A new low-dose levonorgestrel intrauterine contraceptive
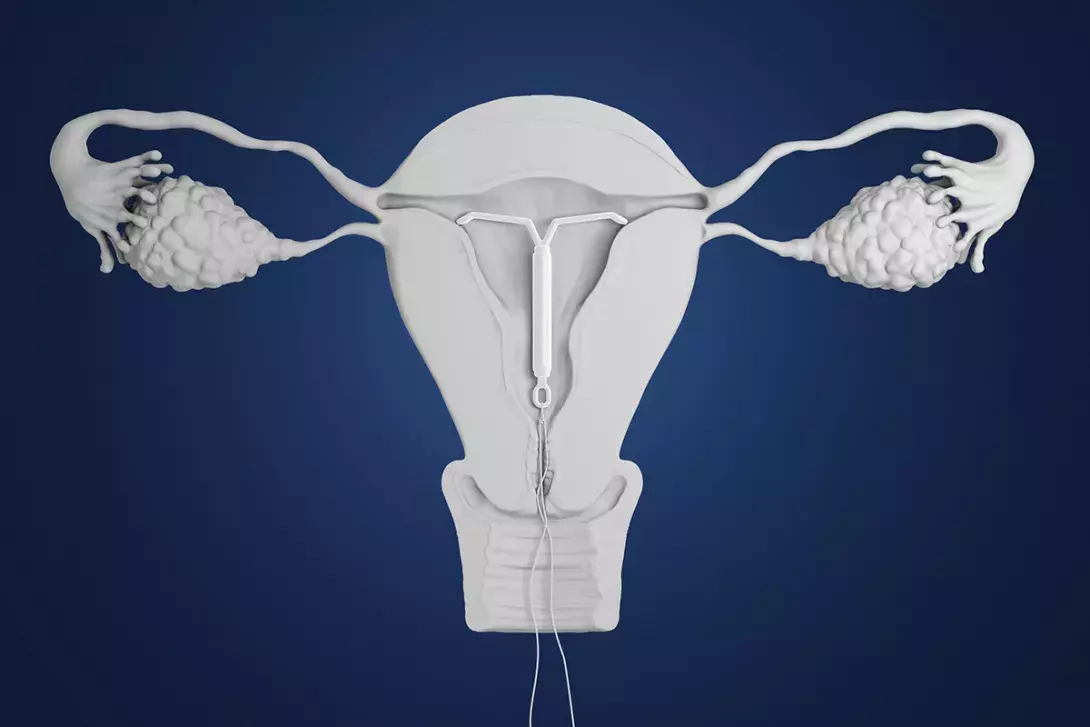
Long-acting reversible contraceptives (LARCs) provide high-efficacy, cost-effective contraception suitable for most women across the reproductive life course. The PBS-listed 19.5 mg levonorgestrel intrauterine device (IUD) is a highly effective LARC option with a lower hormonal dose and smaller frame size than the 52 mg levonorgestrel IUD.
Long-acting reversible contraceptives (LARCs) are universally recognised as providing high-efficacy, cost-effective contraception that can be a used by most patients across the reproductive life course.1,2 The most recent published nationally representative data from 2012-13 found that about 6% of women in Australia using contraception were using an intrauterine device (IUD); although this figure is likely to have increased, uptake still appears relatively low compared with other high-income countries.3,4 The introduction of a new PBS-listed IUD on 1 March 2020 that has a smaller frame and lower levonorgestrel (LNG) dose than the 52 mg LNG IUD (Mirena) offers an additional LARC choice. The availability of the 19.5 mg LNG IUD (Kyleena) is likely to enhance overall awareness and uptake of LARCs across Australia and to contribute to a reduction in unintended pregnancies and abortions.
What is the new medication?
The new LNG IUD contains 19.5 mg of LNG in its stem, which is released at an average daily rate of 9 mcg/24 hours over five years following an initial release rate of 17.5 mcg/24 hours.5 The systemic LNG exposure after 90 days of use is about 140 ng/L, half that of the 52 mg LNG IUD device (see the comparison in Table 1).6 The 19.5 mg LNG IUD has a smaller frame, 28 mm wide by 30 mm high compared with 32 mm by 32 mm for the 52 mg LNG IUD. The 19.5 mg LNG IUD additionally has a silver ring at the neck of the stem, which is visible on imaging and may be helpful in identifying which device is in situ if this is uncertain.5,7
The 19.5 mg LNG IUD is licensed to provide contraception for five years of use. Pearl Index studies show an effectiveness rate of 99.7% over five years of use compared with 99.9% for the 52 mg LNG IUD.8 The main mechanism of action is through toxicity to the gametes to prevent fertilisation, thickening of the mucus at the cervix and thinning of the endometrium. It may prevent ovulation in some cycles, especially in the first year of use.6
How is the medication used?
The insertion procedure is identical for both hormonal IUDs, but the 19.5 mg IUD inserter tube is narrower at 3.8mm compared with 4.4 mm for the 52 mg LNG IUD. A nonblinded clinical trial comparing clinician-rated ease of insertion and client-related insertion pain found a statistically significant difference between the 19.5 mg and 52 mg LNG devices in both domains: insertion was rated as easy by 94% versus 86% of clinicians (p<0.001) for the 19.5 mg compared with the 52 mg LNG device; and insertion pain was rated as either mild or none for 72% versus 58% of women (p<0.001).9 However, this study used a slightly wider insertion tube (4.75 mm) for the 52 mg LNG IUD than the currently used 4.4 mm tube, and the difference between devices may not be applicable to the current insertion tube.
Fear of pain with IUD insertion is a common concern among potential users.10 On average, nulliparous women experience more IUD insertion pain than parous women.11 Whether the 19.5 mg LNG IUD offers an advantage in reduced insertion pain compared with other IUDs in nulliparous people is yet to be determined.
Timing of insertion
Both the 52 mg and the 19.5 mg LNG IUD should be inserted only when the possibility of an existing pregnancy has been excluded. Neither can be used for emergency contraception.
Both the 19.5 mg and 52 mg LNG IUD can be inserted:
- in the first five days of the menstrual cycle if there has been either no unprotected intercourse or use of a reliable method of contraception in the previous three weeks, with a negative urine pregnancy test
- immediately postpartum or from four weeks after delivery (in primary care this is usually delayed until six to eight weeks) when a pregnancy has been excluded
- at the time of a surgical abortion or
- after completion of a medical abortion when a repeat pregnancy has been excluded.
Recommendations on when to insert the 19.5 mg LNG IUD and when it is effective in different situations are detailed in Table 2.12 This includes when switching from other forms of contraception.
Indications and benefits
Although both the 19.5 mg and the 52 mg LNG IUDs are licensed for up to five years of use for contraception, they differ in other attributes. The 19.5 mg LNG IUD is effective in reducing menstrual bleeding and induces endometrial atrophy. However, unlike the 52 mg LNG IUD, it is not licensed for the management of heavy menstrual bleeding nor for providing endometrial protection as part of a menopausal hormone therapy (MHT) regimen. Studies of the 19.5 mg LNG IUD in these specific populations are lacking. The extended off-label use of the 52 mg LNG IUD beyond five years if inserted at age 45 years or above, either until menopause or until it is no longer needed, also does not apply to the 19.5 mg LNG IUD.13 The latter must be removed and replaced at or before five years.
The 52 mg LNG IUD has been shown to be effective in reducing dysmenorrhoea, including dysmenorrhoea associated with endometriosis and adenomyosis.14-16 Although the 19.5 mg LNG IUD has not been studied in these specific populations, in a comparative trial it had a similar effect to the 52 mg LNG IUD in decreasing dysmenorrhoea overall. In users of both IUDs, the number reporting no dysmenorrhoea increased from around 50% to 80% over a three-year period of use.9
Both copper and LNG IUDs appear to have benefits in relation to reproductive cancers. Retrospective studies show an association between IUD use and a reduction in ovarian, cervical and endometrial cancer.17-19 The 52 mg LNG IUD can be used for management of complex atypical endometrial hyperplasia and early-grade endometrial cancer.20 It is unknown whether use of the 19.5 mg LNG IUD will be associated with these benefits.
Who can use it?
The few absolute or strong contraindications to both the 19.5 mg and 52 mg LNG IUD include:
- abnormal vaginal bleeding suggesting a serious cause
- current pelvic infection
- distortion of the uterine cavity
- insertion between 48 hours and four weeks postpartum
- breast cancer
- severe liver disease.
Both devices can be used in people with a past history of stroke or ischaemic heart disease. In those who develop these conditions during use, continuation can be considered on a case-by-case basis, with caution and clear documentation if no other suitable method is available.21
The 19.5 mg LNG IUD can be used by all medically eligible people, including adolescents and nulliparous people as well as those who are postpartum or perimenopausal. The smaller size of the device and lower dose of progestogen may be attractive to some people, including younger people and those who prefer to menstruate, whereas others may prefer the higher dose LNG IUD which has a proven effect on heavy menstrual bleeding and an increased likelihood of amenorrhoea.22
Risks and complications
There is no evidence of a difference in the risk of failed insertion, perforation and insertion-related infection for the 19.5 mg compared with the 52 mg device.9 The cumulative risk of complete or partial expulsion for the 19.5 mg LNG IUD over five years was 3.7%, similar to the 5% rate quoted for all IUDs.23,24
As for all IUDs, asymptomatic people diagnosed and treated for chlamydia or gonorrhoea can retain their 19.5 mg LNG IUD. If pelvic inflammatory disease develops while an IUD is in situ, treatment should be instituted, with a clinical review scheduled in two to three days. If there is clinical improvement the device can be retained, but it should be removed if the condition is not improving or is worsening.21
In the rare case of a pregnancy occurring with an IUD in situ, pregnancy options should be discussed. The device must be removed before a medical abortion or at the time of a surgical abortion if the IUD threads are missing and prior removal has not been possible. If the pregnancy is continuing, provided it is before 12 weeks’ gestation, the device should be removed as soon as possible because of the risk of septic miscarriage or premature delivery if it is left in situ.25 After 12 weeks’ gestation, specialist referral is required.
About 1 to 2% of all pregnancies are ectopic, and the rate of ectopic pregnancies is significantly reduced in IUD users because of their high level of effectiveness in preventing pregnancies overall. However, if an IUD failure occurs the proportion of extrauterine (ectopic) to intrauterine pregnancies is increased. Of the 13 pregnancies that occurred in a study of around 1400 users of the 19.5 mg LNG IUD, eight were ectopic.23 This is not statistically different from the rate of around 50% of pregnancies occurring with a 52 mg LNG IUD in situ.26 People using any LNG IUD should be advised to seek medical help if they have symptoms suggesting pregnancy or a positive home pregnancy test and should be made aware of the symptoms of ectopic pregnancy and when to seek medical help.
Common side effects
Both the 52 mg and 19.5 mg LNG IUDs have an impact on vaginal bleeding patterns owing to the effect of LNG on the endometrium. Irregular bleeding or spotting is relatively common with both devices in the first few months of use, and both are associated with a reduction in the number of bleeding or spotting days over time (Figure).9 The 19.5 mg LNG IUD appears to be associated with a higher mean number of bleeding/spotting days and lower rates of amenorrhoea than the 52 mg LNG IUD.22 However, the significance of this difference to users may be small as discontinuation of the 19.5 mg LNG IUD because of bleeding issues (including amenorrhoea) was only 4.9% at three years, with no difference in discontinuation due to bleeding patterns by age or parity.27,28
Although a difference in other hormonal side effects might be expected, the clinical trial data did not show any significant differences in side effects, including acne, breast discomfort, pelvic pain or weight gain between devices.9
All progestogen-only contraceptive methods can be associated with an increase in benign functional ovarian cysts. The lower hormone dose in the 19.5 mg LNG IUD appears to have a lower risk relative to the 52 mg LNG IUD. Should cysts occur, they are almost always asymptomatic and resolve spontaneously.9
Conclusion
The PBS-listed 19.5 mg LNG IUD offers an additional highly effective LARC option that has a lower hormonal dose and a smaller frame size than the 52 mg LNG IUD. The smaller size of the device may make it easier to insert with less discomfort for the user, and the impact of the lower progestogen dose on the bleeding pattern, with a reduced likelihood of amenorrhoea, may suit some potential users. This new LARC method is suitable for all medically eligible people who have made an informed choice and understand its advantages and disadvantages relative to other options. MT
