plaque rupture
- new ECG abnormalities (ST segment elevation and/or T-wave inversion)
- modest elevation in cardiac troponin level
- absence of phaeochromocytoma and myocarditis.6
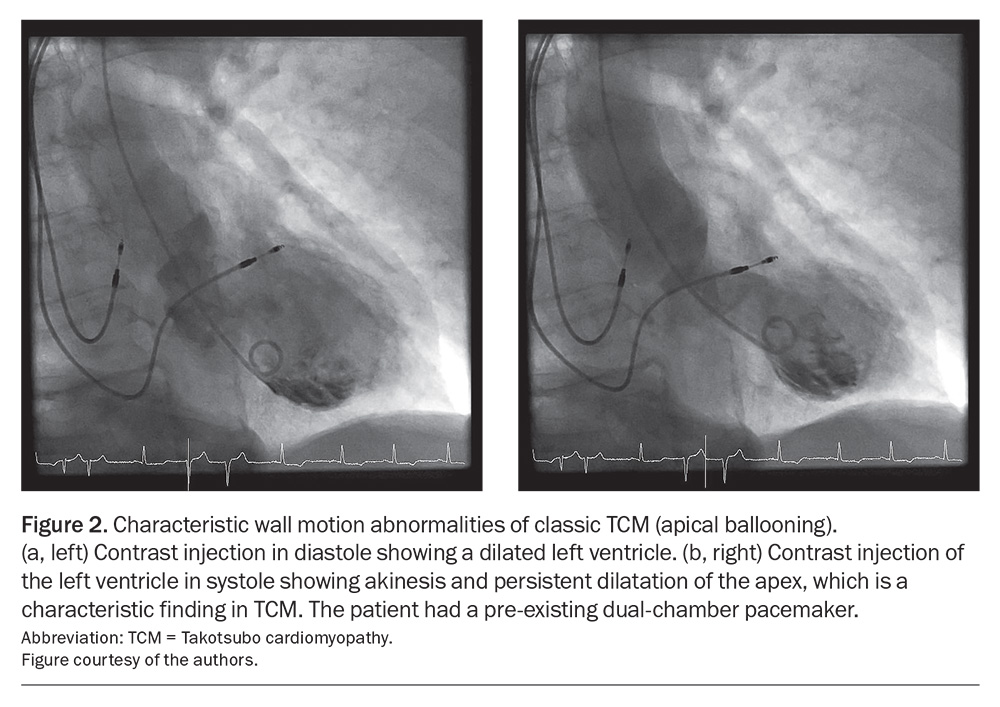
There are multiple well-described variants of TCM in the literature that refer to differing patterns of abnormal left ventricular wall motion. The ‘classic’ form of apical ballooning describes severely hypokinetic apical segments with sparing of the basal segments (Figure 2a and b). ‘Reverse’ or basal TCM is the opposite, with hypokinetic basal segments with preserved mid- to apical contraction. Midventricular TCM presents with severe hypokinesis of all midcavity segments with preservation of basal and apical contraction. Finally, the rarest form is ‘focal’ TCM, in which one myocardial segment is affected.
Investigations
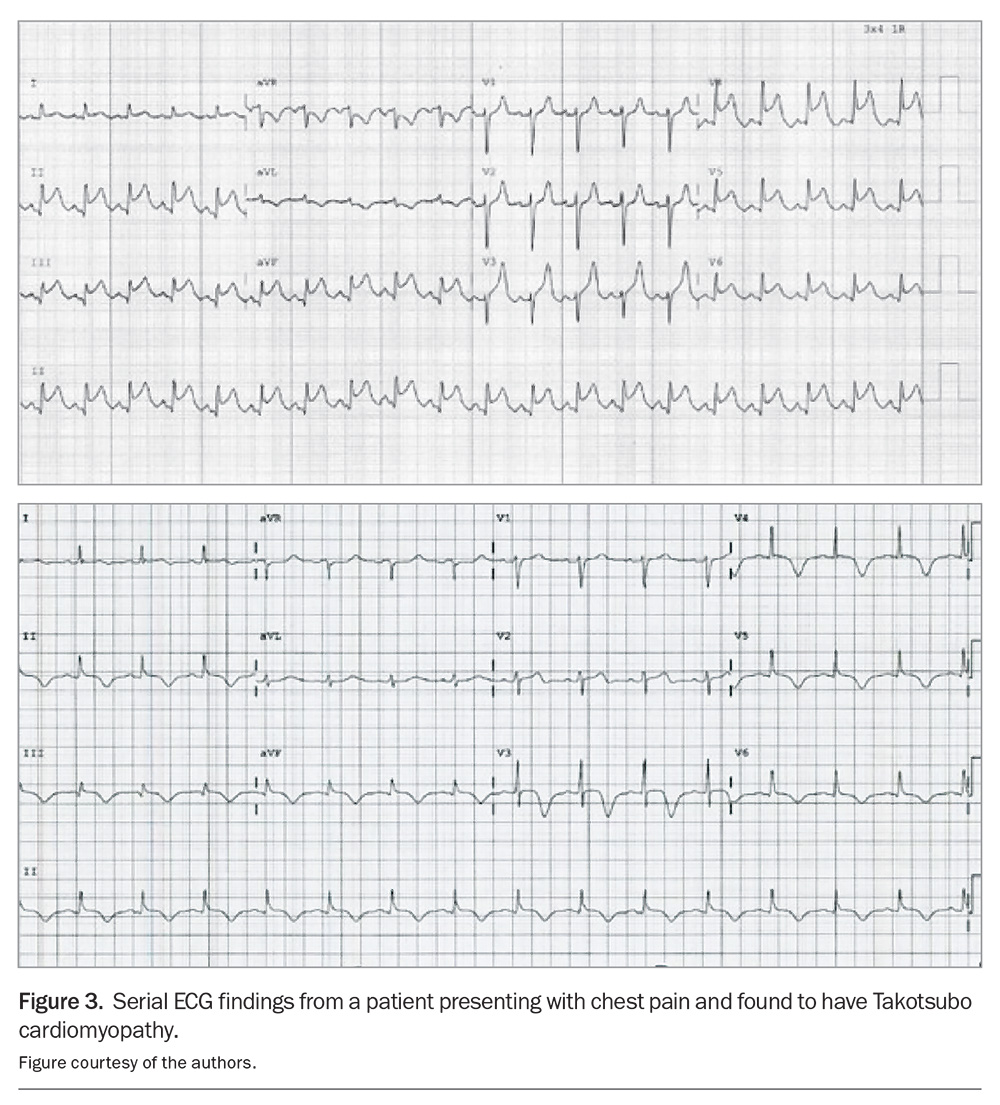
12-lead ECG
There are often characteristic ECG changes associated with the progression of TCM. In the hyperacute stage, ST segment elevations are often indistinguishable from ST elevation myocardial infarction (STEMI) and will tend to affect precordial leads.7
Figure 3 illustrates an example of a patient presenting with chest pain who was subsequently diagnosed with TCM. These ECG findings show the typical evolution of TCM over days, starting with ST elevation (mimicking STEMI) and followed by global deep T-wave inversions and QT prolongation, which may predispose the patient to ventricular arrhythmias. These changes will usually resolve after a few weeks.
Cardiac biomarkers
Troponin levels are elevated in patients with TCM because of myocardial injury but to a lesser degree compared with levels in those with STEMI or non-ST elevation myocardial infarction (NSTEMI). Levels of N-terminal pro b-type natriuretic peptide (NT-proBNP), a marker of ventricular stretching, are usually significantly elevated and disproportionate to elevations in serum levels of troponin T. Hence, an elevated NT-proBNP to troponin T ratio greater than 10 may suggest TCM over other differential diagnoses. Creatine kinase levels are not usually significantly elevated in TCM.
Invasive coronary angiography
A diagnosis of TCM can only be made after the exclusion of coronary artery disease, as the classic appearance of apical ballooning can represent an apical infarct from a large occluded left anterior descending artery. Left ventriculography at the time of angiography can also help identify the characteristic apical ballooning.8 The unique association of normal coronary arteries on angiography and extensive apical ballooning is diagnostic of TCM.
The decision to perform coronary angiography must take into account standard procedural risks, including significant bleeding, stroke, myocardial infarction, renal dysfunction and death.
CT coronary angiography
CT coronary angiography, when readily available, is increasingly utilised as an alternative to invasive coronary angiography when the likelihood of significant coronary artery disease is low and the probability of TCM is high. In this context, CT coronary angiography has a negative predictive value of 97% when used to exclude significant coronary artery disease.
Echocardiography
Echocardiography allows for easy visualisation of the typical apical-midventricular ballooning pattern, allows for the assessment of left ventricular function and is critical for the evaluation of complications such as left ventricular outflow obstruction, mitral regurgitation, ventricular rupture and pericardial effusion.9 Contrast echocardiography with perflutren-containing lipid contrast is essential to exclude left ventricular apical thrombus as the sequelae of stroke is often devastating. Serial echocardiography once the patient has been discharged is a key aspect in documenting the recovery of left ventricular function on follow up.
Cardiac magnetic resonance imaging
Cardiac MRI is becoming widely used for the diagnosis of TCM as it can help differentiate between TCM, acute myocardial infarction and myocarditis – the most common differential diagnoses. In the acute phase of disease, the distribution of myocardial oedema can help differentiate TCM from myocarditis. Late-gadolinium contrast enhancement to detect scarring is useful to differentiate TCM from myocardial infarction, especially in patients with coronary artery disease. Structural complications and thrombus are also identified on cardiac MRI.
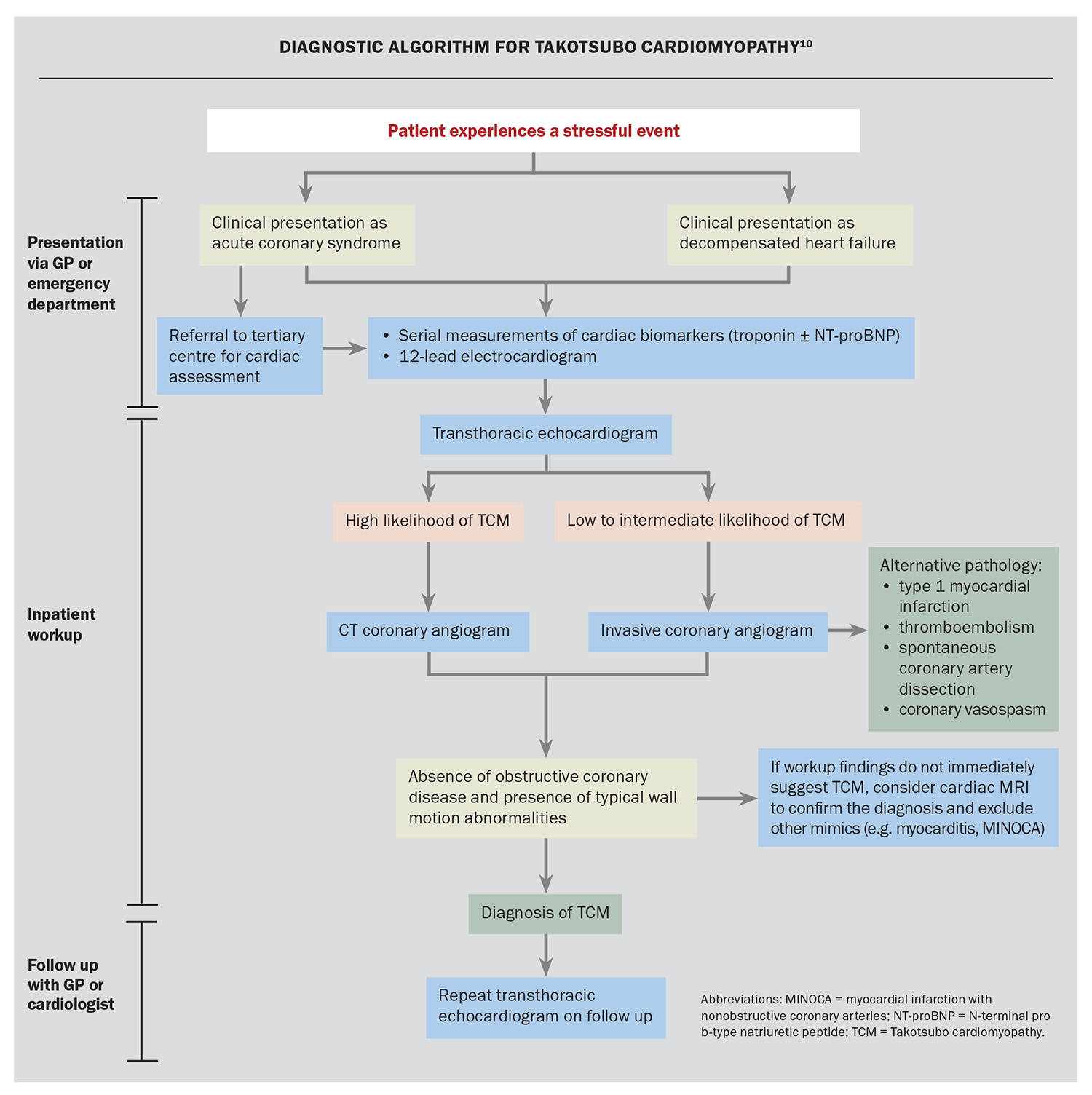
A suggested diagnostic approach is outlined in the Flowchart.10
Complications
Complications of TCM may include ventricular arrhythmia, left ventricular thrombus formation, left ventricular free wall rupture and cardiogenic shock. In rare cases, TCM can lead to cardiac arrest. However, the prognosis of TCM is generally good, with most people fully recovering even without treatment. The overall rates of complication are unknown; however, it is suggested that in-hospital mortality rates may be as high as 5%.11
Management
There is no specific treatment for TCM and, therefore, management involves a combination of supportive care, monitoring and pharmacotherapy. In general, associated left ventricular dysfunction resolves over a period of weeks to months; however, care must be taken to treat complications in the acute phase as a patient’s condition can range from mildly symptomatic to severe shock requiring intensive care unit admission.
Supportive care
In cases of left ventricular failure, diuretics are prescribed to treat pulmonary oedema until recovery of left ventricular function occurs, usually within days. Furosemide is the mainstay of treatment for this period, and oxygen and occasionally, continuous positive airway pressure therapy is required for additional respiratory support.
Cardiogenic shock is seen in about 5 to 10% of patients. Factors associated with the development of shock include younger age, lower left ventricular ejection fraction and a physical trigger. Appropriate management of shock varies depending on the presence of significant left ventricular outflow tract obstruction and resultant mitral regurgitation, which can occur because of the compensatory basal hypercontractility in response to severe mid- to apical hypokinesis of the left ventricle.12
Patients with cardiogenic shock without left ventricular outflow tract obstruction sometimes require admission to the intensive care unit for more advanced haemodynamic support with combinations of intravenous dobutamine (which is TGA approved but not PBS listed), noradrenaline infusions and invasive arterial blood pressure monitoring. In the presence of obstruction, the treatment of shock is paradoxical, in that it is important to avoid hypovolaemia and the use of vasodilators, with cautious administration of beta blockers.
Cardiac monitoring
Patients with TCM usually undergo routine cardiac monitoring for 24 hours because of the theoretical risk of ventricular arrhythmia, although this has been rarely reported in the literature. Patients with significant QT prolongation (i.e. described up to 600 to 800 ms) should continue to undergo cardiac monitoring for at least 48 hours or until the QT interval returns significantly to baseline because of the risk of Torsades de Pointes and polymorphic ventricular tachycardia. Care must be taken to avoid bradycardia, particularly with the prescription of beta blockers, as this can exacerbate QT prolongation.
Pharmacotherapy
Heart failure medications are prescribed for patients with TCM with significant left ventricular dysfunction, although there are no large randomised controlled trials to support their use. Beta blockers and renin-angiotensin system inhibitors are the most prescribed treatments, at least until complete recovery of left ventricular function.13 The duration or safety in deprescribing these treatments is not known. Cardioselective beta blockers, such as bisoprolol, carvedilol, nebivolol and extended-release metoprolol, in theory, should counteract the impact of the catecholamine surge implicated in the pathogenesis of TCM. Furosemide is the most common diuretic used to manage the symptoms of pulmonary oedema in the acute phase and may need to be continued until the recovery of left ventricular function. Mineralocorticoid receptor antagonists (e.g. spironolactone) may be added if required. Currently, there are no data regarding the use of SGLT-2 inhibitors in TCM.
Left ventricular apical thrombus has been described in patients with TCM, which can result in systemic embolism and stroke. The treatment for thrombus is oral therapeutic anticoagulation, with the most evidence shown with warfarin for stroke prevention in this context. However, there are some small observational data to suggest that the antithrombotic agent rivaroxaban can be considered an alternative.14 The duration of treatment is usually three months or until resolution of the thrombus on serial echocardiography or cardiac MRI.
Follow up and prognosis
Patients with TCM are routinely followed up by cardiologists, to ensure normalisation of left ventricular function and management of any complications. This involves performing echocardiography four to six weeks after the acute event.
It has been reported that one in eight patients may develop recurrent episodes of TCM. Currently, there are no specific features associated with the risk of recurrence. The avoidance of stress, in conjunction with long-term heart failure therapy should be considered.
It was traditionally thought that patients with TCM recover completely. However, newer data suggest that the longer-term prognosis of patients with TCM is similar to that in patients with STEMI or NSTEMI. Despite resolution of left ventricular dysfunction, patients can experience residual chest pains, dyspnoea, lethargy or palpitations for up to two years after the acute event. The reasons and mechanisms for this are not known.15
In patients with recovered TCM without any complications, it is appropriate for them to be followed up by their GP, as they no longer require surveillance imaging.
Conclusion
TCM is a syndrome characterised by transient acute left ventricular dysfunction triggered by emotional, physical or medical stressors. The evaluation is complex and requires close consultation with a cardiologist in the inpatient setting. Investigation includes the measurement of cardiac biomarkers and advanced cardiac imaging techniques, such as angiography, echocardiography and cardiac MRI. The treatment of TCM is supportive, but specific management is directed towards specific complications should they arise. Left ventricular function almost always returns to normal after a period of weeks to months, but some patients may experience symptoms after resolution of the acute episode. Recurrences of TCM are rare but possible. MT
COMPETING INTERESTS: Dr Hii: None. Dr Chan has received support for attending meetings from Novartis and AstraZeneca; is a Member of the South Australian Advisory Board for the National Heart Foundation of Australia; and is the South Australia Elected Board Member for the Cardiac Society of Australia and New Zealand.
References
1. Redfors B, Jha S, Thorleifsson S, et al. Short- and long-term clinical outcomes for patients with takotsubo syndrome and patients with myocardial infarction: a report from the Swedish Coronary Angiography and Angioplasty Registry. J Am Heart Assoc 2021; 10: e017290.
2. Assad J, Femia G, Pender P, Badie T, Rajaratnam R. Takotsubo syndrome: a review of presentation, diagnosis and management. Clin Med Insights Cardiol 2022; 16: 11795468211065782.
3. Compare A, Bigi R, Orrego P, Proietti R, Grossi E, Steptoe A. Type D personality is associated with the development of stress cardiomyopathy following emotional triggers. Ann Behav Med 2013; 45: 299-307.
4. Pelliccia F, Kaski J, Crea F, Camici P. Pathophysiology of Takotsubo syndrome. Circulation 2017; 135: 2426-2441.
5. Singh T, Khan H, Gamble D, Scally C, Newby D, Dawson D. Takotsubo syndrome: pathophysiology, emerging concepts, and clinical implications. Circulation 2022; 145: 1002-1019.
6. Akashi Y, Goldstein D, Barbarao G, Ueyama T. Takotsubo cardiomyopathy: a new form of acute reversible heart failure. Circulation 2008; 118: 2754-2762.
7. Namgung J. Electrocardiographic findings in takotsubo cardiomyopathy: ECG evolution and its difference from the ECG of acute coronary syndrome. Clin Med Insights Cardiol 2014; 8: 29-34.
8. Ghadri J-R, Wittstein I, Prasad A, et al. International expert consensus document on Takotsubo syndrome (part I): clinical characteristics, diagnostic criteria, and pathophysiology. Eur Heart J 2018; 39: 2032-2046.
9. Templin C, Collste O, Ehreborg E,Jambert-Petterson H. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med 2015; 373: 929-938.
10. Agewall S, Beltrame J, Reynolds H, et al. ESC working group position paper on myocardial infarction with non-obstructive coronary arteries. Eur Heart J 2017; 38: 143-153.
11. Brinijikji W, El-Sayed A, Salka S. In-hospital mortality among patients with takotsubo cardiomyopathy: a study of the National Inpatient Sample 2008 to 2009. Am Heart J 2012; 164: 215-221.
12. Muratsu A, Muroya T, Kuwugata Y. Takotsubo cardiomyopathy in the intensive care unit. Acute Med Surg 2019; 6: 152-157.
13. Ong GJ, Nguyen T, Stansborough J, et al. The N-AcetylCysteine and RAMipril in Takotsubo Syndrome Trial (NACRAM): rationale and design of a randomised controlled trial of sequential N-Acetylcysteine and ramipril for the management of Takotsubo syndrome. Contemp Clin Trials 2019; 90: 105894.
14. Albabtain M, Alhebaishi Y, Al-Yafi O, et al. Rivaroxaban versus warfarin for the management of left ventricle thrombus. Egypt Heart J 2021; 73: 41.
15. Ghadri J, Kato K, Cammann V, et al. Long-term prognosis of patients with Takotsubo syndrome. J Am Coll Cardiol 2018; 72: 874-882.
16. Boyd B, Solh T. Takotsubo cardiomyopathy: review of broken heart syndrome. JAAPA 2020; 33: 24-29.