Ocular associations of autoimmune disease
Although autoimmune conditions may predominantly affect one organ system, they are systemic diseases and can therefore cause complications in other parts of the body, including the eye.
- Ocular manifestations are not specific to the autoimmune disease and require a high level of clinical suspicion by the GP to recognise.
- Prompt recognition and management of complications may decrease visual morbidity.
- Optic neuritis is the presenting sign of multiple sclerosis in 20% of cases.
- Visual disturbance is the presenting complaint in 25 to 50% of patients with giant cell arteritis.
- Up to 25% of patients with rheumatoid arthritis experience ocular involvement.
- Some medications used in the management of autoimmune disease have ocular side effects and patients require regular screening.
- A collaborative approach between the GP and ophthalmologist in the evaluation and treatment of patients with ocular complications of systemic disease is essential for effective management.
Ocular structures that may be affected in autoimmune disease include the cornea, conjunctiva, sclera, lens, uvea (iris, ciliary body and choroid), optic nerve and retina. A summary of the terminology and definitions of common complications together with signs and symptoms are outlined in Table 1.
Ocular manifestations may be the first presenting sign of autoimmune disease, so prompt recognition of common associations and management of complications may decrease the risk of visual morbidity (Table 2). Aspects of the ophthalmic examination that are useful to assess for ocular complications include:
- visual acuity
- pupil reactions
- ocular motility
- confrontation visual field testing
- external inspection including fluorescein staining and ophthalmoscopy.
Multiple sclerosis
Optic neuritis is the presenting sign of multiple sclerosis in 20% of cases, and 50% of patients with multiple sclerosis will experience an episode of optic neuritis during their lifetime.1
Typical symptoms of ocular involvement in multiple sclerosis include blurring of vision (generally unilateral) and pain on eye movement. However, patients may also present with nystagmus (uncontrolled rotatory movements of the eye), extraocular muscle paresis manifesting as diplopia, altered colour vision and loss of central vision. Clinical tests assisting in assessment of these patients include visual acuity, checking pupils for relative afferent pupillary defect and assessing the range of extraocular muscle movement. Referral to an ophthalmologist is necessary to exclude other primary ophthalmic causes.
Acute attacks of optic neuritis may be treated with corticosteroids, which have been shown to decrease the duration of the acute attack but do not have an impact on final visual outcome.1
Myasthenia gravis
Myasthenia gravis most commonly presents with visual symptoms such as ptosis, extraocular muscle palsies and double vision, which can be worse with fatigue. Systemic signs include voluntary muscle weakness, dysphagia and dysarthria. Weakness may be limited to the extraocular muscles in about 15% of cases, a subgroup of myasthenia known as ‘ocular myasthenia’.2
Myasthenia gravis is a clinical diagnosis based on history and physical examination. A simple diagnostic test accessible in general practice is the ice-pack test, whereby ptosis is improved by at least 2 mm after a five minute application of ice to the affected lid.
Patients presenting with ptosis, especially acute-onset ptosis, should be examined closely for pupil involvement to exclude Horner’s syndrome or third nerve palsy, which require urgent neuroimaging to exclude neurological dysfunction, whether intracranial or extracranial. Myasthenia gravis never causes unilateral pupillary involvement.
Thyroid orbitopathy
Thyroid orbitopathy can result in a spectrum of ocular disease, from dryness to disfiguring proptosis and lid retraction to restricted eye movements (Figure 1 and Figure 2). The extent of eye disease and thyroid disease do not necessarily correlate and severe eye disease may occur in patients with a normally functioning thyroid.
The most common ocular involvement is dryness and proptosis, which occur in about 50% of patients with thyroid orbitopathy.3 Other ocular signs and symptoms are double vision, conjunctival redness, oedema, lid swelling and pain on eye movements. Inflammation of the extraocular muscles and orbital tissues in the confined space of the bony orbit can result in sight-threatening complications including optic nerve compression and proptosis leading to corneal exposure from incomplete eye closure and inadequate blinking. Urgent investigation with orbital imaging is required if there are signs of optic nerve compression such as decreased vision, reduced visual fields or abnormal pupillary reactions. Imaging is carried out to confirm sight-threatening optic neuropathy due to thyroid orbitopathy. This may facilitate and justify appropriate medical or surgical management.
Symptoms of dry eye are managed with eye lubricants and gels but may require referral for more aggressive management if proptosis causes incomplete lid closure and exposure.
Smoking is an important risk factor for thyroid orbitopathy and is associated with disease progression, poor response to treatment and higher recurrence after treatment. Therefore smoking cessation is an essential part of managing thyroid orbitopathy.4
Ocular rehabilitation in thyroid orbitopathy is aimed at preserving vision through the inflammatory phase, which generally lasts one to two years, and addressing cosmetic issues when the disease has entered the inactive phase.
Systemic lupus erythematosus
Ocular manifestations in systemic lupus erythematosus (SLE) are common and present in 20% of patients with SLE, but these ocular manifestations are not specific to SLE. In a similar manner to how SLE affects many general organ systems, it may also affect any part of the eye from the eyelids to the retina. The most common ocular manifestation of SLE is dry eye, seen in 30% of cases.5 Skin changes to the eyelids, conjunctivitis, episcleritis and scleritis may be due to SLE. Episcleritis presents as episcleral injection, either sectorial or diffuse, that blanches with topical application of 2.5% phenylephrine and is associated with less discomfort than scleritis. Scleritis is rare and is characterised by deep scleral injection that does not blanch with topical 2.5% phenylephrine and a severe, deep orbital pain that often prevents sleep. Scleritis requires urgent referral as it may result in severe visual morbidity including scleral thinning and possibly perforation.
SLE may also affect the retina and optic nerve causing loss of vision. Optic neuropathy is one of the major causes of impaired vision in SLE. Neuro-ophthalmic manifestations due to central nervous system vasculitic changes include visual field changes, lesions of the oculomotor system and cranial nerve palsies. Cranial nerve palsies are generally multiple and rarely isolated, reflecting an ischaemic lesion in the brainstem. Of the isolated oculomotor nerves, abducens nerve (CN VI) lesions are the most common.6
Inflammatory bowel disease
About 10% of patients with inflammatory bowel disease, Crohn’s disease and ulcerative colitis develop ocular involvement.7 These complications are more common in patients with Crohn’s disease, especially when associated with arthralgia.
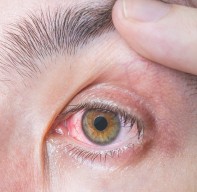
Ocular manifestations are primarily uveitis, episcleritis and scleritis. Uveitis in inflammatory bowel disease is typically anterior. The symptoms of uveitis are red eye, pain, photophobia and blurred vision. Signs include decreased visual acuity, redness and synechiae (adhesions between the iris and the lens) and elevated intraocular pressure. Patients with suspected uveitis require ophthalmological referral for treatment with topical corticosteroids and pupil-dilating agents and may need intraocular pressure-lowering therapy. Episcleritis and scleritis manifest with the same signs and symptoms as described above and summarised in Table 1.
Uveitis may occur during periods of quiescent or active intestinal inflammation and may also precede the diagnosis of inflammatory bowel disease. Episcleritis typically flares during episodes of intestinal flare and may be useful as a marker of disease activity.7
Rheumatoid arthritis
Up to 25% of patients with rheumatoid arthritis (RA) develop ocular involvement ranging from dry eye to corneal ulceration, episcleritis, scleritis and uveitis.8
The most common manifestation is dry eye, or keratoconjunctivitis sicca, which is initially managed with ocular lubricants to increase the tear volume. Nonresponsive, severe dry eye warrants ophthalmology referral for further therapy such as lacrimal drainage occlusion. Other corneal complications include corneal scarring and thinning, which may result in perforation and significant visual morbidity (Figure 3). Episcleritis and scleritis occur in up to 10% of patients with RA and these are differentiated based on appearance and symptoms as described above and summarised in Table 1. Signs and symptoms of uveitis are as described above and summarised in Table 1. Retinal vasculitis and macula oedema are less common complications of RA but must be considered and excluded in patients who present with blurred vision.
Children with juvenile idiopathic arthritis represent a population subset that requires regular screening because the incidence of ocular involvement is high and these patients are often asymptomatic. Incidence of ocular complications is highest in patients with pauciarticular disease, positive antinuclear antibody and a young age of onset. Recommendations for screening are outlined in Table 3.9
Sjögren’s syndrome
Sjögren’s syndrome can occur in isolation or in association with other autoimmune diseases. It has a strong association with RA with up to 25% of patients with RA being affected.8
Sjögren’s syndrome is characterised by dry mucous membranes including those of the eyes and mouth. It is caused by lymphocytic infiltration of the lacrimal gland and the spectrum of ocular dryness can range from mild discomfort to severe dry eyes leading to corneal scarring, ulceration and perforation. Tests useful in the investigation of Sjögren’s syndrome include visual acuity and fluorescein staining. Management includes ocular lubricants and ointment but can require referral for more intensive treatment.
Seronegative spondyloarthropathies
The seronegative spondyloarthropathies, including ankylosing spondylitis, psoriatic arthritis, reactive arthritis and enteropathic arthritis, can be associated with uveitis, which may be recurrent. In patients presenting with uveitis, the signs and symptoms are as described above and summarised in Table 1. Prompt ophthalmological referral is indicated.
Giant cell arteritis
Visual disturbance is the presenting complaint in 25 to 50% of patients with giant cell arteritis (GCA).10 These disturbances include blurred vision, diplopia, transient obscuration of vision (amaurosis fugax), visual field defects and complete loss of vision (unilateral or bilateral). Other symptoms include headache, neck pain, scalp tenderness, jaw claudication and nonspecific symptoms such as weight loss and fever.10
On examination, the findings include tender, thickened dilated superficial temporal arteries (Figure 4). Other signs include visual field defects, swollen optic discs or late optic atrophy with pallor, as well as retinal haemorrhages and cotton wool spots.10
Given that GCA is a condition with devastating consequences – including blindness – it requires urgent investigations including erythrocyte sedimentation rate, C-reactive protein level and full blood count. In patients with high clinical suspicion of disease and elevated inflammatory markers, commencement of high-dose oral corticosteroids such as prednisone (1 mg/kg) to decrease the risk of progression or development of vision loss is recommended.
Patients with suspected GCA should be referred to an ophthalmologist for assessment and temporal artery biopsy, ideally within seven days of commencing corticosteroids. Temporal artery biopsy is an essential part of the diagnosis given that it is the only specific diagnostic test for GCA. Patients with GCA are best managed by a co-operative approach between the rheumatologist, anatomical pathologist and ophthalmologist with the GP playing a vital role in co-ordinating long-term management.
The recent TGA approval of tocilizumab is changing the management of GCA. Tocilizumab – a monoclonal antibody – has been used for other autoimmune conditions for more than eight years and is now largely accepted worldwide as the definitive treatment for GCA, generally in combination with systemic corticosteroids.11
Vasculitis
There are many primary systemic vasculitides in addition to GCA that may affect the eye in various forms.
Granulomatosis with polyangiitis (Wegener’s) affects small arteries and veins with 10% of patients experiencing orbital involvement from extension of inflammation from the adjacent paranasal sinuses, which may lead to proptosis, orbital cellulitis or inflammation of the lacrimal drainage system known as dacryocystitis. Keratitis, scleritis, uveitis and optic nerve involvement may also occur (Table 1).12 Up to 20% of patients with polyarteritis nodosa may have ocular involvement including episcleritis, scleritis and optic nerve involvement (Table 1).12
Medications for autoimmune disease
Medications used in the management of autoimmune disease may also be associated with ocular side effects and guidelines exist for screening regimens. The side effects and recommended screening regimens are outlined in Table 4.
Conclusion
Ocular complications in autoimmune disease are common but these manifestations are not specific to autoimmune disease and require a high level of clinical suspicion by the GP to recognise them. A collaborative approach between the GP and ophthalmologist in the evaluation and treatment of patients with ocular complications of systemic disease is essential to effectively manage these conditions. MT